Retinal Tear: Causes, Symptoms, Treatment, and Prevention
Retinal tears are a potentially vision-threatening condition requiring prompt diagnosis and effective treatment to prevent permanent sight loss.
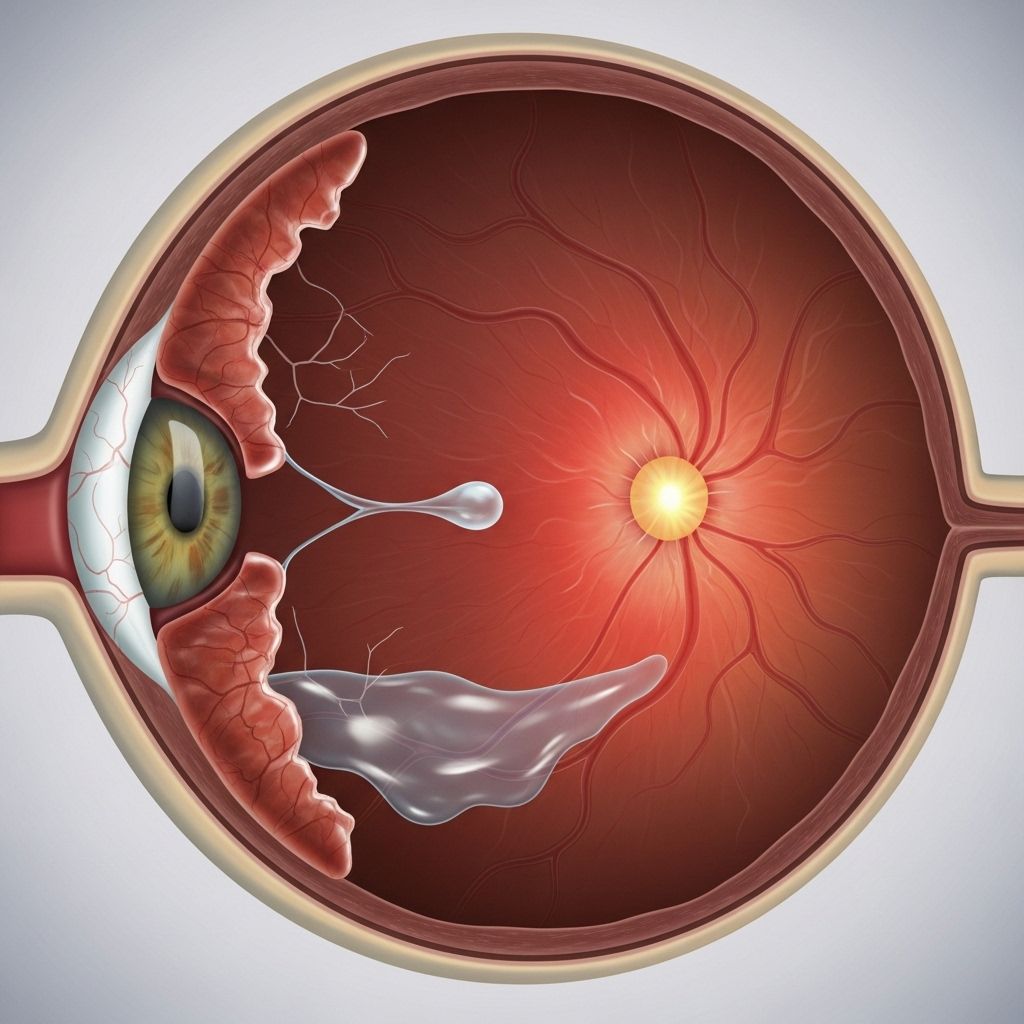
The retina is a thin, light-sensitive tissue lining the back of the eye that is crucial to vision. A retinal tear occurs when this delicate membrane develops a break, which can threaten your sight and, if untreated, may lead to retinal detachment—a medical emergency requiring swift action. This article provides a comprehensive look at retinal tears, including their causes, symptoms, risk factors, diagnosis, treatment, recovery, and prevention strategies.
What is a Retinal Tear?
