Renal Parenchymal Disease: Symptoms, Causes, Diagnosis, and Treatment
Understand renal parenchymal disease—its symptoms, causes, diagnosis, and modern management to maintain optimal kidney health.
Renal parenchymal disease is a significant medical condition affecting the structural and functional components of the kidneys. This disorder can have a variety of causes and may result in acute or chronic kidney damage if left unaddressed. Understanding its signs, risk factors, diagnostic approaches, and management strategies is pivotal for timely intervention and preserving long-term kidney health.
What Is Renal Parenchymal Disease?
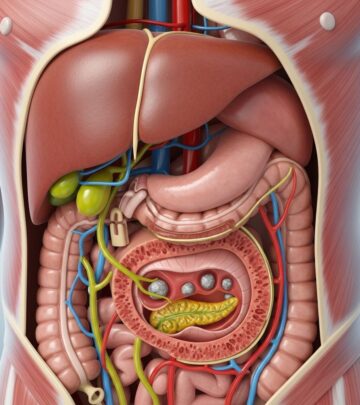
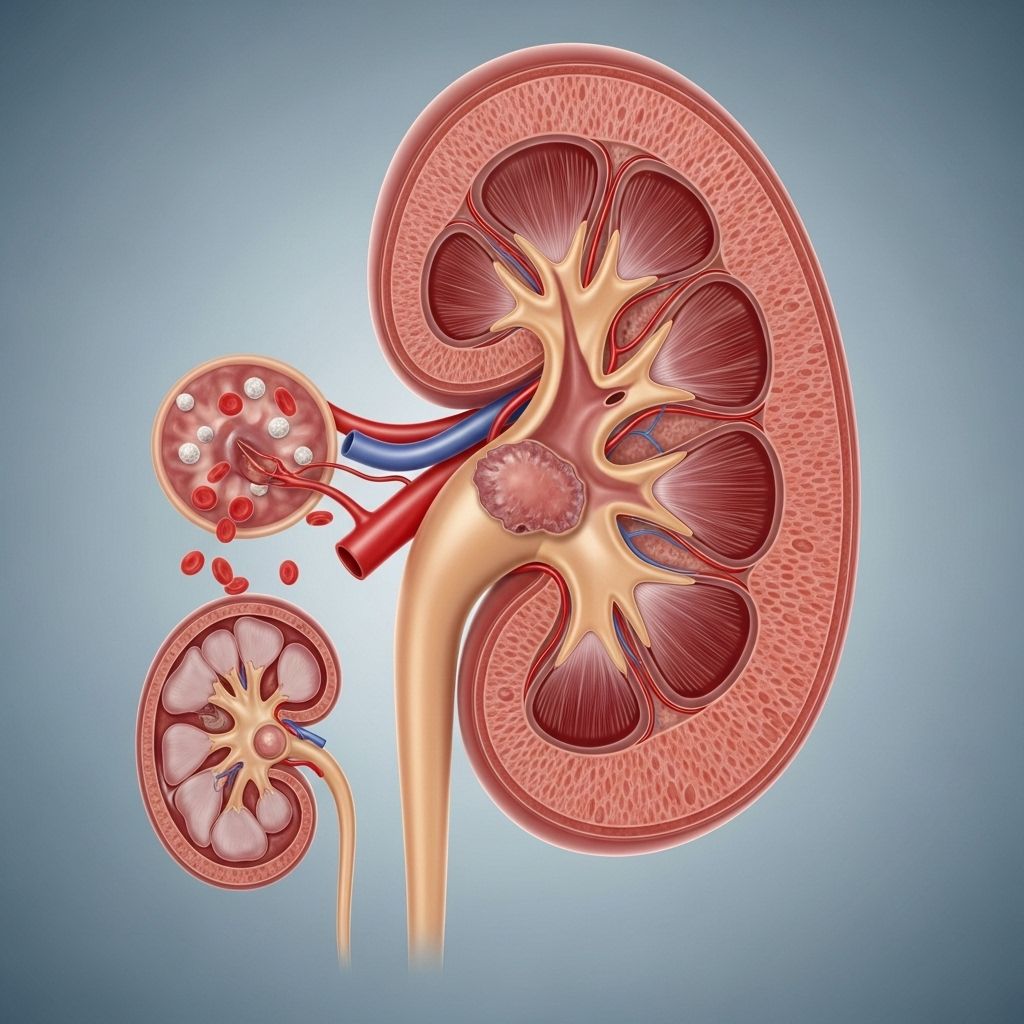
The term renal parenchymal disease covers conditions that damage the parenchyma—the functional tissue of the kidneys, which includes the renal cortex and renal medulla. This tissue contains millions of nephrons responsible for filtering blood, removing waste, balancing electrolytes, and regulating fluids. Injury or disease affecting this area can impair overall kidney function and, if unchecked, may progress to chronic kidney disease (CKD).
