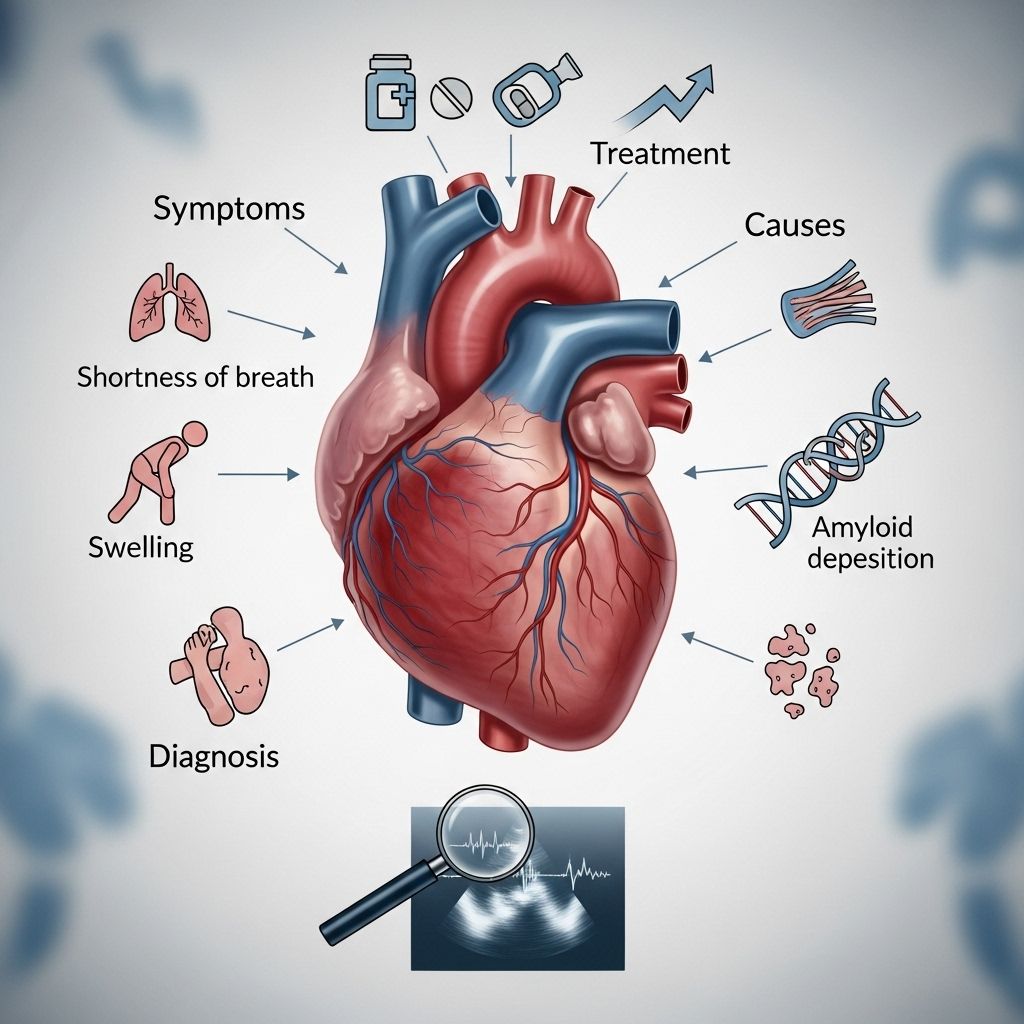
Restrictive Cardiomyopathy: Understanding Symptoms, Causes, Diagnosis, and Treatment
Everything you need to know about restrictive cardiomyopathy, from symptoms to treatment and living well with this rare heart disease.
Restrictive Cardiomyopathy Overview
Restrictive cardiomyopathy is a rare form of heart disease that affects how the ventricles—the heart’s lower chambers—function. Unlike other cardiomyopathies, the ventricular walls in restrictive cardiomyopathy become stiff and cannot expand normally, making it difficult for the heart to fill with blood. This leads to reduced blood flow and can eventually result in heart failure.
What Is Restrictive Cardiomyopathy?
In restrictive cardiomyopathy (RCM), the primary problem is that the muscles of the heart’s ventricles become rigid, typically due to the buildup of abnormal tissue such as scar tissue, abnormal proteins, or iron deposits.
While the heart’s pumping ability may remain normal during the early stages, the inability of the ventricles to relax and fill adequately with blood leads to compromised cardiac output over time. The atria—the upper chambers—often become enlarged as a result, and the heart’s ability to circulate blood deteriorates gradually.
- RCM is the least common form of cardiomyopathy.
- It can affect either or both ventricles.
- Blood flow issues can lead to complications such as heart failure and arrhythmias.
Symptoms of Restrictive Cardiomyopathy
Symptoms of restrictive cardiomyopathy vary widely. Some individuals may not experience any symptoms for years and can lead a nearly normal life. Others may have progressively worsening symptoms as heart function declines.
