Retinal Tear vs. Retinal Detachment: Recognizing Symptoms, Causes, and Treatments
Learn how to spot the signs, understand the risks, and act quickly to protect your vision from retinal tears and detachments.
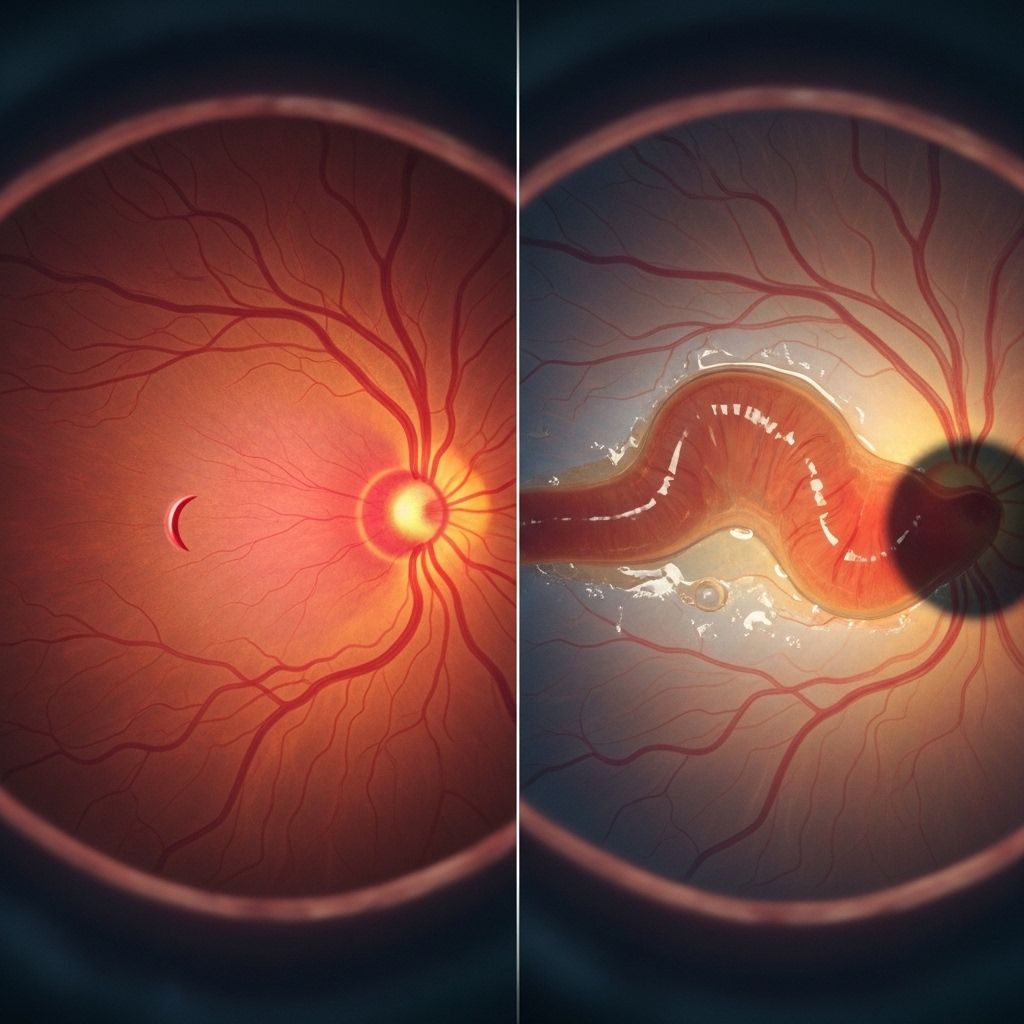
Retinal Tear vs. Retinal Detachment: What’s the Difference?
The retina is a delicate layer of tissue at the back of the eye, responsible for capturing light and sending visual signals to the brain. Retinal tears and retinal detachments are two distinct but closely related ocular conditions that threaten this vital tissue and can put vision at risk. While both require immediate medical attention, their causes, symptoms, and treatments each have unique aspects that eye health patients and caregivers should understand.
What Is a Retinal Tear?
