Retinal Tear: Causes, Symptoms, Diagnosis, and Treatment
Learn about retinal tears, their symptoms, causes, risk factors, diagnosis, and effective treatments to protect your vision.
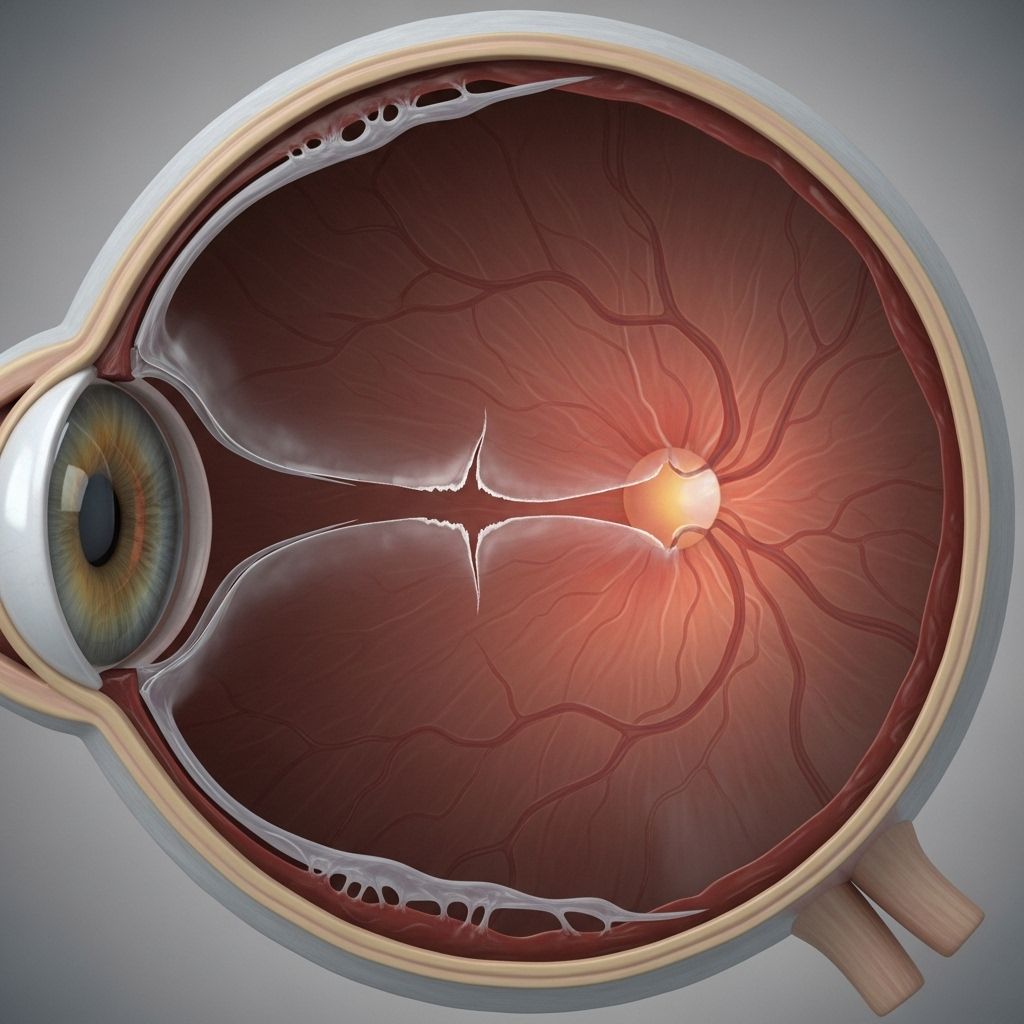
A retinal tear occurs when a rip develops in the thin layer of tissue, called the retina, that lines the back of your eye. Retinal tears are a serious medical concern that can lead to permanent vision loss if not addressed swiftly and appropriately. Early diagnosis and treatment can help prevent severe complications and preserve your vision.
Overview of Retinal Tears
The retina is a delicate layer of light-sensing cells at the back of your eye. It acts similar to film in a camera, capturing visual images and transmitting them to your brain for interpretation. When the retina develops a tear, it can disrupt these processes, putting your eyesight at risk. Retinal tears are considered a medical emergency due to the potential for vision-threatening complications, particularly retinal detachment.
- Retinal tears may occur in one or several spots along the retina.
- The condition is typically associated with aging and posterior vitreous detachment (PVD).
