Retinal Bleeding: Symptoms, Causes, Diagnosis, and Treatment
Learn about retinal bleeding—its causes, symptoms, types, risk factors, treatment options, and how timely intervention helps protect your vision.
Retinal Bleeding: Understanding the Causes, Symptoms, and Treatment
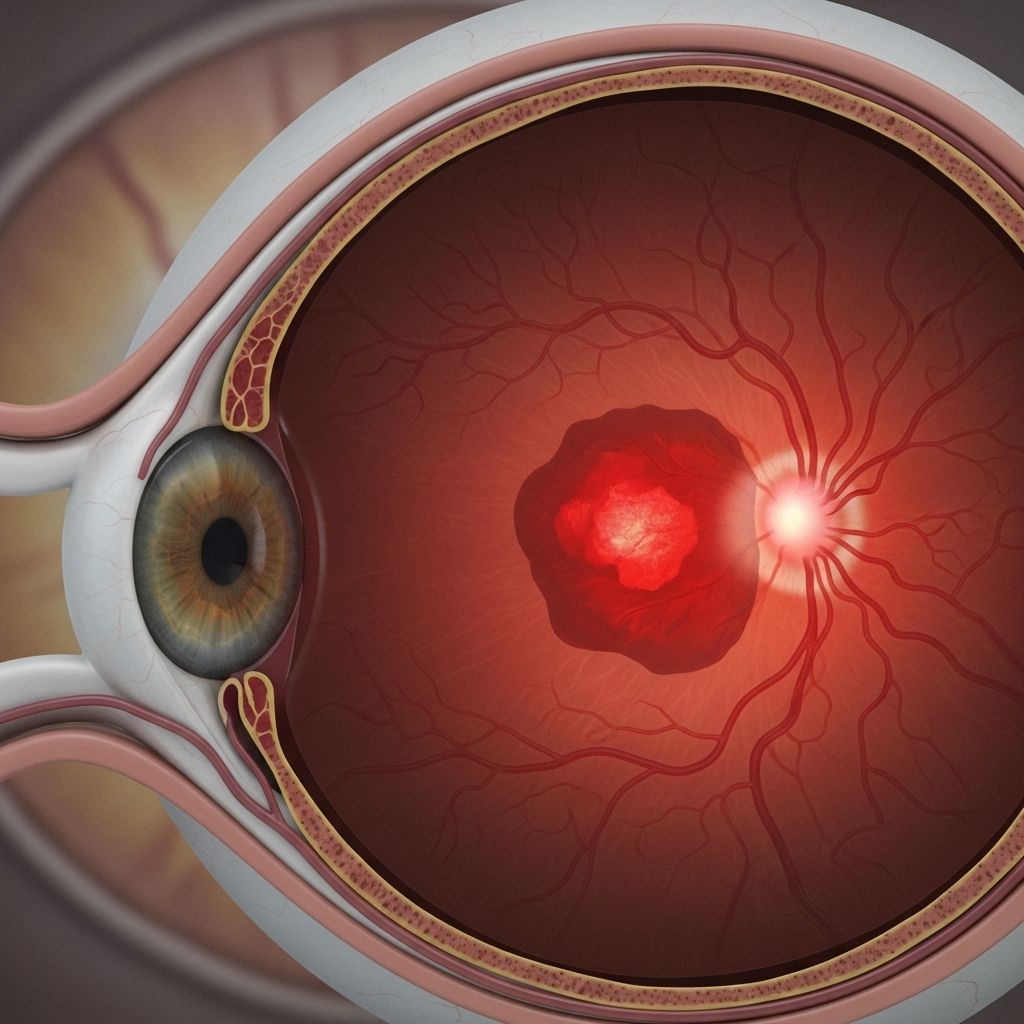
Retinal bleeding, also referred to as retinal hemorrhage, is a potentially serious eye condition where blood escapes from the tiny blood vessels inside the retina—the light-sensitive tissue at the back of the eye responsible for vision. Prompt recognition and treatment are crucial to preserving sight and addressing possible underlying health concerns.
What is Retinal Bleeding?
Retinal bleeding describes the leakage of blood from small blood vessels into the layers of the retina. Unlike superficial eye bleeds (such as subconjunctival hemorrhage), retinal bleeds can directly threaten the cells vital for vision, risking permanent damage if not treated swiftly.
- The retina contains millions of light-sensitive cells and micro-vessels that help capture and process visual information.
- Bleeding may present as pinpoint spots, flame-shaped streaks, or larger pooled areas depending on the location and severity.
