Retinal Bleeding: Causes, Symptoms, Diagnosis, and Treatment
A thorough guide to retinal bleeding, its origins, risks, symptoms, diagnostic methods, and treatment strategies for safeguarding vision.
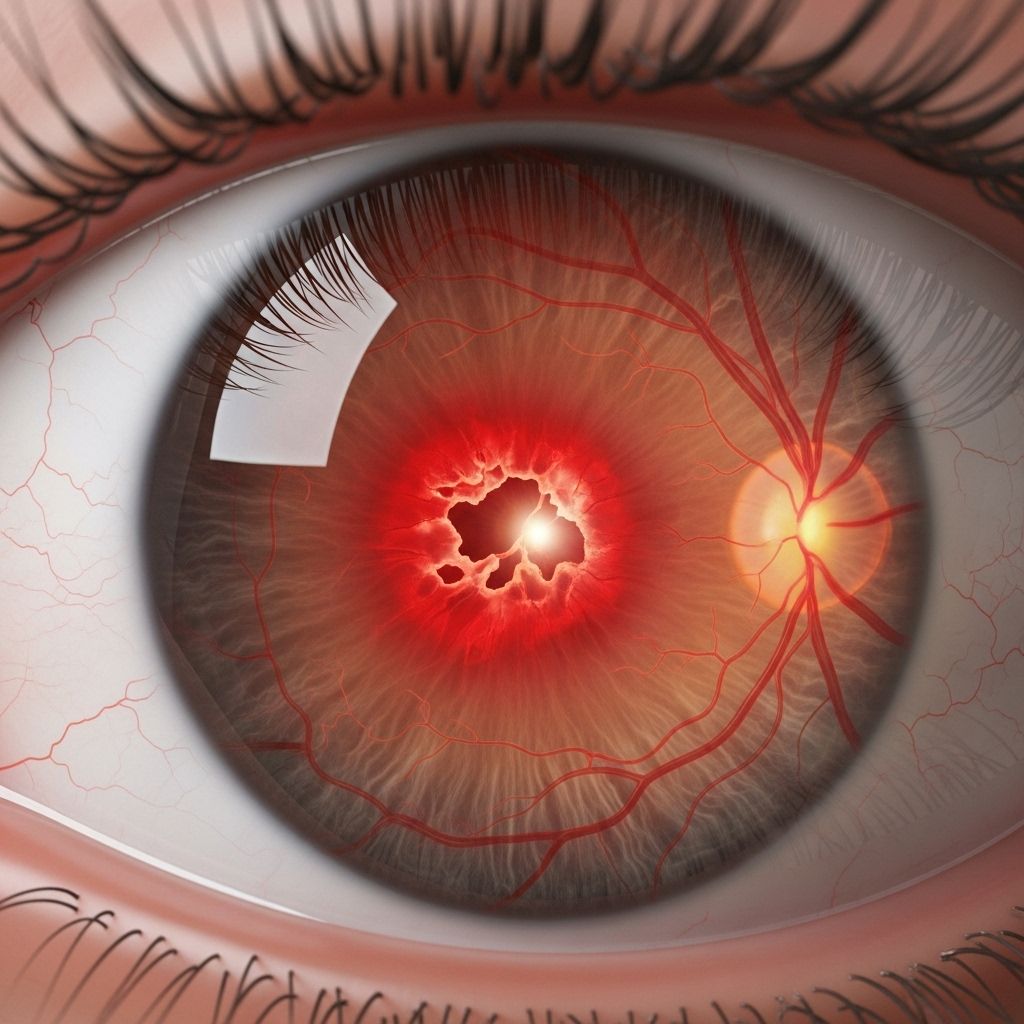
Retinal Bleeding: Understanding the Silent Threat to Vision
Retinal bleeding, medically known as retinal hemorrhage, can pose an acute threat to sight and may signal underlying systemic health problems requiring prompt attention. This condition arises when the tiny blood vessels nourishing the retina—the delicate, light-sensitive membrane at the back of the eye—rupture and leak blood into its layers. Whether caused by diseases such as diabetes or hypertension, traumatic injury, or rare blood disorders, retinal bleeding is a significant concern in eye health with the potential to lead to vision loss if untreated.
What Is Retinal Bleeding?
Retinal bleeding describes any leakage of blood within the layers of the retina due to damage or rupture of small blood vessels. The retina captures light and sends visual signals to your brain, underpinning your ability to see. When blood invades this space, it disrupts function and may immediately or gradually affect vision.
