Retinal Tears: Causes, Symptoms, Treatments, and Prevention
Understand the risk factors, symptoms, diagnosis, and treatment options for retinal tears—early action is key for preventing vision loss.
Retinal tears are critical eye conditions that can lead to significant vision loss if not treated promptly. This article will explore what a retinal tear is, what causes it, its symptoms, how it’s diagnosed and treated, and what you can do to prevent severe complications like retinal detachment. Understanding retinal tears is essential for maintaining lifelong eye health and acting quickly in the event of sudden vision changes.
What Is a Retinal Tear?
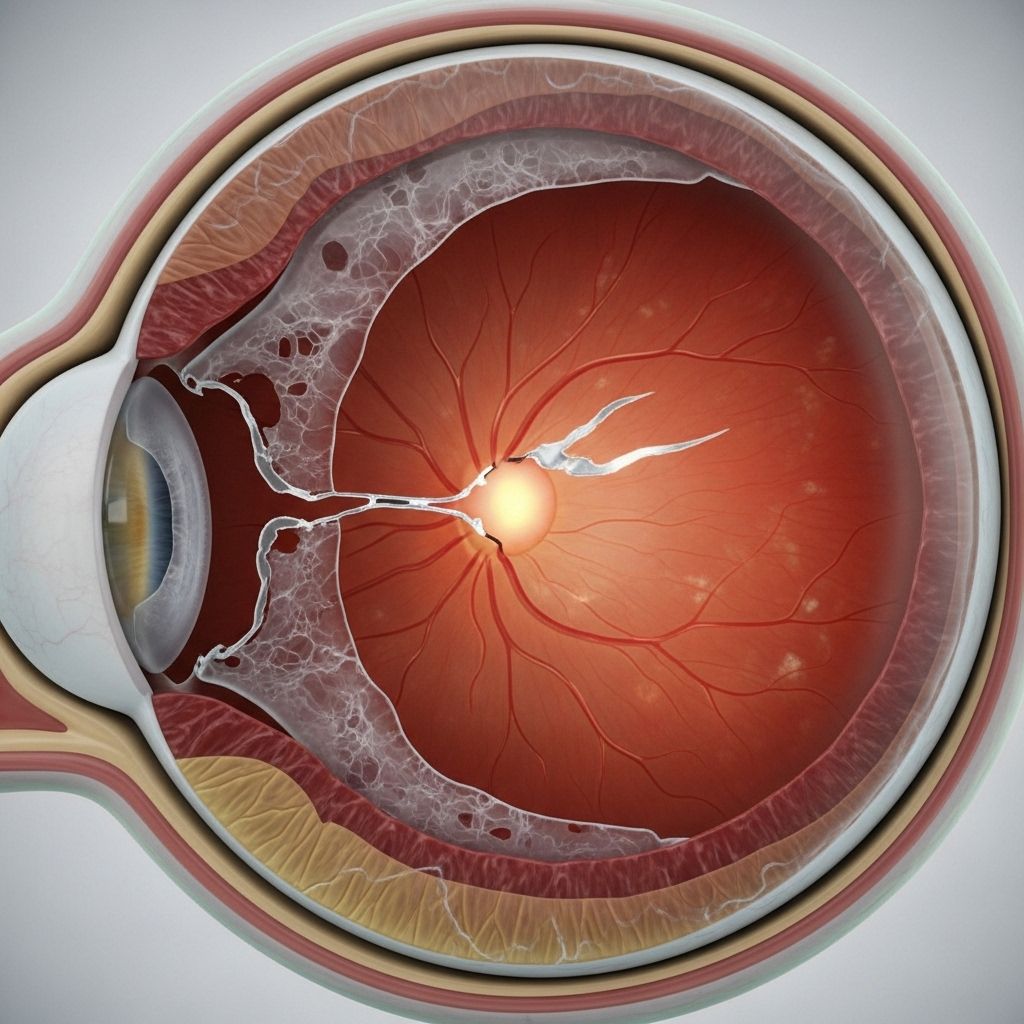
The retina is a thin, light-sensitive layer of tissue lining the back of your eye. It is responsible for converting light into visual signals sent to your brain, making vision possible. A retinal tear occurs when a small break develops in this delicate tissue. While some tears remain stable, many can progress, allowing fluid from the eye to seep underneath the retina and causing a potentially blinding condition called retinal detachment.
