Retinal Tear vs. Retinal Detachment: Key Differences, Symptoms, and Treatments
Learn the differences between retinal tears and detachments, their causes, signs, and urgent treatment options to safeguard your vision.
Retinal Tear vs. Retinal Detachment: Understanding the Differences, Risks, and Treatments
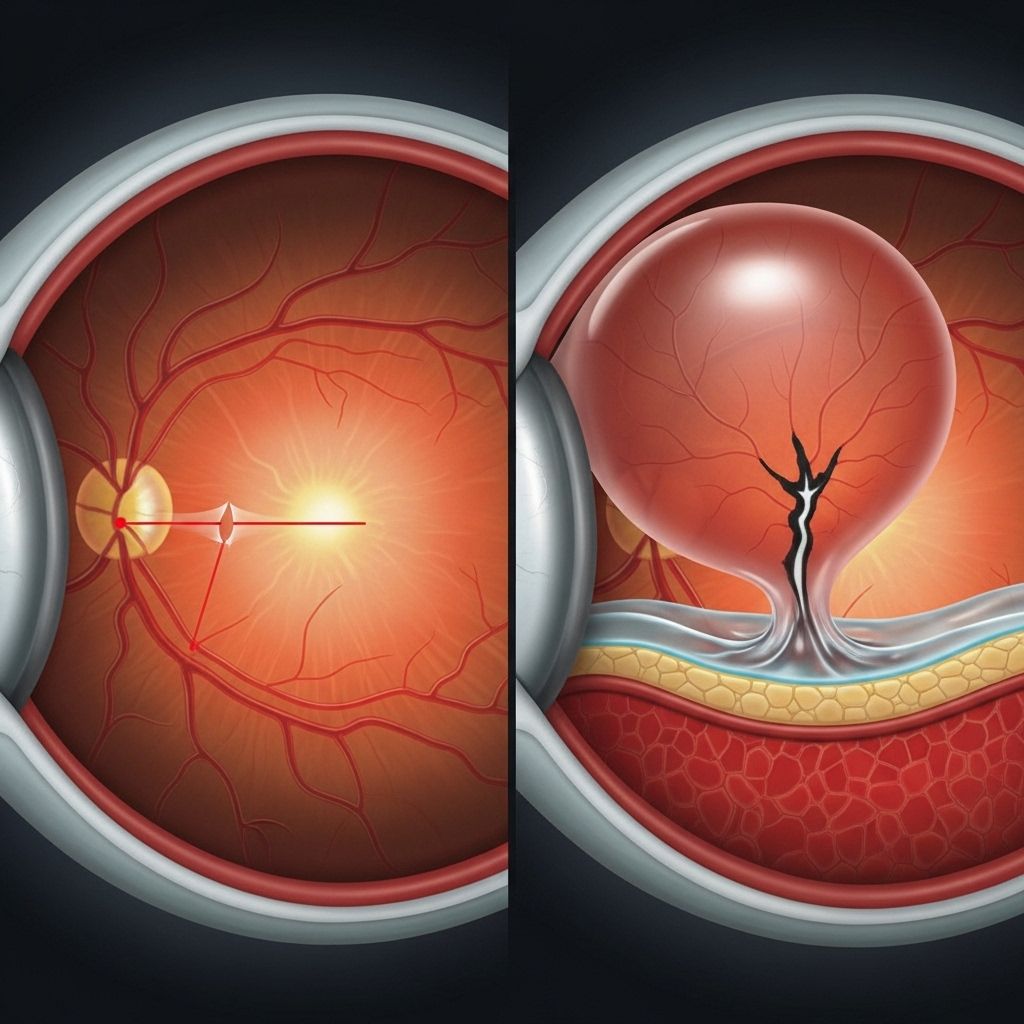
Your retina is a thin, light-sensitive tissue lining the inside back wall of your eye. This essential part of your vision system can suffer serious conditions such as retinal tears and retinal detachments, which are both medical emergencies capable of causing permanent vision loss if untreated. While these two problems are related, they are distinct in how they affect the retina and differ in severity, causes, symptoms, and treatment options.
What Is the Difference Between a Retinal Tear and a Retinal Detachment?