- Types of Retinal Hemorrhage:
- Dot-and-blot hemorrhages: Small, round bleeding spots within the deeper layers.
- Flame-shaped hemorrhages: Linear streaks of blood along the retinal nerve fibers.
- Subhyaloid hemorrhage: Blood pooling between the retina and the vitreous.
- Large hematomas: Extensive bleeding forming a mass.
- This bleeding is distinct from more superficial ocular bleeds such as subconjunctival hemorrhages (on the eye’s white) or hyphema (blood in the front chamber of the eye).
Clinical Significance of Retinal Bleeding
Retinal hemorrhages are not merely ocular symptoms but can be harbingers of systemic health problems. Prompt recognition and intervention are vital to minimize retinal scarring, fluid accumulation (macular edema), retinal detachment, or lasting vision impairment.
- Retinal bleeding may be the first observable sign of a larger problem, such as diabetes, hypertension, or blood disorders.
- Early treatment options, like laser therapy or intravitreal medication, can control damage and preserve sight.
- Delayed diagnosis can result in permanent loss of visual acuity.
Retinal Bleeding as a Systemic Warning
Detecting hemorrhages during eye exams may prompt deeper investigation for systemic conditions, including:
- Diabetes
- High cholesterol
- Coagulation disorders
- Cardiovascular diseases
Who Is Most at Risk?
While anyone can develop retinal bleeding, some groups face greater risk:
- Older adults >40 years, especially those with chronic diseases like diabetes or high blood pressure.
- Infants, particularly those delivered with forceps or experiencing abusive head trauma (shaken baby syndrome), with a high prevalence seen in some pediatric cases.
- People in rural or underserved regions are vulnerable due to reduced access to specialist eye care and routine screening.
- Individuals with pre-existing eye conditions such as macular degeneration.
Symptoms of Retinal Bleeding
Retinal bleeding often begins silently, without pain or obvious discomfort, making regular eye exams critical. However, once blood disrupts retinal function, symptoms may arise such as:
- Sudden blurry or distorted vision
- Appearance of floaters (spots or cobwebs drifting in the field of view)
- Partial or total loss of vision in one or both eyes
- Dark spots (scotomas)
- Occasional eye pain or discomfort, but pain is less common unless accompanied by other complications
Symptoms can vary depending on the hemorrhage’s location and size. Hemorrhages near the macula—responsible for central sharp vision—can cause rapid and profound changes in sight.
What Causes Retinal Bleeding?
There are many possible causes for retinal bleeding. Understanding these is crucial to both preventing and managing the condition:
- Diabetic retinopathy: High blood sugar damages retinal vessels, weakening their walls and leading to leakage or bleeding.
- Hypertension (high blood pressure): Chronic elevated pressure can rupture retinal arteries or veins.
- Age-related macular degeneration (AMD): New abnormal blood vessels form beneath the retina, prone to bleeding in advanced stages.
- Eye trauma: Physical injuries—including blunt force or penetrating trauma—can rupture vessels.
- Blood disorders: Conditions or medications affecting clotting (e.g., anemia, leukemia, anticoagulants) heighten bleeding risk.
- Infections: Certain viral, bacterial, or inflammatory diseases may attack blood vessels, causing hemorrhages.
- Pediatric causes: Trauma and delivery injury are leading causes in newborns and infants. Shaken baby syndrome is closely associated with retinal hemorrhages.
| Cause | Mechanism | Typical Patient |
|---|---|---|
| Diabetic Retinopathy | High blood sugar damages retinal vessels | Adults with diabetes |
| Hypertension | Elevated blood pressure ruptures vessels | Older adults |
| Age-related Macular Degeneration | Fragile new vessels bleed | Adults >60 |
| Trauma | Injury ruptures vessels | Any age |
| Blood Disorders | Affects normal clotting | All ages |
| Pediatric Injury | Delivery or abusive trauma | Infants, children |
Diagnosis: How Is Retinal Bleeding Detected?
Because many cases are painless and asymptomatic at first, routine ophthalmic exams play a key role in early detection. Diagnosis involves:
- Comprehensive eye exam: Visual acuity testing, slit-lamp examination, and direct visualization of the retina using ophthalmoscopy.
- Pupil dilation: Drops enlarge the pupils for better viewing of the back of the eye.