A retinal tear is a breach in the layer of light-detecting cells at the back of the eye. This break can allow fluid to seep behind the retina, increasing the risk of retinal detachment—a far more serious condition in which the retina separates from its supporting tissues. Retinal tears do not cause pain, so recognizing visual symptoms is vital to avoiding permanent vision loss.
Symptoms of a Retinal Tear
Recognizing the symptoms of a retinal tear is essential as the condition is generally painless, and prompt medical attention can make the difference in preserving vision. Common symptoms include:
- Flashing lights (photopsia): Sudden flashes or shimmering lights, sometimes described as ‘seeing stars,’ especially when moving your eyes or in dark environments.
- Floaters: New onset of black spots, specks, or cobweb-like shapes drifting in your field of vision. These can appear suddenly and may multiply quickly.
- Shadows in peripheral vision: Partial darkening or shadows at the edge of your visual field, which can progress to cover larger areas.
- Gray curtain over vision: A sensation like a veil or curtain moving across part of your visual field, indicating that a more extensive portion of the retina is affected.
- Blurred or distorted vision: In some cases, vision may become cloudy or distorted, especially if a vitreous hemorrhage or retinal detachment occurs.
Some retinal tears remain asymptomatic, meaning individuals may not notice any changes until complications arise. Early intervention is crucial to prevent progression to retinal detachment.
Causes and Risk Factors
Several factors can lead to the development of a retinal tear. Understanding these causes can help individuals identify those at increased risk and encourage proactive eye health management:
Primary Causes
- Posterior Vitreous Detachment (PVD): With age, the gel-like substance called vitreous in the eye begins to separate from the retina. In most cases, this process occurs without incident. However, in individuals with a more ‘sticky’ vitreous, abnormal adhesion can pull on the retina, causing a tear. PVD is the single most common cause of retinal tears.
- Eye Trauma: Direct injury or blunt force to the eye can mechanically rupture the retina, often creating tears and increasing the risk for detachment.
- Eye Surgery: Procedures such as cataract surgery or other intraocular operations may disrupt the vitreoretinal interface, raising the chances of post-surgical retinal tears.
- Progressive Retinal Thinning: Some individuals develop retinal holes due to thinning of the retina itself. Retinal holes are typically smaller than tears but may require similar treatment in certain circumstances.
Risk Factors
- Age: Risk rises significantly after age 50 as age-related vitreous changes become more common.
- Family History: Genetics can play a role. A family background of retinal tears or detachment increases personal risk.
- Previous Eye Surgery: Past surgical interventions or laser therapy in the eye predispose to further complications.
- High Myopia (Nearsightedness): Those with severe myopia have thinner retinas and a higher risk of tears and holes.
- Retinal Disorders: Existing eye conditions such as lattice degeneration weaken retinal structures, making tears more likely.
Retinal Tear vs. Retinal Detachment
| Feature | Retinal Tear | Retinal Detachment |
|---|---|---|
| Definition | Break/rupture in the retinal tissue | Separation of retina from underlying support tissues |
| Symptoms | Flashes, floaters, shadows, curtain-like vision loss | Progression of curtain-like shadow, rapid vision loss |
| Pain | None | None |
| Severity | Moderate, risk for detachment | Very high—medical emergency |
| Treatment urgency | Prompt | Immediate (emergency) |
A retinal tear can directly progress to retinal detachment if fluid migrates beneath the retina, separating it from its blood supply and causing irreversible vision loss if not treated swiftly.
Diagnosis
If you experience any symptoms of a retinal tear, immediate evaluation by an ophthalmologist is essential. Diagnosis typically involves:
- Clinical History: Assessment of recent changes in vision, floaters, or light flashes.
- Dilated Eye Examination: The specialist uses dilating drops to examine the retina for tears, holes, or signs of detachment.
- Imaging: In some cases, tests such as optical coherence tomography (OCT) or fundus photography may be utilized to visualize the retina and vitreous.
- Ultrasound: If the view is obstructed by blood (vitreous hemorrhage), ocular ultrasound can help identify retinal tears or detachments.
Treatment Options
Treatment for retinal tears aims to seal the rupture and prevent retinal detachment. Early intervention is critical for favorable outcomes. Common therapies include:
Laser Photocoagulation
This procedure uses targeted laser energy to create small burns around the tear, forming a scar that seals the retina and prevents fluid migration underneath. It is highly effective and typically performed in an outpatient setting.