Renal parenchymal disease can be classified as either acute or chronic:
- Acute renal parenchymal disease develops rapidly, often in response to an immediate event or injury and has the potential to be reversible with timely treatment.
- Chronic renal parenchymal disease evolves over months or years, typically as a result of prolonged illness or repeated kidney insults, and can lead to permanent loss of kidney function.
Symptoms of Renal Parenchymal Disease
Symptoms can vary significantly depending on the severity, duration, and specific part of the kidney affected. Many individuals experience few or no symptoms in the early stages, making early detection challenging. As the condition progresses, symptoms often become more apparent and can include:
- Elevated blood pressure (hypertension)
- Fatigue and persistent tiredness
- Shortness of breath
- Swelling (edema) in the feet, ankles, hands, or face
- Nausea and vomiting
- Loss of appetite
- Decreased urination or changes in urine output
- Visible blood in urine (hematuria)
- Foamy urine
- Dizziness or itching
- Brittle or weakening bones
- Joint discomfort
- Unintentional weight loss
- Confusion or drowsiness (in severe cases)
It’s important to note that not all symptoms need to be present for a diagnosis, and symptoms may worsen gradually as the disease advances.
What Causes Renal Parenchymal Disease?
The causes of renal parenchymal disease are diverse and can include both acquired and hereditary factors. These can be grouped based on whether they are more likely to provoke an acute or chronic presentation:
Acute Causes
- Severe bleeding
- Severe dehydration (prolonged vomiting, diarrhea)
- Acute infections
- Major burns
- Pulmonary embolism (blood clot in the lungs)
- Acute coronary syndromes (heart attacks)
- Septic shock (infection causing dangerously low blood pressure)
- Conditions causing low blood flow to the kidneys
Chronic Causes and Risk Factors
- Diabetes (type 1 and type 2)
- High blood pressure (hypertension)
- Chronic or recurrent kidney infections
- Renal and urinary tract obstructions (e.g., kidney stones)
- Polycystic kidney disease (genetic disorder)
- Congenital (present at birth) kidney conditions or anomalies
- Hereditary kidney diseases
- Prolonged use of nephrotoxic medications (e.g., some NSAIDs, antibiotics)
Certain lifestyle factors and underlying conditions can increase the risk of developing renal parenchymal disease, including obesity, smoking, excessive alcohol use, and a family history of kidney disorders.
How Is Renal Parenchymal Disease Diagnosed?