- Imaging tests:
- Optical coherence tomography (OCT): Scans the retina in high resolution to locate and measure bleeding or swelling.
- Fundus photography: Documents the retina’s appearance over time.
- Fluorescein angiography: Uses dye to highlight abnormal blood vessels and pinpoint sources of leakage/bleeding.
- Systemic evaluation: Additional blood tests or referral may identify underlying disorders, such as diabetes, hypertension, or blood dyscrasias.
Treatment Options for Retinal Bleeding
Managing retinal bleeding depends on its underlying cause, hemorrhage severity, and the patient’s overall health. Treatment strategies include:
- Lifestyle and Medical Management:
- Control of diabetes and hypertension through medication, diet, and exercise.
- Management of underlying blood disorders or clotting abnormalities.
- Laser Photocoagulation:
- A targeted laser seals leaking blood vessels, preventing further bleeding and limiting retinal damage.
- Especially effective for diabetic retinopathy or small hemorrhages.
- Intravitreal Injections:
- Direct injection of medication into the vitreous gel reduces abnormal vessel growth (especially in AMD) and inflammation.
- Common agents: anti-VEGF therapy, steroids.
- Vitrectomy:
- Surgical removal of blood-filled vitreous gel, restoring clarity and access for retina repair.
- Reserved for cases with extensive bleeding or non-resolving hemorrhage.
- Observation:
- Small, stable hemorrhages may resolve without intervention under close monitoring.
Preventing Retinal Bleeding
Prevention requires managing risk factors and regular eye health monitoring. Consider the following strategies:
- Monitor and control blood sugar for diabetic patients.
- Maintain healthy blood pressure with lifestyle changes and medication.
- Treat underlying blood or cardiovascular disorders.
- Protect eyes against trauma, especially during sports or high-risk activities.
- Routine comprehensive eye exams, particularly for those over 40 or with chronic health conditions.
FAQs: Retinal Bleeding
What is the retina and why is it so important?
The retina is a thin, light-sensitive membrane at the back of the eye that captures visual information and transmits it to the brain via the optic nerve. It is essential for sight; any disruption, such as bleeding, may lead to compromised vision.
Is retinal bleeding always painful or noticeable?
Not always. Many cases are painless and go unnoticed until vision changes occur. Regular eye examinations are crucial for catching silent problems before they cause irreversible damage.
Can retinal bleeding cause permanent blindness?
If severe or untreated, retinal bleeding can result in permanent vision loss due to scarring, macular edema, or retinal detachment. Early intervention and treatment greatly reduce this risk.
Who should be screened regularly for retinal bleeding?
- Individuals with diabetes, hypertension, or blood disorders
- Adults over 40
- Infants with history of difficult delivery or possible trauma
- Anyone experiencing sudden visual changes or eye injury
What are the long-term outcomes for treated retinal bleeding?
If caught early and properly managed, many patients experience stabilization or improvement in vision. However, outcomes depend on the underlying cause, severity, and speed of intervention.
Key Takeaways
- Retinal bleeding is a potentially sight-threatening event that highlights not only eye health, but systemic vascular health.
- Early symptoms may be subtle or absent, reinforcing the value of routine eye screening—especially in high-risk groups.
- Management is multidisciplinary, addressing the eye and underlying systemic conditions to safeguard vision.
References
- Australian BrightSight. “Retinal Bleeding: Symptoms, Causes, Diagnosis & Treatment.” June 18, 2025.
- All About Vision. “Retinal Hemorrhage and Retinal Bleeding.” Reviewed August 28, 2021.
- YouTube: “Retinal Bleeding: A Closer Look at Sight’s Silent Assassin.”
References
- https://brightsight.com.au/2025/06/18/retinal-bleeding/
- https://www.youtube.com/watch?v=YIeSrHzFQTY
- https://www.allaboutvision.com/conditions/retinal-hemorrhage/
- https://www.medicalnewstoday.com/articles/retinal-hemorrhage
- https://www.healthline.com/health/eye-health/vitreous-hemorrhage
- https://www.ncbi.nlm.nih.gov/books/NBK560777/
- https://patient-rvo.vision-relief.com/introduction/what-is-retinal-vein-occlusion/
- https://my.clevelandclinic.org/health/diseases/25106-retinal-hemorrhage
- https://louisianaretina.com/retinal-hemorrhage-treatment-in-louisiana/
Read full bio of Sneha Tete