- Shortness of breath — may begin during exercise but can progress to being present even at rest
- Fatigue
- Swelling (edema) in the legs and feet
- Palpitations (fluttering chest sensation due to abnormal heart rhythms)
- Chest pain or pressure
- Inability to exercise
- Weight gain (sometimes due to fluid buildup)
- Nausea, bloating, poor appetite
- Fainting (syncope)
Symptoms can appear at any age and often worsen as ventricular stiffness increases.
Causes of Restrictive Cardiomyopathy
The exact cause of restrictive cardiomyopathy is often unknown (idiopathic), but several precipitating conditions are recognized. There are multiple mechanisms leading to the stiffening of the ventricular walls. These include deposits of abnormal substances, scarring, or infiltration by cells and proteins.
- Amyloidosis — buildup of misfolded proteins in heart tissue
- Hemochromatosis — excessive iron accumulation in heart muscle
- Scar tissue formation — can follow radiation, chemotherapy, or unknown mechanisms
- Post-heart transplant complications
- Cancer treatments — especially chest radiation and chemotherapy
- Other infiltrative diseases — such as sarcoidosis (inflammatory cell deposition) and scleroderma
- Endomyocardial fibrosis — scarring of the heart lining
- Tumors — in rare cases
Restrictive cardiomyopathy can also result from hereditary conditions or after exposure to certain toxins and drugs. Sometimes it occurs secondary to other diseases affecting the whole body or specific organs.
Types of Restrictive Cardiomyopathy
- Non-infiltrative: Scarring or fibrosis without abnormal substance deposits
- Infiltrative: Amyloidosis, sarcoidosis, or similar conditions with deposits in tissue
- Storage diseases: Accumulation of substances such as iron (hemochromatosis)
- Endomyocardial disorders: Involvement of the heart’s inner lining, such as Loeffler syndrome
Diagnosis of Restrictive Cardiomyopathy
Diagnosis can be challenging, as restrictive cardiomyopathy shares some symptoms with other heart diseases, particularly constrictive pericarditis. A careful evaluation is necessary to distinguish between these conditions and to identify the underlying cause.
The diagnostic process typically involves:
- Detailed history and physical examination
- Blood tests — to check for markers of inflammation, iron levels, abnormal proteins, etc.
- Electrocardiogram (ECG) — records the electrical activity of the heart and detects abnormal rhythms
- Chest X-ray — looks for changes in heart size and shape
- Echocardiogram — uses ultrasound to visualize heart structure and function, assess ventricular rigidity and filling, and measure chamber sizes
- Exercise stress test — evaluates the heart’s response to physical activity
- Cardiac catheterization — provides detailed information on heart pressures and blood flow
- Imaging studies — CT scan or MRI for enhanced heart visualization and assessment of tissue infiltration
- Myocardial biopsy — in select cases, a tissue sample from the heart is analyzed under a microscope to identify abnormal cells or deposits
An accurate diagnosis not only confirms restrictive cardiomyopathy but also clarifies whether it is due to infiltrative or non-infiltrative processes and reveals any treatable underlying causes.
| Test | Purpose | Findings in RCM |
|---|---|---|
| Echocardiogram | Heart structure and wall motion | Thickened/rigid ventricles, enlarged atria |
| ECG | Heart rhythm | Arrhythmias, conduction abnormalities |
| Chest X-ray | Size and shape of heart | Enlarged heart, pulmonary congestion |
| Blood tests | Detect systemic causes | Abnormal proteins, iron overload, inflammation markers |
| Cardiac catheterization | Hemodynamics | Abnormal filling pressures |
| MRI/CT | Tissue characterization | Fibrosis, infiltrative deposits |
| Biopsy | Microscopic tissue analysis | Amyloid, iron, inflammatory cells |
Treatment of Restrictive Cardiomyopathy
Treatment for restrictive cardiomyopathy focuses on managing symptoms and, wherever possible, addressing the underlying cause. Because the condition often results from other diseases, the best therapy depends on the specific root cause identified.
General Treatment Strategies
- Lifestyle modifications
- Medications to control symptoms
- Treatment of underlying disease
- Advanced interventions (e.g., heart transplant in severe cases)
Lifestyle Modifications
- Dietary changes: Reducing sodium intake helps limit fluid retention and eases heart workload. Adhering to recommended dietary restrictions is vital, even when symptoms stabilize.
- Tailored exercise plans: While mild physical activity is generally beneficial, patients must exercise within their tolerance, resting often and avoiding heavy weightlifting. Exercising at times of peak energy and progressive training are recommended.
Medications
- Diuretics: Reduce fluid buildup, improve breathing and decrease swelling
- Beta-blockers and ACE inhibitors: Help manage heart rate and blood pressure; may be useful for certain patients
- Aldosterone inhibitors and digoxin: Sometimes used if symptoms persist
- Blood thinners: Used if blood clots or atrial fibrillation occur
- Medication for specific causes: Drugs to treat iron overload or abnormal protein deposits (e.g., tafamidis for amyloidosis, chemotherapeutic agents in select cases)
- Antiarrhythmics: Manage abnormal heart rhythms
Treating Underlying Conditions
- If restrictive cardiomyopathy is secondary to another disease (e.g., amyloidosis, sarcoidosis, hemochromatosis), treatment of that disease is essential and may involve immunosuppressive therapy, iron removal, or medications targeting abnormal proteins.
