Who Is at Risk for Retinal Detachment? Key Factors, Symptoms, and Prevention
Understand the risk factors, symptoms, and strategies for early detection and prevention of retinal detachment to protect your vision.
Who Is at Risk for Retinal Detachment?
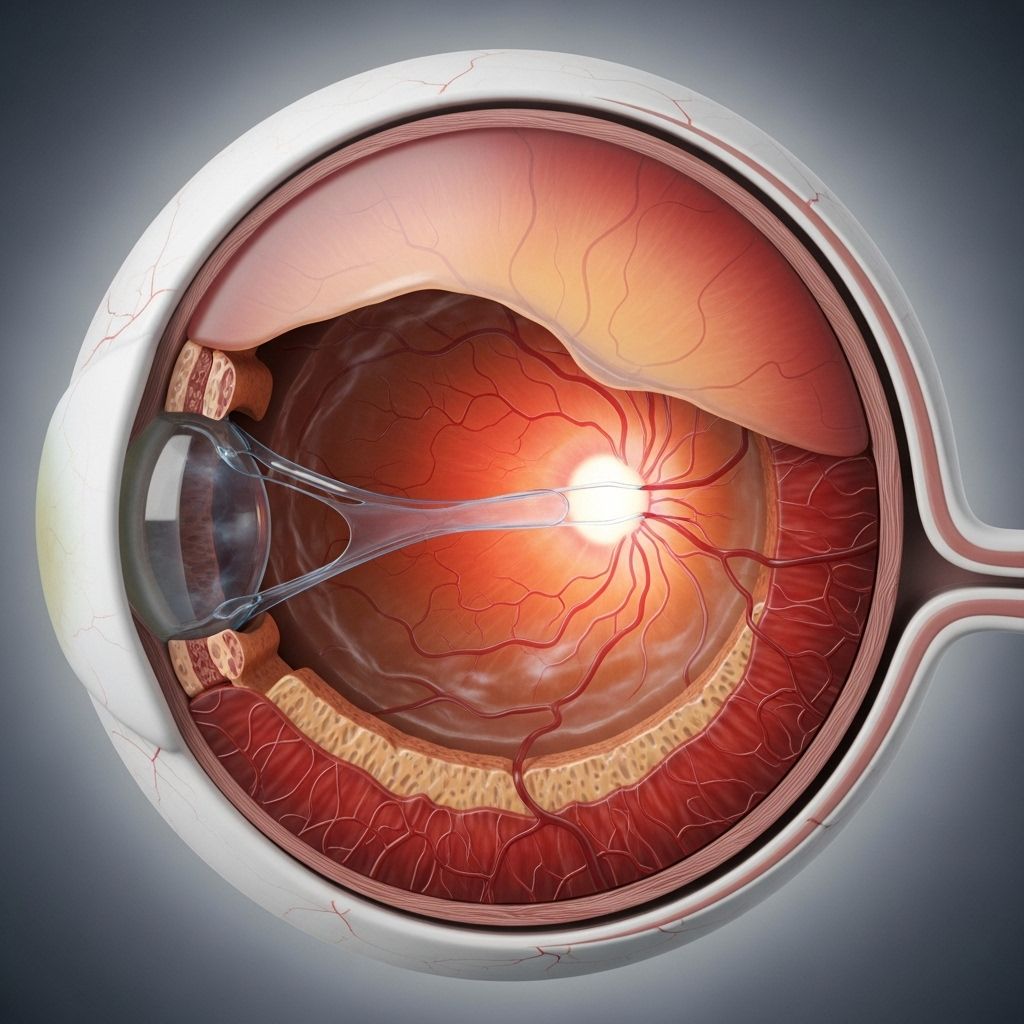
Retinal detachment is a serious eye condition where the retina — the thin layer of tissue at the back of the eye — separates from its underlying support tissue. This separation can cause permanent vision loss if not treated quickly. Understanding who is at risk allows for early detection, better prevention, and timely treatment.
What Is Retinal Detachment?
The retina plays a critical role in vision, converting light into neural signals the brain can interpret. When the retina pulls away from supportive tissues, it loses access to essential nutrients and oxygen, threatening its function. Detached retinas require prompt medical intervention to prevent irreversible vision loss.
Common Risk Factors for Retinal Detachment
While anyone can potentially develop retinal detachment, certain individuals have a higher risk due to genetic, physiological, and environmental factors. Key risk factors include:
- Family history of retinal detachment (especially in first-degree relatives)
- Previous eye injuries such as blunt trauma or heavy lifting accidents
- Past eye surgery, especially cataract removal
- Eye diseases and conditions, such as diabetic retinopathy or macular degeneration
- Age — increased risk as you get older
Family History and Genetics
Genetics play a significant role in retinal detachment risk. Studies show:
- People with a first-degree relative (parent, sibling, child) who has had a detached retina are at significantly higher risk.