Retinal tear is a condition where a hole or rip appears in the retina, often caused by age-related changes or injury.
Retinal detachment is when the retina is lifted or pulled completely away from its underlying layer of support tissue inside the eye. Without quick treatment, detachment can result in permanent loss of vision.
| Feature | Retinal Tear | Retinal Detachment |
|---|---|---|
| Definition | A hole or rip in the retina | Retina separates from the back of the eye |
| Severity | Less severe (if treated quickly) | More severe; can cause permanent vision loss |
| Common Progression | May lead to detachment if untreated | May result from untreated tears/other causes |
| Emergency? | Yes | Yes (more urgent) |
How Are Retinal Tears Related to Retinal Detachment?
Retinal tears can be a precursor to detachment. When a tear develops, vitreous fluid in the eye can seep behind the retina through the tear, gradually lifting it off and causing a detachment. However, not all retinal detachments start with a tear; there are other causes as well.
Types of Retinal Detachment
There are three main types of retinal detachment, each with different causes and characteristics:
- Rhegmatogenous retinal detachment: The most common type, occurs when a tear or hole in the retina allows fluid to pass through, separating it from the underlying tissue.
- Tractional retinal detachment: Caused by scar tissue (often from diabetic retinopathy) pulling the retina off the back of the eye.
- Exudative retinal detachment: Develops when fluid builds up behind the retina without a tear or hole, often due to inflammation, injury, or vascular problems.
Symptoms of Retinal Tears and Detachments
Retinal tears and detachments can cause similar symptoms—both are often painless but result in visual disturbances. Acting quickly if you experience any of these signs is crucial because timely treatment can save your vision.
- Sudden appearance of floaters (tiny shapes, lines, or cobwebs drifting in your field of vision)
- Flashes of light in one or both eyes, especially in the outer periphery
- Blurred vision without clear cause
- Dark or shadowy areas appearing across your vision, like a curtain coming down
- Loss of peripheral (side) vision
- In some cases: overall dimming or darkening of your vision
It’s important to highlight that neither condition causes pain—symptoms are related to changes in what you see, not what you feel.
Can a Retinal Tear Lead to Retinal Detachment?
Yes. A retinal tear can allow fluid to pass through and accumulate behind the retina, which often results in progressive detachment. The timeline for this progression varies—sometimes occurring within hours, sometimes taking weeks. Immediate medical assessment and treatment are critical to prevent detachment and preserve vision.
Causes and Risk Factors
Understanding what increases your risk for retinal tears and detachments can help you act early. Several factors are known to contribute:
- Aging: Age-related changes make retinal tears more common after age 50, largely due to thinning and shrinking of the jelly-like vitreous fluid in the eye.
- Posterior vitreous detachment (PVD): As you age, the vitreous may shrink and tug on the retina, causing a tear.
- Severe nearsightedness (myopia): Increases risk due to abnormal eye shape and stretching of the retina.
- Eye injuries or trauma: Blunt force or penetrating injuries to the eye can cause tears or detachments.
- Previous eye surgery: Operations such as cataract removal can elevate risk.
- Family or personal history: Genetic factors can play a role.
- Diabetic retinopathy: Scar tissue from diabetes can pull the retina (tractional detachment).
- Lattice degeneration: Thinned, weakened areas of retina susceptible to breakage.
Anyone with these risk factors should be especially alert to sudden vision changes.
How Are Retinal Tears and Detachments Diagnosed?
If you experience symptoms, a prompt, comprehensive eye exam is essential. Diagnosis typically involves:
- Ophthalmoscopy: The eye doctor dilates (widens) your pupils with special drops to carefully examine the retina for tears or areas of detachment.
- Ocular imaging: Additional tests, such as ultrasound or specialized retinal imaging, may be used if the view is obscured by bleeding or cloudiness.
Early diagnosis is vital—smaller tears are easier to treat and less likely to cause permanent vision loss.
Treatment Options for Retinal Tears and Retinal Detachment
Retinal Tear Treatment
Treatment for a retinal tear aims to seal the break and prevent fluid from passing through, which could otherwise cause a detachment. The two most common treatments are:
- Laser photocoagulation: A laser creates small burns around the tear, forming scar tissue that seals the edges and prevents fluid passage.