- Cancer treatments may need adjustment or cessation if cardiac damage is detected.
Surgical & Advanced Therapies
- Heart transplant: Considered if heart function deteriorates despite all other treatments, and symptoms remain severe
- Liver transplantation: May be offered in rare cases of systemic diseases affecting the heart and liver
Many treatments remain investigational. The main goal is to control symptoms, slow disease progression, and maintain quality of life.
Prognosis and Complications
The prognosis for restrictive cardiomyopathy depends on the underlying cause, disease progression, and response to therapy. Severe forms can lead to heart failure, pulmonary hypertension, arrhythmias, and multi-organ involvement. With optimal care, some patients may maintain stable heart function for years, while others may require advanced treatments.
Living with Restrictive Cardiomyopathy
- Follow healthcare provider recommendations closely and attend regular check-ups.
- Monitor symptoms and report any changes such as increased swelling, fatigue, or chest pain.
- Stay physically active within the limits prescribed by your doctor.
- Eat a heart-healthy, low-sodium diet as instructed.
- Take medications exactly as prescribed and do not discontinue them without medical advice.
- Ask about screening family members if a hereditary cause is suspected.
Frequently Asked Questions About Restrictive Cardiomyopathy
What is the main difference between restrictive and other cardiomyopathies?
Restrictive cardiomyopathy is characterized primarily by ventricular stiffness, not by thickening (hypertrophy) or enlargement (dilation) of heart muscles as seen in other types. The heart’s filling phase (diastole) is most affected, causing poor blood flow.
Can restrictive cardiomyopathy be cured?
There is currently no cure for restrictive cardiomyopathy, but many causes can be managed, and symptoms controlled to improve quality of life. Treatment is tailored to each patient and underlying condition.
Is restrictive cardiomyopathy hereditary?
Some causes, such as certain storage diseases, may be hereditary. Amyloidosis and hemochromatosis have genetic forms, so family screening may be recommended.
Can I exercise with restrictive cardiomyopathy?
Most patients can perform mild to moderate exercise, with medical guidance. Regular activity may help improve endurance and well-being, but high-intensity or strenuous activities may be unsafe.
What should I do if I notice new or worsening symptoms?
Contact your healthcare provider promptly, as worsening symptoms may indicate arrhythmias, worsening heart failure, or another complication requiring treatment adjustments.
When to Contact a Medical Professional
- Persistent or worsening shortness of breath
- Swelling in the legs or abdomen
- Unexplained chest pain or pressure
- Sudden weight gain (possible fluid retention)
- Palpitations or fainting episodes
Early intervention can prevent complications and optimize outcomes.
Resources for Patients and Families
- American Heart Association – Cardiomyopathy Education and Support
- Heart Failure Society – Patient guides and management tools
- Rare Disease Organizations – Support for rare heart conditions
Restrictive Cardiomyopathy FAQs
Q: Who is at risk for restrictive cardiomyopathy?
A: Those with underlying systemic diseases, a family history of certain heart conditions, or previous cancer treatments are at increased risk.
Q: How is restrictive cardiomyopathy different from constrictive pericarditis?
A: Restrictive cardiomyopathy is caused by stiff heart muscle, while constrictive pericarditis results from a stiff outer heart layer (the pericardium). Both reduce heart’s ability to fill, but have distinct treatments.
Q: What lifestyle changes are most helpful?
A: Reducing sodium in your diet, pacing activity, managing medications, and regular communication with your healthcare team are effective strategies.
Q: Are there support groups for people with restrictive cardiomyopathy?
A: Yes, many heart disease advocacy organizations and hospitals offer support groups for patients and families.
Q: Can restrictive cardiomyopathy progress to heart failure?
A: Yes, untreated or progressive restrictive cardiomyopathy often leads to heart failure and requires complex medical management.
References
- https://www.webmd.com/heart-disease/restrictive-cardiomyopathy
- https://www.pennmedicine.org/conditions/restrictive-cardiomyopathy
- https://www.heart.org/en/health-topics/cardiomyopathy/what-is-cardiomyopathy-in-adults/restrictive-cardiomyopathy
- https://my.clevelandclinic.org/health/diseases/17427-restrictive-cardiomyopathy
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/r/restrictive-cardiomyopathy.html
- https://www.mayoclinic.org/diseases-conditions/cardiomyopathy/symptoms-causes/syc-20370709
- https://www.ncbi.nlm.nih.gov/books/NBK537234/
- https://www.ahajournals.org/doi/10.1161/circresaha.117.310982
- https://health.ucdavis.edu/conditions/restrictive-cardiomyopathy
Read full bio of medha deb












