Is It Possible to Reverse Coronary Artery Disease?
Exploring strategies, treatments, and lifestyle changes to manage and potentially reverse coronary artery disease.
Coronary artery disease (CAD) affects millions worldwide, leading to chest pain, heart attacks, and sometimes death. One of the most common questions patients have is: Can coronary artery disease be reversed? This article explores current research, expert insights, available treatments, and lifestyle changes that may slow, stop, or potentially reverse the progression of CAD.
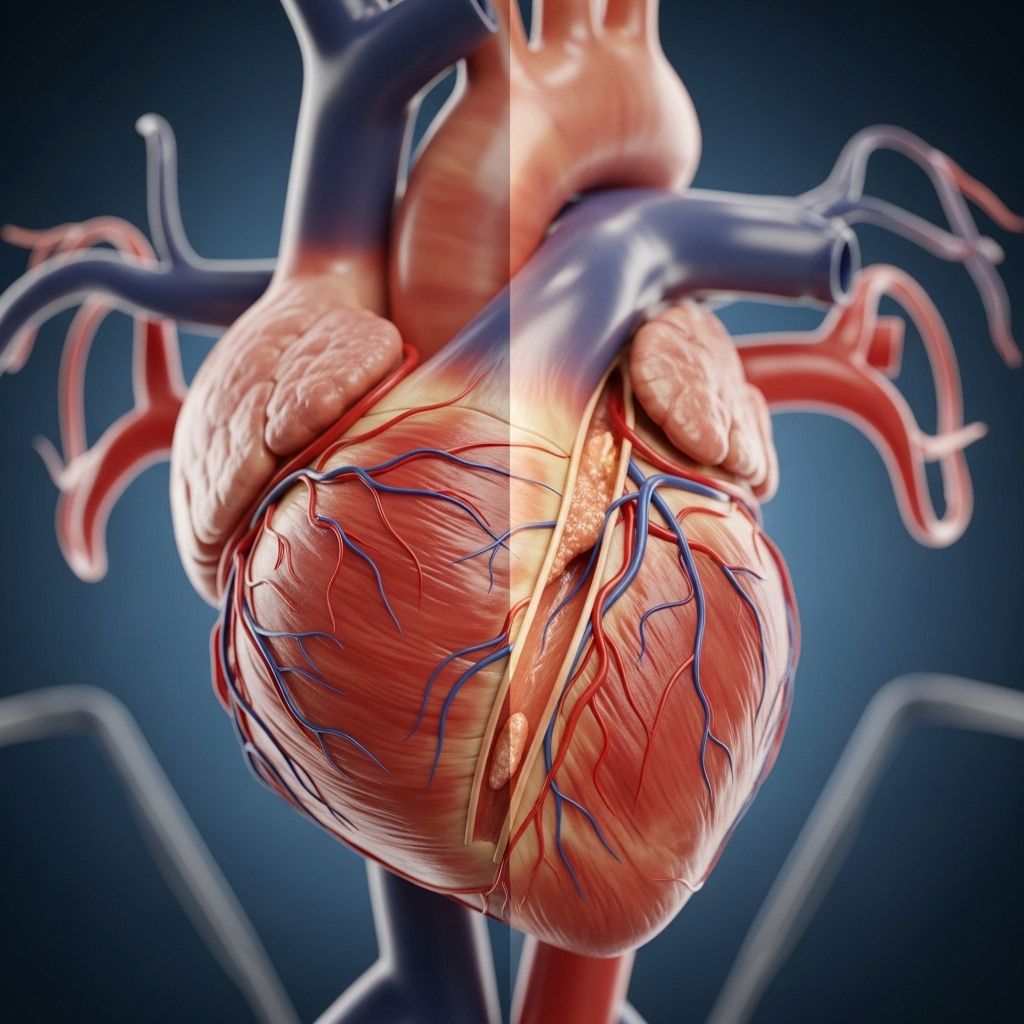
Understanding Coronary Artery Disease
Coronary artery disease is primarily caused by atherosclerosis, the buildup of plaque—a mixture of cholesterol and other substances—on the inner walls of coronary arteries. This buildup restricts blood flow to the heart muscle, resulting in reduced oxygen supply that can trigger symptoms such as chest pain (angina), shortness of breath, heart attacks, or develop silently over decades.
- Key contributors to plaque buildup: High LDL (“bad”) cholesterol, high blood pressure, diabetes, smoking, obesity, and lack of exercise.