- Prompt treatment is crucial to prevent retinal detachment and vision loss.
Causes and Risk Factors for Retinal Tears
The interior of the eye is filled with a clear, gel-like substance called vitreous fluid. This gel is attached to the retina when you are born, but it may gradually pull away as you age—a process termed posterior vitreous detachment (PVD). Although PVD itself typically does not cause problems, the pulling away of vitreous fluid can sometimes tear the retina.
- Posterior vitreous detachment (PVD): The most common cause of retinal tears, especially after age 50.
- Eye trauma: Sudden impacts or injuries can cause retinal tears, even years after the event.
- Nearsightedness (myopia): Increases the risk due to the shape and stretching of the eyeball.
- Lattice degeneration: Refers to thin or weak patches in the retina, found in about 7–8% of people and associated with increased risk.
- Family history: Genetics may play a role; a family history of retinal tears can raise one’s risk.
- Previous eye surgery: Surgeries such as cataract removal can increase risk, especially if complications arise.
A 2023 study indicated that the risk of developing a retinal tear or detachment during PVD is approximately 9.9% at the time PVD is detected.
Symptoms of Retinal Tears
Retinal tears often do not cause pain, and small tears may not produce noticeable symptoms. However, certain signs are typical warning indicators.
- Flashes of light: Sudden appearance of light streaks or brief flashes, especially in the peripheral vision.
- Floaters: The sensation of dark spots, threads, or cobweb-like shapes drifting across your field of vision.
- Blurred vision: Unexplained or sudden clouding of your vision.
- Decreased peripheral vision: Loss or reduction in side vision (may indicate progression to retinal detachment).
- Shaded areas: A shadow or ‘curtain’ moving over part of your field of vision, which may signal a retinal detachment and should prompt immediate medical attention.
Symptoms can appear suddenly and may worsen as the tear progresses or if a detachment occurs.
Complications of Retinal Tears
If a retinal tear is not promptly diagnosed and treated, it can lead to more severe eye problems, the most significant being:
- Retinal Detachment: Fluid from the vitreous cavity may pass through the tear, causing the retina to lift or detach from its underlying tissue. This is a medical emergency that can result in irreversible vision loss.
- Permanent vision loss: Untreated tears and detachments may lead to loss of visual acuity or blindness in the affected eye.
Approximately 7–8 out of every 100 people have areas of lattice degeneration, further increasing their likelihood of complications if a tear occurs.
When to Seek Medical Help
Retinal tears and detachments are both considered medical emergencies. It is vital to seek immediate evaluation and treatment by an eye care professional if you experience:
- Sudden appearance of floaters or flashes of light
- Dark shadows or curtains descending across your vision
- Rapid decrease in central or peripheral vision
Delaying care may increase your risk of permanent vision loss.
Diagnosis of Retinal Tears
A comprehensive eye examination is required for diagnosis, which typically includes:
- Dilated eye exam: Special drops enlarge your pupils so the ophthalmologist can examine the retina for tears or detachment.
- Ophthalmoscopy: A detailed study of the eye’s interior using a slit lamp or specialized lens.
- Optical coherence tomography (OCT): A noninvasive scan that provides a detailed cross-section of the retina.
- Ultrasound imaging: Used if the retina cannot be fully visualized directly, such as when bleeding is present.
A prompt and accurate diagnosis is vital to direct the appropriate treatment and minimize complications.
Treatment Options for Retinal Tears
The primary goal of retinal tear treatment is to seal the tear and prevent retinal detachment. Several methods may be used, depending on the size, severity, and location of the tear:
- Observation and rest: For small, uncomplicated tears, your doctor may recommend rest and monitoring.
- Laser photocoagulation: A focused laser is used to create small burns around the tear, forming scar tissue that seals the retina to the underlying layer. This treatment is quick (usually less than 30 minutes), generally performed in the office, and usually causes only mild discomfort.
- Cryopexy (freeze therapy): A probe delivers intense cold to the area around the tear, creating a scar to anchor the retina.
- Surgery: Larger or more complicated tears, or cases involving bleeding or early detachment, may require more extensive surgical interventions.
Both laser and cryotherapy are highly effective in most cases and generally produce a good prognosis. Rapid treatment is key to reducing the risk of detachment and vision loss.