- Research suggests that the lifetime risk doubles if a first-degree family member has experienced retinal detachment, pointing to a strong hereditary component.
- Detachment can cluster within families, indicating genetic predisposition.
Knowing your family eye-health history can help with effective risk assessment and early monitoring.
Other Health and Eye Conditions
Certain medical and ophthalmic conditions increase the risk of retinal detachment:
- Extreme nearsightedness (high myopia): People who are very nearsighted have longer eyeballs, which stretches and thins the retina, making tears and detachment more likely.
- Diabetic retinopathy: Diabetes can damage retinal blood vessels, making the retina more vulnerable to detachment.
- Diabetic macular edema: This diabetes-related condition increases retinal swelling and risk for separation.
- Glaucoma: Elevated eye pressure and treatments may weaken the retina or the support tissues.
- Age-related macular degeneration (AMD): Damage to the retina due to degeneration may trigger or exacerbate detachment.
- Posterior vitreous detachment: The gel-like fluid in the eye (vitreous) pulling away from the retina increases the chance of tears.
- Previous retinal detachment: If you have had a detached retina in one eye, your risk increases for the other eye.
Other, less common causes include eye diseases like Coats disease (abnormal retinal vessels), retinal separation, and areas of thinning in the retina called lattice degeneration.
Age, Eye Injuries, and Surgeries
Age is an independent risk factor. Retinal detachment becomes more likely as you grow older, particularly between ages 40 and 70. With aging, the vitreous gel within the eye shrinks and can tug on the retina, leading to tears or detachment.
- Eye injuries: Any trauma or blunt force to the eye increases detachment risk, both immediately and long term. Examples include sports injuries, falls, or accidents during physical activities.
- Eye surgeries: Procedures like cataract removal, retinal laser treatments, or injections can inadvertently compromise the retina, especially in individuals already predisposed through other factors.
People who have had past retinal detachment or those with scars or thin spots are at heightened risk for recurrence.
A Personal Perspective: Living with High Risk Factors
Many people carry several risk factors for retinal detachment, sometimes without realizing it. Consider the story of a person living with:
- Type 1 diabetes since childhood, resulting in diabetic retinopathy and macular edema.
- Glaucoma, increasing intraocular pressure and risk.
- Family history — maternal relatives with cataracts and paternal relatives with detached retinas.
- Nearsightedness from an early age.
- Age over 40, marking the period of heightened risk.
In this example, a paternal uncle had a detached retina in his 50s, successfully treated thanks to early intervention. Later, the person’s father also experienced retinal detachment, which was detected after he noticed unusual vision changes while driving. Prompt treatment helped preserve his sight. These personal accounts underscore why knowing your risk profile and watching for symptoms is critical.
Other Noteworthy Risk Factors
Beyond those already detailed, additional risks include:
- Uveitis (eye inflammation)
- Retinoschisis (retina splitting into layers)
- Weak areas in the retina, detectable by an eye doctor
- Thinning of the peripheral retina, known as lattice degeneration, which is especially prevalent in people with high myopia
Why Early Detection Matters
Retinal detachment is considered a medical emergency. The American Academy of Ophthalmology (AAO) emphasizes the importance of early detection. Timely diagnosis and intervention can mean the difference between vision preservation and permanent blindness.
Doctors should inform people at high risk about warning signs and advise them to seek medical care immediately if symptoms occur. Routine eye exams and periodic fundus (retina) checks, especially with a retinal specialist, are vital in identifying retinal tears before they advance to detachment.
Symptoms to Watch For
- Sudden onset of floaters: Seeing small specks or cobwebs drifting in your field of vision
- Flashes of light: Brief flashes or streaks of light, usually in the peripheral vision
- A shadow or curtain effect: Loss of vision resembling a shadow or curtain descending over part of your visual field
- Blurred or distorted vision
If you notice any of these symptoms, especially if they appear suddenly or worsen, prompt medical attention is essential.
Diagnosis: How Is Retinal Detachment Detected?
To diagnose retinal detachment, an eye care professional conducts a series of tests:
- Dilated eye exam: The doctor examines the retina, optic nerve, and blood vessels by dilating your pupils.
- Vision tests: These assess overall sharpness, peripheral vision, and color perception.
- Eye pressure measurement: Elevated intraocular pressure can signal related eye disorders.