- Over time, CAD can weaken the heart muscle, potentially leading to heart failure.
Is Reversing Coronary Artery Disease Possible?
The concept of reversing CAD refers to reducing or even eliminating the atherosclerotic plaque inside the arteries, thereby improving blood flow. While there is no current cure for CAD, studies show that under certain circumstances, some regression of plaque is possible, particularly with aggressive treatment and lifestyle changes.
Key findings from clinical research:
- Severe dietary modification, medication, and lifestyle changes might reduce plaque volume to a small degree.
- Some statin-based trials, such as the ASTEROID trial, showed measurable decreases in arterial plaque in patients who achieved very low LDL cholesterol levels over several years.
- Even with interventions, plaque rarely disappears entirely; the primary medical focus is stabilizing plaque and preventing its growth or rupture—which is the main trigger for heart attacks.
What Does ‘Reverse’ Really Mean?
Generally, when doctors discuss reversal, they mean reducing the size and vulnerability of plaque deposits so that blockages are less likely to cause symptoms or acutely dangerous events like heart attacks. “Reversal” does not typically mean arteries are returned completely to a pre-diseased state, but rather that their function improves and the risk of events drops.
Evidence for Reversal: What Do the Studies Show?
- Autopsy studies from populations exposed to prolonged fasting or famine, such as during World War II, revealed striking reductions in atherosclerosis, suggesting that extreme dietary restriction can reduce plaque.
- The Ornish lifestyle program, relying on a very low-fat vegetarian diet, regular exercise, stress management, and social support, was shown in clinical trials to cause modest regression of plaque compared to standard care.
- Most notably, the ASTEROID Trial demonstrated that patients who achieved very low LDL cholesterol levels on high-dose statins experienced a small reduction in plaque over two years.
Current Medical Approaches: Slowing, Stopping, and Slightly Reversing CAD
While most treatments aim to stabilize and halt CAD progression, a combination of aggressive medication and lifestyle changes can occasionally lead to minor reversal.
Medication Overview
- Statins: Significantly lower LDL cholesterol; high-intensity statins can shrink the volume of plaque modestly, while also stabilizing it to reduce the risk of rupture and major cardiac events.
- Cholesterol absorption inhibitors: These reduce cholesterol absorption from the diet, reinforcing statin effects.
- Antiplatelet drugs (e.g., low-dose aspirin): Help prevent blood clots that could block narrowed arteries, although aspirin is not suitable for everyone due to bleeding risks.
- Beta blockers and ACE inhibitors: Lower blood pressure and heart workload, protecting against further arterial damage.
- Calcium channel blockers and nitrates: Relax blood vessels, reduce chest pain, and improve blood flow to the heart.
- Ranolazine: May be used for people with persistent angina not controlled by other medications.
Procedures and Surgical Interventions
- Percutaneous Coronary Intervention (PCI): Also known as angioplasty, this procedure uses a balloon to open up blocked arteries and typically places a stent to help keep the artery open. PCI primarily relieves symptoms rather than reversing the underlying disease.
- Coronary Artery Bypass Grafting (CABG): Surgeons use blood vessels from other parts of the body to bypass severely narrowed or blocked coronary arteries, improving blood flow. This is generally reserved for patients with extensive or complex blockages.
- Heart transplants may be considered in end-stage cases when heart failure has developed due to extensive CAD damage.
Lifestyle Changes: The Foundation of Heart Health
While medication and surgery address plaques and symptoms, lifestyle changes have a significant impact on preventing, slowing, and possibly modestly reversing CAD.
- Quit smoking: The single most important change for reducing heart disease progression. Tobacco damages arteries and accelerates plaque buildup.
- Adopt a heart-healthy diet:
- Focus on whole grains, fruits, vegetables, beans, nuts, and lean protein sources like fish or poultry.
- Minimize saturated fat, trans fat, and dietary cholesterol.
- Opt for healthy fats such as olive oil and avocado in moderation.
- Limit salt (sodium) intake to help control blood pressure.
- Physical activity: Aim for at least 150 minutes per week of moderate-intensity aerobic exercise (such as brisk walking), plus strength/resistance training two or more days weekly.
- Weight management: Maintaining a healthy body weight reduces risk factors like high blood pressure, diabetes, and unhealthy cholesterol levels.