- Damage may occur from health conditions, trauma, or systemic disease affecting blood vessels in the eye.
Why is Retinal Bleeding Clinically Important?
Retinal hemorrhages not only pose threats to vision, but can also signal deeper systemic problems like uncontrolled diabetes, hypertension, blood disorders, or trauma. If left untreated, bleeding may result in complications such as scarring, fluid accumulation (macular edema), or retinal detachment—all of which can lead to lasting vision loss.
- May be the first sign of underlying diseases requiring further investigation.
- Prompt diagnosis and intervention are critical for preventing permanent vision impairment.
- Associated with both acute and chronic conditions (from sudden injury to slow-developing vascular disorders).
Common Symptoms of Retinal Bleeding
The symptoms of retinal bleeding vary depending on the extent and location of the hemorrhage. Some people may experience noticeable changes, while others may have no symptoms until the condition becomes advanced.
- Blurry or hazy vision
- Sudden appearance of floaters—dark spots or thread-like strands drifting in your field of vision
- Blind spots (scotomas) or loss of part of the visual field
- Vision with a red tint or seeing streaks/lines
- Reduced vision that is often worse upon waking up
- Occasionally, complete or sudden vision loss, especially with severe bleeds or associated retinal detachment
Sometimes, minor hemorrhages may have no symptoms and are only detected during a routine eye exam.
Types of Retinal Hemorrhages
The type and appearance of retinal bleeding can give clues about its cause and severity. Eye doctors classify hemorrhages by their shape, depth, and anatomical location within the retina, each carrying its own implications.
| Type | Description | Common Causes |
|---|---|---|
| Vitreous & Preretinal Hemorrhages | Blood leaks into the gel (vitreous) or just in front of the retina; may settle at the eye’s bottom. | Diabetes, trauma, high blood pressure, abnormal vessel growth |
| Flame-Shaped Hemorrhages | Thin streaks resembling flames, feathers, or splinters seen under examination. | Hypertension, blood and artery disorders, certain anemias |
| Dot or Blot Hemorrhages | Round, uniform spots found deeper in the retina. | Diabetic retinopathy, vein occlusions, rare eye disorders |
| Roth Spots | Hemorrhages with a white center, indicating underlying disease. | Diabetes, leukemia, hypertension, endocarditis |
| Other Types | Associated with systemic conditions and side effects of medication. | Radiation, infections, blood disorders, medications |
What Causes Retinal Bleeding?
Retinal hemorrhages can result from a variety of factors. Understanding the root cause helps guide effective management and prevents recurrence.
- Medical conditions: Uncontrolled diabetes (diabetic retinopathy), high blood pressure (hypertension), blood disorders (anemia, leukemia), autoimmune diseases (like lupus), and infections.
- Eye diseases: Macular degeneration (especially the wet type due to abnormal vessel growth), retinal vein occlusion, retinal vasculitis.
- Trauma: Direct eye injury, head trauma, shaken baby syndrome, abusive head trauma in infants.
- Sudden pressure changes: Rapid changes in atmospheric pressure during activities such as diving or high-altitude climbing.
- Medications: Blood thinners (anticoagulants), which increase bleeding risk.
- Other rare causes: Severe coughing, vomiting, or straining (valsalva retinopathy), radiation therapy, or complications from invasive eye procedures.
Who Is Most at Risk?
Although retinal bleeding can occur in anyone, certain groups are more vulnerable due to underlying health conditions or circumstances:
- Adults over 40, especially individuals with diabetes or hypertension
- Infants and children, particularly in cases of birth trauma or suspected abuse
- People with blood disorders (e.g., anemia, leukemia, clotting disorders)
- Those on anticoagulant (blood-thinning) medication
- Individuals with a history of eye injuries or surgery
- People exposed to sudden atmospheric pressure changes
Populations with limited access to eye care or regular screening face higher risks of delayed diagnosis and complications.
How is Retinal Bleeding Diagnosed?
A comprehensive eye exam by an ophthalmologist is essential for diagnosing retinal bleeding and its underlying cause. Diagnostic steps may include:
- Visual acuity test: Measures how well you see at various distances.
- Dilated eye exam: Allows detailed viewing of the retina using special lenses after widening (dilating) the pupils.
- Fundoscopy (ophthalmoscopy): Direct visualization of the retina to locate bleeding and its features.
- Optical coherence tomography (OCT): High-resolution imaging to detect swelling, blood, and fluid within retinal layers.
- Fluorescein angiography: Injection of a dye into the bloodstream to visualize abnormal retinal vessels and leaks.
