Retinal Artery Occlusion: Causes, Symptoms, Risks, and Treatment
Retinal artery occlusion is a sudden eye emergency that can lead to vision loss if not treated quickly and effectively.
What Is Retinal Artery Occlusion?
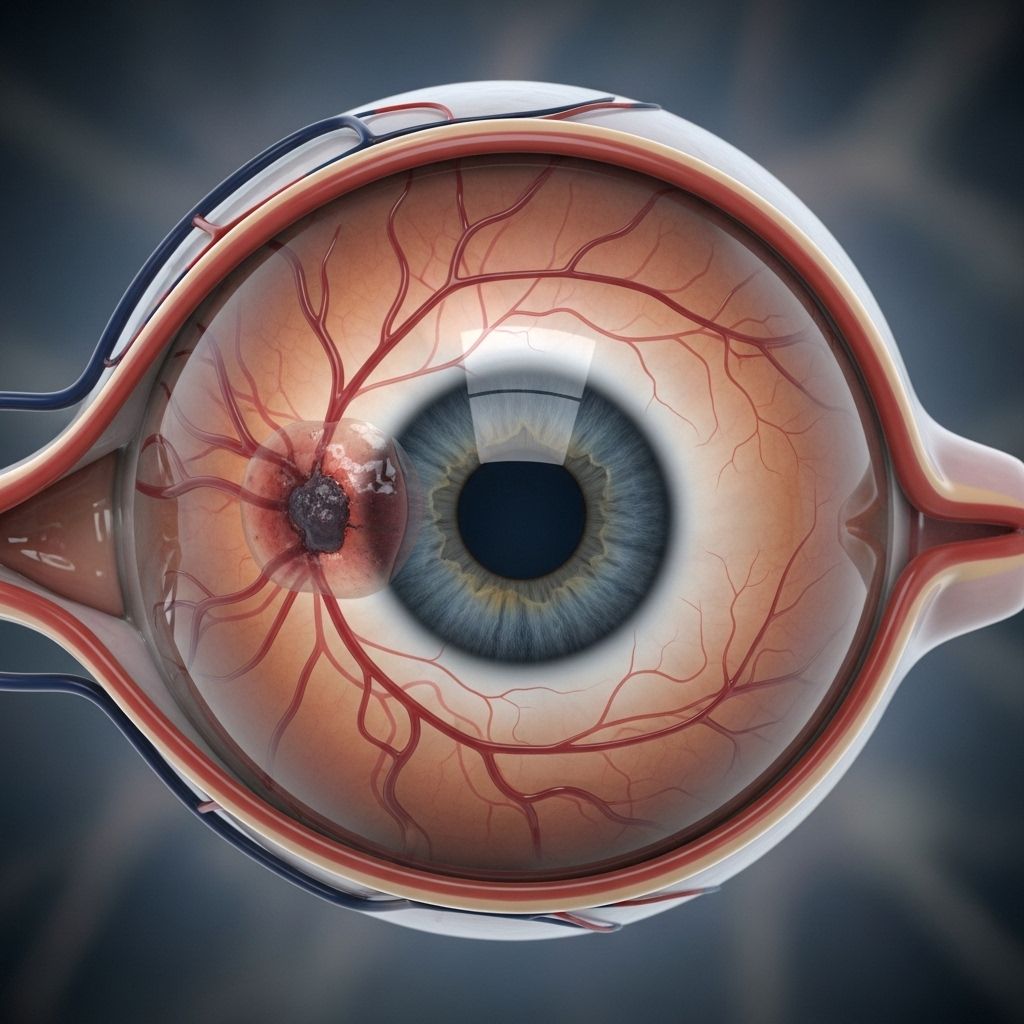
Retinal artery occlusion (RAO) is a serious ophthalmologic emergency caused by a blockage in one of the blood vessels supplying the retina—the thin layer of tissue at the back of your eye that translates light into neural signals for vision. This blockage interrupts the flow of oxygen-rich blood, leading to sudden and often severe vision loss. Prompt diagnosis and intervention are critical, as the retina is highly sensitive to oxygen deprivation and even brief interruptions can result in permanent visual impairment.
Understanding the Retina and its Blood Supply
The retina receives blood supply from small arteries branching off the ophthalmic artery, the main blood vessel for the eye. The two main arteries involved are:
- Central retinal artery: Supplies most of the inner retinal tissue.
- Branch retinal arteries: Supply specific segments or quadrants of the retina.
Any interruption to these vessels can seriously impede retinal function. Most loss of vision results from blocked blood flow to these critical arteries.