- Cryopexy (freezing treatment): A freezing probe applied to the outside of the eye creates a scar to seal the tear.
Both procedures are typically performed in the doctor’s office and are quick with minimal discomfort. Recovery is generally rapid, with vision usually preserved if completed before detachment occurs.
Retinal Detachment Treatment
When detachment occurs, more significant intervention is required—often surgical. Common procedures include:
- Pneumatic retinopexy: The doctor injects a gas bubble into the vitreous; this bubble presses the retina onto the wall of the eye. Laser or cryotherapy is then used to seal the tear. Patients must position themselves to keep the bubble in place for several days.
- Scleral buckle: A flexible band is permanently placed around the outside of the eye, counteracting the pulling forces of the vitreous and holding the retina in position.
- Vitrectomy: The vitreous gel is removed and replaced with saline, gas, or silicone oil. This allows the doctor to directly repair the retina and address any scarring or bleeding.
In some cases, more than one technique may be needed for full retinal reattachment. Surgery is often urgent and outcomes are better with earlier intervention.
What Is the Outlook for Retinal Tears and Detachment?
Retinal tears, if treated promptly, usually heal well with minimal vision loss. The risk of progression to detachment is greatly reduced when medical attention is urgent. Retinal detachment is a more serious emergency: without treatment, it often leads to permanent vision impairment or blindness. Even with treatment, some vision loss may persist, especially if the macula (the area responsible for central vision) is affected.
- Early diagnosis and intervention are the keys to the best outcomes.
- Regular eye exams, particularly in those at higher risk, can detect problems before irreversible damage occurs.
Frequently Asked Questions (FAQs)
What are the earliest symptoms of a retinal tear or detachment?
The first symptoms are usually sudden flashes of light and an increased number of floaters in your vision. A sudden shadow, dimming, or ‘curtain’ across your field of vision is also a red flag. These signs require immediate attention from an eye doctor.
Is either condition painful?
No. Both retinal tears and detachments are painless. This makes it important not to ignore changes in your vision, even in the absence of discomfort.
Can retinal detachment be prevented?
While not all cases are preventable, regular eye exams and prompt treatment of retinal tears (with laser or cryotherapy) can help prevent many cases of detachment. Managing underlying risks, such as diabetes and avoiding eye injuries, further reduces your risk.
How quickly should someone seek care for symptoms?
Anyone experiencing the described symptoms should see an ophthalmologist or go to the nearest emergency department immediately. Vision can often be saved or restored if care is prompt.
What is the prognosis after retinal detachment surgery?
If treated early, significant vision recovery is possible, but outcomes depend on severity and whether the central retina (macula) was detached. Some people may have lingering vision changes or require additional interventions.
When to See a Doctor
Do not delay seeking medical attention if you notice new floaters, flashes of light, sudden blurred vision, or a dark curtain over your sight. Early recognition and treatment of these signs can save your vision.
- If you are unsure about the cause of your symptoms or if you need care, call your eye doctor or the nearest emergency medical service for advice.
- Prompt action can mean the difference between full recovery and permanent sight loss.
Tips for Protecting Eye Health
- Attend regular comprehensive dilated eye exams, especially if you are over age 50 or have risk factors.
- Seek prompt treatment for any new vision symptoms.
- Protect eyes from injury with appropriate safety gear for sports or work.
- Manage chronic conditions like diabetes that increase your risk.
- Know your family eye health history and inform your eye doctor.
Additional Resources
- American Academy of Ophthalmology
- National Eye Institute
- Foundation Fighting Blindness
References
- https://resources.healthgrades.com/right-care/eye-health/retinal-tear-vs-detachment
- https://www.medicalnewstoday.com/articles/retinal-tear-vs-detachment
- https://www.retinaconsultantsofamerica.com/blog/understanding-the-difference-retinal-tears-vs-retinal-detachments
- https://www.medicalvision.com/retinal-tear/
- https://www.healthline.com/health/eye-health/retinal-tear
- http://www.kadrmaseyecare.com/eye-health–care-blog/retinal-tear-vs-detachment-how-do-they-differ
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9834476/
- https://www.texaschildrens.org/content/conditions/retinal-detachment
Read full bio of Sneha Tete