- Stress management: Chronic stress may worsen CAD risk; techniques like yoga, meditation, or structured group support help lower stress.
- Control blood sugar: Properly managing diabetes or prediabetes is vital for heart health.
- Manage blood pressure and cholesterol through regular check-ups, healthy living, and medication when prescribed.
Preventing Further Progression
Even if complete reversal of CAD is rarely achieved, aggressive risk factor management can prevent new plaque from forming and stabilize existing plaques to protect against heart attack or stroke. Early recognition and action—at any age—offer the best chance for reducing complications.
Key Prevention Strategies
- Don’t smoke and avoid secondhand smoke.
- Eat a diet rich in plant-based foods and low in processed, sugary, or fatty items.
- Keep physically active every day.
- Maintain a healthy weight and waist circumference.
- Take all prescribed medications as directed by your healthcare provider.
- Attend regular medical appointments for monitoring and preventive care.
Frequently Asked Questions (FAQs)
Q: Can coronary artery disease be fully cured?
A: While current science does not yet offer a cure that can remove all plaque from coronary arteries, powerful lifestyle changes and judicious use of medications can stabilize artery health, significantly reduce symptoms, and lower the risk for heart attacks and other events. In some cases, small reductions in plaque volume are possible, but full restoration to normal artery walls is uncommon.
Q: Are there any diets proven to help reverse CAD?
A: Some evidence, including trials of the Ornish diet (plant-based, very low in fat and cholesterol), suggests small regression of plaque is possible with extreme dietary change, intensive exercise, and stress management. For most people, adopting a diet rich in whole plant foods, with limited unhealthy fats, is the safest and most sustainable approach to prevent progression.
Q: What role do statins play in reversing CAD?
A: High-intensity statin therapy can slightly shrink existing plaques over several years, but their biggest benefit comes from stabilizing plaques and reducing the risk of rupture (which causes heart attacks). Patients with significant CAD usually benefit from statins regardless of LDL cholesterol starting level.
Q: If I have angioplasty (PCI) or bypass surgery, does that mean my CAD is gone?
A: No. Procedures like PCI and CABG restore blood flow past blockages and can relieve symptoms like angina, but they do not remove all plaque or stop atherosclerosis elsewhere in your arteries. Ongoing medical therapy and lifestyle change remain essential after procedures.
Q: How can I best monitor my risk of progression or future events?
A: Regular follow-up with your healthcare provider is key. Blood tests for cholesterol, diabetes screening, blood pressure monitoring, and periodic heart imaging (if recommended) help assess risk. Reporting new symptoms and sticking with your prevention plan are vital.
Table: Summary of Medical and Lifestyle Interventions for CAD
| Approach | Goal | Impact on CAD |
|---|---|---|
| High-intensity statins | Reduce LDL cholesterol, stabilize plaque | Small regression of plaque, lower risk of heart attack |
| Diet (low-fat, plant-based) | Lower cholesterol, weight, and inflammation | Possible mild regression, prevents progression |
| Quitting smoking | Reduce arterial damage | Slows or halts progression |
| Exercise | Improve heart strength, circulation, weight control | Prevents worsening, improves symptoms |
| Procedures (PCI/CABG) | Restore blood flow | Symptom relief, not true reversal |
| Blood pressure management | Minimize arterial stress | Prevents new plaque formation |
Takeaway
For most, reversal of coronary artery disease means halting or modestly regressing plaque buildup using an all-hands approach: optimal medications, major lifestyle changes (including diet and exercise), and preventive care. Even if arteries are not returned to perfect health, these steps dramatically reduce the risk of heart attacks, strokes, and other life-threatening events associated with CAD.
The journey to better heart health is lifelong; work closely with your doctors, tailor your strategy to your needs, and make heart-healthy choices every day.
References
- https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/diagnosis-treatment/drc-20350619
- https://www.medicalnewstoday.com/articles/how-to-reverse-coronary-artery-disease
- https://www.health.harvard.edu/heart-health/ask_the_doctor_is_it_possible_to_reverse_coronary_artery_disease
- https://www.webmd.com/heart-disease/features/can-you-reverse-coronary-artery-disease
- https://heart.arizona.edu/heart-health/prevention/10-things-you-can-do-today-preventreverse-heart-disease
- https://www.nhlbi.nih.gov/health/atherosclerosis/treatment
Read full bio of Sneha Tete