Retinal tear refers to a hole or rip in the retina. This condition occurs when the retina is torn but remains largely attached to the back wall of the eye. Although less severe than a detachment, a retinal tear can quickly escalate if not managed properly.
- Caused when the vitreous gel inside the eye pulls on the retina, creating a break or opening.
- Tears can sometimes heal on their own, but often need treatment to prevent progression.
- Retinal tears are considered emergencies because they can lead to detachment and vision loss.
What Is Retinal Detachment?
Retinal detachment is a sight-threatening condition where the retina separates from its underlying tissue. When this happens, the retina is unable to function properly, resulting in loss of vision that can become permanent without urgent treatment.
- Frequently develops after a retinal tear allows fluid to seep behind the retina, lifting it away from the back of the eye.
- Detachment disrupts blood supply and can lead to irreversible vision loss if not corrected quickly.
- Always considered a medical emergency.
How Are Retinal Tears and Detachments Related?
Retinal detachment often begins as a retinal tear. When the vitreous humor (the eye’s gel-like filling) shrinks or changes with age, it may tug on the retina, creating a tear. If fluid seeps through this tear, it can build up behind the retina, lifting it off the underlying tissue—a process known as detachment.
However, not every tear leads to detachment, and not every detachment is preceded by a tear. Some retinal detachments arise from other causes such as scarring or abnormal fluid accumulation.
Types of Retinal Detachment
| Type | Description | Common Causes |
|---|---|---|
| Rhegmatogenous | Most common type. A tear or break allows fluid to get under the retina, separating it from underlying tissue. | Aging, posterior vitreous detachment, trauma |
| Tractional | Scar tissue on retina surface pulls it away from the back of the eye. | Diabetic retinopathy (common), other eye diseases with scarring |
| Exudative | Fluid accumulates under the retina without a tear or break. | Inflammatory disorders, injury, vascular abnormalities |
Symptoms of Retinal Tears and Detachments
The symptoms of retinal tears and detachments can be similar and are often sudden. Recognizing these warning signs is critical:
- Floaters: Small specks, dots, or lines drifting across your field of vision.
- Flashes of light: Brief, sudden flashes, often in the peripheral vision.
- Blurred vision: Loss of visual clarity or sharpness.
- Dark spots: Black or gray areas blocking vision.
- Shadow or curtain: A shadow or curtain effect spreading across the field of vision from the top, bottom, or sides.
- Peripheral vision loss: Difficulty seeing to the sides.
Retinal tears and detachments are not painful, but their symptoms indicate an eye emergency and should prompt immediate medical evaluation.
What Causes Retinal Tears and Detachments?
Several processes can lead to retinal tears or detachment. The most common are linked to the aging process:
- Posterior vitreous detachment (PVD): The vitreous humor shrinks and becomes less gel-like with age, eventually pulling away from the retina. This process can tug the retina, causing a tear.
- Injury or trauma: Blunt force to the eye or head may create a retinal tear or detachment.
- Scar tissue: Scarring from diabetic eye disease or other retinal disorders may pull the retina away (tractional detachment).
- Fluid accumulation: Leaky blood vessels or inflammation can create fluid buildup under the retina (exudative detachment).
Risk Factors
- Age (over 50 is highest risk)
- Personal or family history of retinal detachment
- Severe nearsightedness (myopia)
- Previous eye surgery, such as cataract removal
- Significant eye injury or trauma
- Eye diseases, such as diabetic retinopathy or lattice degeneration
Diagnosis: How Are Retinal Tears and Detachments Identified?
Early diagnosis dramatically improves outcomes:
- Comprehensive eye exam: An ophthalmologist will evaluate symptoms and use dilating eye drops to fully view the retina.
- Ophthalmoscopy: Special lenses and lights help inspect the retina for tears, holes, or areas of detachment.
- Imaging: In some cases, ultrasound or optical coherence tomography (OCT) can provide detailed views if the retina is obscured by bleeding or swelling.
Immediate detection is essential, as prompt intervention can often preserve vision.
Treatment Options for Retinal Tears and Retinal Detachments
The urgency and approach depend on whether only a tear is present or detachment has occurred.
Retinal Tear Treatment
- Laser Therapy (Photocoagulation): A laser is used to create tiny burns around the tear, forming scar tissue that “seals” the retina in place and prevents detachment.