Cryopexy
Also known as freezing therapy, cryopexy applies intense cold energy to the area of the tear, triggering scar formation and sealing the defect. Cryopexy is often used for tears located in areas inaccessible to standard lasers.
Surgical Intervention
Surgery is reserved for cases where retinal tears have progressed to detachment or in complex scenarios. Procedures may include:
- Scleral Buckling: Involves placing a silicone band around the eye to push the wall closer to the retina, promoting reattachment.
- Vitrectomy: Removal of the vitreous gel, allowing direct access to repair tears and reattach the retina.
Observation
In rare cases where a retinal tear is very small and stable, careful monitoring by an eye specialist may suffice. However, due to the risk of progression, most tears are promptly treated.
Recovery and Outlook
Most individuals who receive prompt treatment for retinal tears regain stable vision and avoid complications. Recovery tips include:
- Follow all post-treatment instructions: Adhering to prescribed eye drops, medications, and activity restrictions aids recovery.
- Attend follow-up appointments: Regular checkups monitor for new tears or signs of detachment.
- Report new symptoms immediately: Sudden increase in floaters, flashes, or shadowing may signal further retinal problems requiring rapid intervention.
Delaying medical attention can result in permanent vision loss if retinal detachment occurs. Early diagnosis and treatment are key to preventing severe outcomes.
Prevention Strategies
While some risk factors for retinal tears, such as aging and genetics, cannot be altered, certain lifestyle modifications and precautions can help reduce the risk:
- Regular eye examinations: Individuals over 50, those with high myopia, or people with a family history should have routine dilated retinal evaluations.
- Protect your eyes: Use safety eyewear during sports or hazardous work to avoid trauma.
- Manage systemic health: Control conditions like diabetes and hypertension, which can impact retinal health.
- Be aware of warning signs: Learn the symptoms of retinal tears and detachment, and seek immediate care if they develop.
Frequently Asked Questions (FAQs)
Q: Is a retinal tear curable?
Yes. Retinal tears are often treatable with laser photocoagulation or cryopexy, especially when detected early. Prompt intervention prevents further complications and protects vision.
Q: Can a retinal tear heal without surgery?
Minor tears may sometimes heal, but natural healing is unreliable. Even small tears can progress to retinal detachment. Medical evaluation and treatment are strongly advised for any diagnosed tear.
Q: How serious is a retinal tear?
Retinal tears represent a possible threat to vision and should never be underestimated. Their seriousness stems from the risk of progressing to retinal detachment, which can cause permanent sight loss if untreated.
Q: What is the most common cause of retinal tear?
The most frequent cause is posterior vitreous detachment (PVD), where the eye’s vitreous gel separates from the retina, sometimes pulling and tearing the tissue.
Q: What should I do if I notice symptoms?
If you experience flashes, new floaters, vision loss, or curtain-like shadowing, seek emergency evaluation by an ophthalmologist. Immediate treatment can prevent complications.
Summary
Retinal tears are serious but treatable breaks in the back of the eye’s light-sensitive tissue. Often presenting with new floaters, light flashes, and visual shadows, they pose a significant risk of progression to retinal detachment and permanent vision loss. The most common causes include age-related vitreous changes and eye trauma. Laser and freezing therapies can effectively seal tears, and early detection is associated with excellent outcomes.
Be proactive about your eye health—understand your risk factors, recognize warning symptoms, and immediately seek care if you notice changes in your vision. Regular eye examinations and protective measures can help safeguard your sight for years to come.
References
- https://www.asrs.org/patients/retinal-diseases/26/retinal-tears
- https://www.healthline.com/health/eye-health/retinal-tear-vs-detachment
- https://www.medicalnewstoday.com/articles/retinal-tear-causes
- https://www.medicalnewstoday.com/articles/retinal-tear-treatment
- https://www.asrs.org/content/documents/fact-sheet-23-lp-retinal-tears-2020_1_asrs.pdf
- https://my.clevelandclinic.org/health/diseases/25107-retinal-tear
- https://specialty.vision/article/understanding-retinal-tears-symptoms-treatment-risks/
Read full bio of medha deb