- Blood tests or general health assessments: To check for systemic diseases such as diabetes, hypertension, clotting disorders, or infections.
Early detection during routine eye exams is especially important for those at higher risk of ocular and systemic vascular diseases.
Treatment Options for Retinal Bleeding
Treatment depends on the bleed’s severity, underlying cause, and how much it affects vision. Strategies may include:
- Managing underlying health conditions:
- Tight control of blood sugar in diabetes
- Lowering blood pressure in hypertension
- Treating blood or infectious diseases as needed
- Laser photocoagulation: Seals leaking vessels or abnormal neovascularization, especially in diabetic retinopathy or macular degeneration.
- Intravitreal injections: Anti-VEGF (vascular endothelial growth factor) drugs or steroids injected into the eye to reduce neovascularization, swelling, and bleeding.
- Vitrectomy: A surgical procedure to remove blood and scar tissue from the vitreous gel, restoring vision if bleeding is severe or persistent.
- Observation: Small, stable hemorrhages may be monitored for spontaneous resolution if they do not threaten vision or stem from self-limiting causes.
- Addressing secondary complications: Such as managing infections, controlling inflammation, or treating underlying systemic conditions.
What Happens If Retinal Bleeding Is Left Untreated?
Potential complications of untreated or recurrent retinal bleeding include:
- Permanent vision loss due to damage to light-sensitive retinal cells
- Scarring and macular edema causing persistent blurriness or central vision loss
- Retinal detachment leading to profound visual impairment or blindness
- Progression of undiagnosed systemic conditions like diabetes or hypertension
Preventing Retinal Bleeding: Tips for Eye Health
Protecting your eyes and overall vascular health reduces your risk of retinal bleeding. Here are actionable strategies:
- Keep blood sugar and blood pressure consistently controlled if you have diabetes or hypertension
- Attend all regular eye exams, especially if you are at increased risk
- Report new changes in vision promptly—do not ignore acute visual symptoms
- Use appropriate eye protection to avoid physical trauma
- Discuss with your doctor if taking blood thinners or if you have a bleeding disorder
- Maintain a healthy lifestyle with a balanced diet and regular exercise
Good communication with healthcare providers supports early detection, effective management, and better vision outcomes.
Frequently Asked Questions (FAQs) About Retinal Bleeding
Q: Is retinal bleeding a medical emergency?
A: Sudden vision changes or severe eye pain can indicate a medical emergency. If you experience abrupt vision loss, sudden onset of floaters, or a curtain-like shadow, seek immediate care to prevent further damage.
Q: Can retinal bleeding heal on its own?
A: Small, uncomplicated hemorrhages may resolve naturally, particularly when the underlying cause is managed. However, significant or recurrent bleeding requires medical evaluation to prevent permanent loss of vision.
Q: What can I do to reduce my risk?
A: Manage chronic health conditions (diabetes, high blood pressure), attend regular eye exams, wear eye protection in hazardous situations, and adopt a healthy lifestyle to lower general vascular risk.
Q: Is retinal bleeding always painful?
A: Most retinal hemorrhages are painless, but some cases (especially when associated with trauma or retinal detachment) may cause discomfort. Any change in vision or eye pain should prompt professional evaluation.
Q: Who should I see for retinal bleeding?
A: Visit an ophthalmologist or retina specialist promptly, especially if you notice visual changes. If bleeding is discovered during a routine exam, your eye doctor will refer you for further assessment and management.
Key Takeaways for Protecting Your Vision
- Retinal bleeding is a serious eye condition that can threaten sight and signal underlying health problems.
- Early detection and treatment are critical—especially for those with diabetes, hypertension, or history of trauma.
- Managing general health and regular eye screening can help prevent complications and preserve vision long-term.
References
- https://brightsight.com.au/2025/06/18/retinal-bleeding/
- https://www.allaboutvision.com/conditions/retinal-hemorrhage/
- https://my.clevelandclinic.org/health/diseases/25106-retinal-hemorrhage
- https://www.medicalnewstoday.com/articles/retinal-hemorrhage
- https://www.healthline.com/health/eye-health/vitreous-hemorrhage
- https://patient-rvo.vision-relief.com/introduction/what-is-retinal-vein-occlusion/
- https://www.ncbi.nlm.nih.gov/books/NBK560777/
- https://www.healthline.com/health/eye-health/eye-bleeding
- https://www.mayoclinic.org/diseases-conditions/retinal-diseases/symptoms-causes/syc-20355825
Read full bio of medha deb