Types of Retinal Artery Occlusion
Retinal artery occlusions are classified by which vessel is blocked:
- Central Retinal Artery Occlusion (CRAO): Blockage of the central retinal artery, usually resulting in severe, sudden, and painless vision loss in one eye. CRAO is considered a type of ocular stroke and may also indicate increased risk of cerebral stroke. About 1 in 100,000 people develop CRAO each year, most commonly older adults in their 60s.
- Branch Retinal Artery Occlusion (BRAO): Blockage in one of the smaller branch arteries, often causing loss of vision that only affects part of the visual field, such as loss of peripheral or central vision, depending on which branch is involved. Some people may not notice symptoms if the area of the retina affected is small or not central.
- Cilioretinal Artery Occlusion: In a smaller percentage of individuals, an accessory artery called the cilioretinal artery supplies part of the retina. If this vessel is present and not blocked, central vision may be preserved even if other arteries are affected.
Comparison Table: CRAO vs. BRAO
| Feature | CRAO | BRAO |
|---|---|---|
| Blood vessel affected | Central retinal artery | Branch retinal artery |
| Extent of vision loss | Severe, usually entire eye | Partial, corresponding to affected retinal area |
| Onset of symptoms | Sudden, painless | Sudden, painless |
| Risk of permanent vision loss | Very high | Varies (less if peripheral) |
| Prognosis | Often poor | Depends on area affected |
Causes of Retinal Artery Occlusion
The overwhelming cause of retinal artery occlusion is a blockage—most commonly a blood clot (thrombus or embolus) that stops blood from flowing freely through the artery. Other materials that can cause blockages include cholesterol fragments and calcium deposits.
Where do these clots or blockages originate? Most emboli that cause RAO come from elsewhere in the body, such as:
- Carotid arteries in the neck (atherosclerosis, arterial plaque)
- Heart (from abnormal rhythms, heart valve disease, or heart attacks)
- Aorta, the body’s main artery
Occasionally, the blockage is related to vessel wall inflammation—a process called arteritis.
Other Less-Common Causes
- Fat deposits entering the bloodstream after injuries
- Rare inherited clotting disorders
- Vasculitis such as giant cell arteritis (GCA)
- Blood hyperviscosity states (e.g., polycythemia vera, sickle cell disease)
Risk Factors for Retinal Artery Occlusion
Several health and lifestyle factors may increase your risk of developing RAO. The primary risk factors are:
- High blood pressure (hypertension)
- Aging, especially age 60 and above
- Male sex
- Smoking
- Obesity
- Diabetes
- Abnormal cholesterol levels (hyperlipidemia)
- Heart disease such as atrial fibrillation and valvular disease
- Narrowing of the carotid artery (carotid artery disease)
- Clotting disorders (hereditary or acquired)
- Lung disease
- Autoimmune and vasculitic diseases (especially giant cell arteritis/temporal arteritis)
Symptoms of Retinal Artery Occlusion
Symptoms depend on the location and extent of the arterial blockage, but classic features include:
- Sudden, painless loss of vision in one eye
- Entire field (CRAO)
- Partial field (BRAO)—such as loss of peripheral or central vision
- Visual loss typically develops rapidly, often over seconds to minutes. Some people describe a “curtain” coming down over their vision.
- Vision loss is usually permanent, though rare cases of spontaneous improvement occur.
- If vision loss is brief and then reverses (amaurosis fugax), this can indicate a temporary embolism—a warning sign of a possible future stroke.
Pain is rare. The other eye is typically not affected unless there are simultaneous underlying causes.
How Is Retinal Artery Occlusion Diagnosed?
Diagnosing retinal artery occlusion is an urgent, in-person, clinical process. Timeliness is crucial, as some interventions may be most effective within the first hours after symptom onset.
- History and physical exam: Sudden, painless vision loss is a key feature. The doctor will ask about risk factors and prior symptoms like transient vision changes.
- Ophthalmic examination: Eye doctors (ophthalmologists) use a slit-lamp and dilated eye exam to visualize the retina and its blood vessels.
- Retinal findings may include:
- Retina appearing pale and swollen
- Cherry-red spot at the macula (classic in CRAO)
- Visible embolus at artery branch point (less common)
- Additional tests may include:
- Fluorescein angiography (a dye test to assess blood flow in the retina)
- Optical coherence tomography (OCT) to measure retinal swelling
- Blood tests and imaging to look for underlying causes (e.g., carotid ultrasound, echocardiography, and evaluation for clotting disorders or GCA)
Complications and Prognosis
Retinal artery occlusion is a true ocular emergency. Rapid and irreversible damage can occur to the sensitive nerve tissue of the retina; central vision is often permanently lost. Even with prompt intervention, the prognosis for vision recovery is typically poor, especially in CRAO.