Comparison Table: Laser vs. Cryopexy Treatments
| Treatment | Method | Settings | Pain Level | Typical Use |
|---|---|---|---|---|
| Laser Photocoagulation | Burns retina around tear with a laser | Outpatient clinic/office | Mild | Most common, suitable for accessible tears |
| Cryopexy | Freezes tissue around tear | Outpatient clinic/office | Mild to moderate | Used for tears not easily reached by laser |
Recovery from Retinal Tear Treatment
Recovery following treatment for a retinal tear varies depending on the type and extent of the procedure. Most people can expect:
- Improvement in symptoms (such as flashes or floaters) within several days to weeks after treatment.
- Resumption of non-strenuous activities soon after, but heavy lifting, bending, or strenuous exercise should typically be avoided for a period specified by your doctor.
- Follow-up visits to monitor retinal health and healing progress.
- Prompt return to medical care if new symptoms develop (such as increased floaters, vision loss, or new flashes).
While many people recover well after treatment, some may experience lasting changes in vision. Early treatment significantly increases the likelihood of retaining useful vision.
Prevention of Retinal Tears
While not all retinal tears are preventable, you can lower your risk by following these recommendations:
- Regular eye exams: Comprehensive examinations can help catch early changes, especially if you are at higher risk.
- Protect your eyes from trauma: Use appropriate eye protection during sports or high-risk activities.
- Manage underlying conditions: Control diabetes, high blood pressure, and other illnesses that increase eye disease risk.
- Stay alert to symptoms: Seek immediate evaluation if you notice new flashes, floaters, or visual shadows.
- Follow your ophthalmologist’s advice: This is especially important if you have risk factors like high myopia, lattice degeneration, or a family history.
For those with a history of retinal tears, careful monitoring and diligent eye care are essential.
Outlook for Retinal Tear
The outlook for retinal tears has improved dramatically with early detection and modern treatment approaches. Most people who receive timely care retain useful vision and avoid serious complications. However, prognosis depends on factors such as:
- The size and location of the tear
- How quickly treatment is provided
- Presence of associated conditions or other eye diseases
- Severity of symptoms and initial visual acuity
People who have experienced a retinal tear carry a slightly higher risk of new tears or detachment in either eye, necessitating lifelong vigilance and regular follow-up care.
Frequently Asked Questions (FAQs)
What happens if a retinal tear is not treated?
The main risk is retinal detachment, which occurs when fluid seeps behind the retina through the tear, causing it to pull away from the underlying tissues. Untreated retinal detachment can lead to permanent and severe vision loss in the affected eye.
Is a retinal tear painful?
No. Retinal tears themselves do not cause pain. However, they can cause alarming visual symptoms (such as new floaters or flashes), so prompt evaluation is essential.
Can a retinal tear heal on its own?
Small tears may not worsen, but they do not heal spontaneously. Most require treatment to prevent detachment. Your ophthalmologist will determine the appropriate approach based on tear severity and your risk profile.
Who is most at risk for retinal tears?
People over the age of 50, those with significant nearsightedness, individuals with a history of eye injury or surgery, and those with thin patches in their retina (lattice degeneration) or a family history of retinal tears face increased risk.
What steps can I take after retinal tear treatment?
- Follow all post-procedure instructions.
- Attend scheduled follow-up appointments for monitoring.
- Report any new or worsening symptoms to your eye doctor promptly.
- Avoid strenuous activities until cleared by your doctor.
Summary
A retinal tear is a serious tear in the light-sensitive layer at the back of the eye, commonly linked to age-related changes in the vitreous gel. While not always symptomatic, sudden onset floaters, flashes, or shadowed vision should prompt immediate medical evaluation. Early and effective treatment is the key to protecting your eyesight, preventing retinal detachment, and ensuring the best possible vision for the future.
References
- https://www.med.umich.edu/1libr/Ophthalmology/Retina/RetinalTear.pdf
- https://www.retinamd.com/retinal-conditions-and-diseases/retinal-tears-and-detachments/
- https://www.medicalnewstoday.com/articles/retinal-tear
- https://www.healthline.com/health/eye-health/retinal-tear
- https://www.healthline.com/health/eye-health/retinal-tear-vs-detachment
- https://www.medicalnewstoday.com/articles/retinal-tear-treatment
- https://www.asrs.org/content/documents/fact-sheet-23-lp-retinal-tears-2020_1_asrs.pdf
- https://my.clevelandclinic.org/health/diseases/25107-retinal-tear
- https://www.britannica.com/science/detached-retina
Read full bio of Sneha Tete