- Retinal tears often develop suddenly, especially in people at higher risk due to age, previous eye surgery, or trauma.
- Not all retinal tears cause immediate symptoms, but rapid identification is vital to prevent complications.
Symptoms of a Retinal Tear
Recognizing the warning signs of a retinal tear can be vision-saving. While many symptoms overlap with those of retinal detachment, a few specific features can indicate a tear has occurred:
- Sudden appearance of floaters: Tiny black spots or cobweb-like shapes drifting in your field of vision.
- Flashing lights (photopsia): Brief bursts of light, often at the eye’s periphery, described as seeing stars.
- Shadow in the peripheral vision: A blurry edge or shadow that may spread across your side (peripheral) vision.
- Gray curtain or veil effect: A sensation of a curtain or shade descending over part of your visual field.
- Less commonly, blurred vision or decreased clarity, especially if bleeding occurs within the eye.
Importantly, retinal tears usually do not cause pain. Some tears have no noticeable symptoms, making regular eye exams crucial—especially if you are at higher risk.
When to Seek Immediate Medical Attention
- The sudden onset of new floaters or flashes
- Dark areas, shadows, or curtains over your vision
- Sudden, significant loss of vision in one eye
These can indicate a retinal tear or detachment, both of which require urgent medical care.
Causes of Retinal Tears
Retinal tears result from both internal changes within the eye and external traumatic events. The most frequent causes and risk factors include:
Posterior Vitreous Detachment (PVD)
The most common cause of retinal tears is a phenomenon called posterior vitreous detachment (PVD). The eye’s center contains a clear, gel-like substance called vitreous. As people age, the vitreous naturally shrinks and pulls away from the retina. While this usually happens harmlessly, in some individuals the vitreous is unusually adherent to the retinal surface. As it separates, it can tug on the retina and generate a tear.
Other Causes
- Eye trauma: Accidents or injuries that strike the eye can cause tears in the retina.
- Eye surgery complications: Certain procedures, such as cataract surgery, may raise the risk of developing retinal tears later on.
- Extreme nearsightedness (myopia): Thinner retinas in very nearsighted people can make tears more likely.
- Genetics and family history: A family history of retinal tears or detachment can increase your risk.
- Previous retinal tears or detachment: Developing a tear or detachment in one eye raises the risk in the other eye.
- Lattice degeneration: Thinning or weakness in the retina’s periphery can predispose certain people to tearing.
Risk Factors for Retinal Tears
Certain groups are more susceptible to retinal tears:
- Aging: Risk increases with age, especially over 50.
- High myopia (nearsightedness): Severe nearsightedness stretches and thins the retina.
- Prior eye surgery: Including cataract or previous retinal procedures.
- Blunt or penetrating eye trauma: Sports injuries, accidents, or physical assault.
- Family history: Genetic predisposition for retinal problems.
- Retinal disorders: Conditions like lattice degeneration weaken retinal tissue.
How Are Retinal Tears Diagnosed?
Diagnosis of a retinal tear involves prompt, thorough examination by an eye care specialist known as an ophthalmologist. The diagnostic process may include:
- Dilated eye exam: Your doctor uses eye drops to widen (dilate) your pupils, then examines the retina closely with special lights and lenses.
- Ophthalmoscopy: Direct visualization of the retina to assess for tears, holes, and potential detachment.
- Optical coherence tomography (OCT): High-resolution imaging to detect subtle tears or retinal thinning.
- Ultrasound imaging: Used when blood in the eye (vitreous hemorrhage) obscures the view of the retina.
Early diagnosis is crucial. If you develop sudden symptoms, do not delay seeking medical care; outcomes are best if treated quickly.
Potential Complications: Retinal Detachment
The greatest threat posed by an untreated retinal tear is the risk of retinal detachment. In this condition, fluid seeps through the tear and lifts the retinal tissue away from the underlying blood supply. Retinal detachment is a medical emergency that can lead to rapid, permanent vision loss if not treated promptly.
Symptoms Indicating Progression to Detachment
- A curtain or shadow rapidly spreading across vision
- Sudden, dramatic decrease in vision
Treatment within a matter of hours or days is often necessary to save vision in cases of detachment.