Potential complications include:
- Permanent vision loss in the affected eye
- ∗Increased risk of ischemic stroke∗ in the brain, particularly in the days and weeks following a CRAO
- Neovascular glaucoma (in rare, severe cases)
- Retinal and optic nerve atrophy due to prolonged lack of blood flow
Treatment Options for Retinal Artery Occlusion
Currently, no treatment has been proven to reliably restore vision once a major artery to the retina has been blocked for more than a short window of time. Still, several therapies may be attempted, particularly if the patient presents within a few hours of symptom onset.
- Ocular massage: Gentle pressure on the closed eyelid may help dislodge the blockage and restore blood flow.
- Anterior chamber paracentesis: Removing a small amount of fluid from the front of the eye can lower intraocular pressure and possibly shift the embolus downstream, affecting less critical tissue.
- Inhalation of carbon dioxide/oxygen mixture: This increases carbon dioxide in the blood, causing dilation of retinal arteries and potentially encouraging blood flow around the blockage.
- Medications to lower eye pressure: Eye drops or oral medications may be used to decrease intraocular pressure.
- Hyperbaric oxygen therapy: This is sometimes considered if available, as it may provide additional oxygen to the retina through the choroidal circulation.
- Addressing underlying causes: Evaluating and managing risk factors (hypertension, diabetes, high cholesterol, atrial fibrillation, carotid artery disease) is critical for secondary prevention, as RAO is a risk factor for future strokes.
- Treating vasculitis: If GCA/temporal arteritis is suspected (especially in elderly patients with headache, jaw pain, scalp tenderness), high-dose corticosteroids may be urgently indicated to preserve vision in both eyes.
Despite these interventions, vision often does not return to normal. Rehabilitation and visual aids may be necessary for long-term management.
What to Do if You Suspect Retinal Artery Occlusion
Retinal artery occlusion is a medical emergency. If you or someone else experiences sudden, painless vision loss in one eye, seek immediate medical attention. Fast action can help diagnose the cause, initiate treatments that may preserve vision, and prevent further complications like a stroke.
Preventing Retinal Artery Occlusion
While retinal artery occlusion cannot always be prevented, lowering your risk factors can reduce the likelihood of occurrence. Preventive measures include:
- Managing high blood pressure, cholesterol, and diabetes
- Maintaining a healthy weight and engaging in regular physical activity
- Not smoking
- Following your doctor’s advice regarding cardiovascular health and regular check-ups
- Reporting any symptoms of transient vision loss immediately
Treating underlying cardiovascular, clotting, or inflammatory conditions can also help reduce the risk of recurrence.
Frequently Asked Questions (FAQs)
What is the main difference between central and branch retinal artery occlusion?
CRAO affects the main artery leading to severe, global vision loss in one eye. BRAO blocks a smaller vessel, leading to partial or sometimes unnoticed vision loss.
Is retinal artery occlusion painful?
No, the onset of vision loss is characteristically sudden and painless.
Can vision be restored after retinal artery occlusion?
Sometimes vision improves, but permanent vision loss is common, especially in CRAO. Treatments are largely aimed at preventing further damage and underlying causes.
Who is most at risk?
Older adults, males, individuals with high blood pressure, smokers, and people with underlying cardiovascular risk factors are most at risk.
How is retinal artery occlusion different from a retinal vein occlusion?
Retinal vein occlusion is caused by blockage of the blood vessel carrying blood away from the retina, while artery occlusion involves arteries bringing blood to the retina. Both cause vision loss but have different risk factors and management approaches.
Summary Table: Key Facts About Retinal Artery Occlusion
| Aspect | Details |
|---|---|
| Pathology | Blockage of a retinal artery cutting off blood and oxygen to retinal tissue |
| Symptoms | Sudden, painless vision loss (partial or complete) |
| Main Risk Factors | Age, male sex, hypertension, heart disease, clotting disorders |
| Diagnosis | Clinical history & eye exam; retinal imaging; vascular evaluation |
| Treatment | Often limited; eye massage, lowering eye pressure, addressing risk factors |
| Prognosis | Generally poor for vision recovery—prevention and risk management are critical |
| Emergency? | Yes—requires urgent medical attention |
References
- https://medlineplus.gov/ency/article/001028.htm
- https://www.ahajournals.org/doi/10.1161/STR.0000000000000366
- https://www.healthline.com/health/eye-health/retinal-artery-occlusion
- https://www.asrs.org/patients/retinal-diseases/32/central-retinal-artery-occlusion
- https://eyewiki.org/Retinal_Artery_Occlusion
- https://my.clevelandclinic.org/health/diseases/24127-eye-stroke
- https://www.aurorahealthcare.org/services/eye-care/retinal-artery-occlusions
- https://www.ncbi.nlm.nih.gov/books/NBK470354/
Read full bio of medha deb