- Cryotherapy (Freezing Treatment): Cold temperatures are applied with a probe to freeze the area around the tear, promoting a scar that secures the retina to the eye wall.
Both treatments are office procedures and typically require only local anesthesia.
Retinal Detachment Treatment
- Pneumatic Retinopexy: A gas bubble is injected into the eye. The bubble presses the retina back into place, while laser or cryotherapy seals the tear. The patient must maintain a specific head position for several days.
- Scleral Buckling: A flexible band (buckle) is placed around the eye’s exterior, gently pushing the eye wall against the detached retina. This method may be combined with laser or cryotherapy.
- Vitrectomy: The vitreous gel is surgically removed and replaced (often with a gas bubble or silicone oil), letting the retina return to its normal position. Laser or cryotherapy repairs the tear during surgery.
Treatment choice depends on the detachment’s type, size, and location. Some patients need more than one method for complete repair.
Recovery and Outlook
- Early intervention is crucial for visual recovery. Retinal tear treatments have a high success rate if applied before detachment occurs.
- After retinal detachment surgery, most people regain some vision. However, the degree depends on how long the retina was detached and whether the macula (central vision area) was involved.
- Multiple surgeries may be necessary in complex cases.
- Follow all post-procedure care instructions carefully for best results.
Potential Complications
- Partial or total vision loss: If untreated, detachment may cause irreversible blindness.
- Re-detachment: The retina can re-tear or detach again, requiring further intervention.
- Infection or bleeding: Rare but possible after surgery or procedures.
- Cataract formation: Lens clouding can sometimes develop after surgical repair.
When to Seek Medical Care
If you experience any new visual symptoms, contact an eye doctor or go to an emergency room immediately. Key red flags include:
- Sudden increase in floaters
- Flashing lights
- A shadow or curtain spreading across your vision
- Noticeable vision loss or blurring
Immediate medical attention can make the difference between restored sight and permanent loss.
Prevention Tips: Protecting Your Vision
- Regular comprehensive eye exams, especially if you are over age 50, highly nearsighted, or have known risk factors.
- Report any sudden vision changes to a medical professional promptly.
- Protect your eyes from trauma with safety eyewear during sports or hazardous activities.
- Manage chronic health conditions, such as diabetes, to reduce risk.
Frequently Asked Questions (FAQs)
Q: Can a retinal tear heal on its own?
A retinal tear often does not heal by itself and may progress to detachment if left untreated. Rapid intervention with laser or freezing therapy is critical to prevent vision loss.
Q: Is retinal detachment always painful?
Neither retinal tears nor detachments cause pain, but their visual changes should be considered an emergency.
Q: What is the difference between retinal tear and detachment symptoms?
Both present with floaters, flashes, and shadows in vision. Detachment may create a larger “curtain” effect or more severe loss of vision, but initial symptoms overlap.
Q: Am I at risk if I have a family history of retinal detachment?
Yes, a family history increases your risk. Regular eye checks and paying attention to symptoms are especially important if you have relatives who experienced detachment.
Q: How fast does a tear progress to detachment?
The timeline varies greatly. A tear can progress rapidly to detachment or remain stable for years; immediate evaluation after new symptoms is always advised.
Summary
Retinal tears and detachments are medical emergencies requiring immediate attention. Recognize the symptoms—floaters, flashes, shadows, and vision loss—and act urgently to prevent irreversible blindness. With early detection and treatment, vision can often be preserved.
References
- https://resources.healthgrades.com/right-care/eye-health/retinal-tear-vs-detachment
- https://www.medicalnewstoday.com/articles/retinal-tear-vs-detachment
- https://www.retinaconsultantsofamerica.com/blog/understanding-the-difference-retinal-tears-vs-retinal-detachments
- https://www.medicalvision.com/retinal-tear/
- https://www.healthline.com/health/eye-health/retinal-tear
- http://www.kadrmaseyecare.com/eye-health–care-blog/retinal-tear-vs-detachment-how-do-they-differ
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9834476/
- https://www.texaschildrens.org/content/conditions/retinal-detachment
Read full bio of Sneha Tete