Treatment Options for Retinal Tears
Not every retinal tear needs immediate intervention, but most tears with symptoms or a high risk of detachment are treated promptly. The main goals are to seal the tear, prevent progression, and protect sight. The most common treatments include:
Laser Photocoagulation
- A focused laser is used to burn small spots around the retinal tear, creating scar tissue that effectively “welds” the retina in place and prevents fluid from entering underneath.
- This outpatient procedure is quick and usually painless. Recovery is often rapid.
Cryopexy (Freezing Therapy)
- This technique utilizes a super-cooled probe, applied to the outside surface of the eye, to freeze the area surrounding the retinal tear.
- The resulting scarring secures the retina to the tissue underneath, preventing detachment.
Vitrectomy Surgery
- Reserved for more complex situations or when a tear has already led to detachment.
- Involves removing the vitreous gel and replacing it with a substitute, followed by repair of the retina.
Observation
- Some very minor tears, particularly those without symptoms and at low risk for detachment, may be monitored closely without immediate treatment.
Can Retinal Tears Heal on Their Own?
Small, asymptomatic retinal tears may sometimes stabilize without surgery, but specialists caution against relying on natural healing. Untreated tears still carry the risk of progressing to detachment, so prompt evaluation is always advised.
Recovery After Treatment
Recovery depends on the type of treatment performed and the severity of the tear. Most people experience a quick recovery from outpatient laser or cryopexy procedures, with minimal discomfort and little downtime. It is important to follow your doctor’s advice on activity restrictions and attend all follow-up appointments.
- Vision may improve if the tear is treated early.
- Early intervention often prevents further complications and preserves sight.
- Some people may notice persistent floaters or slight visual changes following treatment, but these often diminish over time.
Preventing Retinal Tears and Their Complications
While not all retinal tears can be prevented, you can take steps to reduce your risk and ensure early detection:
- Have regular, comprehensive eye exams, especially after age 50 or if you are at higher risk.
- Seek immediate medical care if you experience new floaters, flashes, or visual shadows.
- Protect eyes from traumatic injury by using safety glasses during sports or hazardous activities.
- Inform your eye doctor if you’ve had previous retinal problems or family history of retinal detachment.
Early detection and treatment are the best strategies for preserving your vision.
Frequently Asked Questions (FAQs)
What is the difference between a retinal tear and a retinal detachment?
A retinal tear is a break or hole in the retina, while a retinal detachment is when the retina lifts away from the underlying tissue, often through a tear. Both are medical emergencies, but detachment poses a more immediate threat to vision.
Can you cure a retinal tear?
Most retinal tears can be effectively treated—often cured—using laser photocoagulation or cryopexy if caught early. The main purpose is to prevent detachment and preserve vision.
How serious is a retinal tear?
Retinal tears should be taken very seriously. Without prompt treatment, they can lead to retinal detachment, which may cause permanent vision loss.
Are retinal tears painful?
No, retinal tears typically do not cause pain. The most common symptoms are visual changes like floaters and flashes.
Can retinal tears heal naturally without treatment?
Some small tears may stabilize on their own, but because all tears carry a risk of progressing to detachment, medical evaluation is crucial. Prompt treatment dramatically reduces the odds of permanent vision loss.
What should I do if I notice symptoms of a retinal tear?
Contact an eye care professional or go to the emergency room immediately. Early intervention is the key to preserving sight.
Key Takeaways
- Retinal tears are not painful but can lead to sudden vision changes and, if untreated, irreversible vision loss.
- Prompt diagnosis and treatment—usually with laser or freezing therapies—are highly effective.
- Regular eye exams and attention to visual symptoms are crucial for prevention and early detection.
- If you ever notice a sudden increase in floaters, flashes of light, or vision loss, seek medical care immediately.
References
- https://www.asrs.org/patients/retinal-diseases/26/retinal-tears
- https://www.healthline.com/health/eye-health/retinal-tear-vs-detachment
- https://www.medicalnewstoday.com/articles/retinal-tear-causes
- https://www.medicalnewstoday.com/articles/retinal-tear-treatment
- https://www.asrs.org/content/documents/fact-sheet-23-lp-retinal-tears-2020_1_asrs.pdf
- https://my.clevelandclinic.org/health/diseases/25107-retinal-tear
- https://specialty.vision/article/understanding-retinal-tears-symptoms-treatment-risks/
Read full bio of Sneha Tete