- Imaging scans:
- Optical coherence tomography (OCT): Produces high-resolution images of the retina for detailed assessment.
- Retinal photography: Documents the extent of retinal changes or detachment.
- Ultrasound: Utilized when a direct view is hindered (for example, by bleeding or cataract). Sound waves create a visual map of the internal eye structures.
Specialized exams may include scleral depression, where gentle pressure is used to examine the retina’s farthest corners for tears or weak spots. A thorough exam is critical for an accurate diagnosis and appropriate intervention.
Minimizing Your Risk: Preventive Measures
While not all cases can be prevented, certain strategies can significantly reduce your risk and promote early detection:
- Regular comprehensive eye exams — especially if you have risk factors or are over 40.
- Monitor your vision: Be observant for new symptoms, such as floaters, flashes, or visual shadows. Report changes to your eye doctor immediately.
- Safety measures: Wear protective eyewear during sports or hazardous activities to reduce the risk of trauma.
- Manage systemic health conditions: Keep blood sugar and blood pressure under control, especially if you have diabetes or hypertension.
- Promptly treat eye diseases: Follow recommendations for controlling glaucoma, managing macular degeneration, or addressing diabetic eye disease.
- Discuss your family history: Make your eye doctor aware of any family eye disease, so they can adjust exams and monitoring protocols accordingly.
These steps may help detect retinal issues before they advance, giving you the best chance to preserve your vision.
Retinal Detachment Risk Factors Table
| Risk Factor | Explanation |
|---|---|
| Family History | Increased risk, especially with a first-degree relative who had detachment |
| Extreme Nearsightedness (Myopia) | Longer eye length stretches/thins the retina |
| Previous Eye Injury | Trauma can cause tears or weakened retinal tissue |
| Past Eye Surgery | Procedures such as cataract removal may elevate risk |
| Aging | More common in ages 40–70 due to vitreous changes |
| Other Eye Diseases | Conditions like glaucoma, diabetic retinopathy, AMD, lattice degeneration |
Frequently Asked Questions (FAQs)
Who is at the highest risk for retinal detachment?
People with a family history of retinal detachment, high myopia (extreme nearsightedness), past eye injuries or surgeries, existing eye conditions (like diabetic retinopathy or glaucoma), and those over age 40 face the highest risk.
Can retinal detachment be prevented?
While not all cases can be prevented, lowering risk factors—such as wearing protective eyewear, attending regular eye exams, and managing chronic health conditions—can reduce likelihood and support early detection for best outcomes.
Are symptoms always noticeable before serious vision loss?
No. Some people experience subtle or no symptoms until significant detachment and vision loss occurs, which is why routine screenings are so important for high-risk individuals.
Does myopia (nearsightedness) always lead to detachment?
No, but people with high myopia have a higher risk because their elongated eyes stretch and thin the retina, making tears or detachment more likely than in the general population.
What should I do if I notice sudden floaters, flashes, or visual shadows?
Seek immediate medical care from an eye specialist. Timeliness is critical to prevent permanent vision loss.
How often should I have eye exams if I’m at high risk?
Your eye doctor may recommend annual or even more frequent exams if you have multiple risk factors. These exams can catch problems early, even before symptoms appear.
Key Takeaways
- Retinal detachment is a vision-threatening condition requiring urgent care.
- Major risk factors include family history, high myopia, eye injuries, previous surgeries, certain eye diseases, and age.
- Symptoms to watch for include new floaters, light flashes, and shadows or curtains over your vision.
- Routine comprehensive eye exams are crucial for high-risk individuals.
- Early detection and treatment dramatically improve outcomes and can help preserve eyesight.
If you belong to any high-risk group or notice possible symptoms, consult an ophthalmologist or retinal specialist promptly. Protecting your eye health now can prevent serious complications in the future.
References
- https://www.healthline.com/health/eye-health/who-is-at-risk-for-detached-retina
- https://www.healthline.com/health/retinal-detachment
- https://www.asrs.org/retinaldetachment
- https://www.mayoclinic.org/diseases-conditions/retinal-detachment/symptoms-causes/syc-20351344
- https://www.umkelloggeye.org/conditions-treatments/detached-retina-retinal-detachment
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/retinal-detachment/types-and-causes-retinal-detachment
- https://stanfordhealthcare.org/medical-conditions/eyes-and-vision/retinal-detachment/risk-factors.html
- https://my.clevelandclinic.org/health/diseases/10705-retinal-detachment
- https://www.youtube.com/watch?v=Vgc2zzPprlY
Read full bio of Sneha Tete