Diagnosing renal parenchymal disease involves a combination of clinical evaluation, laboratory tests, and imaging studies. A doctor will typically:
- Assess your symptoms and take a detailed medical history
- Perform a physical examination focused on blood pressure, swelling, and overall health
- Order urine tests to check for protein, blood, or cellular casts
- Conduct blood tests to evaluate kidney function (e.g., creatinine, urea, estimated glomerular filtration rate—eGFR)
- Order imaging studies such as renal ultrasound or CT scan to look for structural changes, scarring, or obstructions
- In some cases, arrange for a kidney biopsy to examine tissue directly if the diagnosis remains unclear or to determine the extent of damage
Grading of Renal Parenchymal Disease
Doctors often classify the severity of renal parenchymal disease into different grades using imaging (particularly ultrasound):
| Grade | Description |
|---|---|
| Grade 1 (Mild) | Minimal increase in echogenicity; preserved cortico-medullary differentiation |
| Grade 2 (Moderate) | Moderate increase in echogenicity; slight blurring between cortex and medulla |
| Grade 3 (Severe) | Marked increase in echogenicity; loss of cortico-medullary differentiation |
Grading helps guide treatment planning and prognosis estimation.
Complications of Renal Parenchymal Disease
Untreated or advanced renal parenchymal disease can lead to serious complications, such as:
- Chronic kidney disease (CKD) – progressive loss of kidney function over months or years
- Acute kidney injury (AKI) – sudden decline in kidney function
- Kidney failure (end-stage renal disease) – kidneys can no longer sustain body processes without external support
- Electrolyte imbalances – abnormalities in sodium, potassium, or calcium metabolism
- Dehydration or fluid overload
- Anemia due to reduced production of erythropoietin
- Bone weakening (renal osteodystrophy)
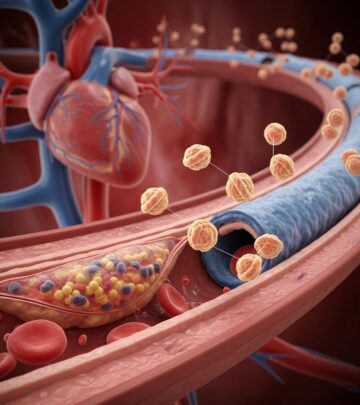
- Cardiovascular complications due to associated hypertension and fluid imbalances
Treatment and Management of Renal Parenchymal Disease
Effective management focuses on controlling symptoms, addressing underlying causes, and minimizing further kidney damage. Treatment options are tailored to individual needs and the severity of disease, and may include:
Lifestyle and Dietary Changes
- Reduce salt intake to help manage blood pressure and fluid retention
- Limit protein consumption if advised, as excessive protein may burden damaged kidneys
- Avoid processed foods, smoking, and excessive alcohol
- Maintain a healthy weight and stay physically active as tolerated
- Monitor and control blood glucose if diabetic
Medications
- Antihypertensive drugs to control high blood pressure (often ACE inhibitors or ARBs)
- Medications to manage cholesterol or reduce proteinuria
- Diuretics for edema
- Iron supplements or erythropoietin for anemia
- Phosphate binders for bone protection
Managing Fluid Retention
- Monitor daily fluid intake, especially if swelling or shortness of breath occurs
- Diuretics or fluid restrictions as prescribed by your doctor
- Regular follow-up to evaluate electrolyte and fluid balance
Advanced Therapies
- Dialysis (hemodialysis or peritoneal dialysis) for advanced kidney failure
- Kidney transplant in suitable candidates with end-stage disease
Early intervention and customized treatment can slow or halt the progression of the disease.
Prevention and Risk Reduction
- Regular health check-ups, especially if you have risk factors like diabetes or hypertension
- Adhering to prescribed medications and disease management if you have chronic illnesses
- Maintaining well-balanced nutrition and a healthy lifestyle
- Avoiding overuse of over-the-counter painkillers and nephrotoxic drugs
- Promptly treating infections or urinary tract problems
- Family screening if there’s a history of inherited kidney disease
Frequently Asked Questions (FAQs)
What is the difference between renal parenchymal disease and chronic kidney disease?
Renal parenchymal disease refers to direct damage or disease affecting the functional tissue of the kidney. Chronic kidney disease (CKD) is a potential result of long-standing renal parenchymal disease where kidney function progressively worsens over time, often requiring more rigorous intervention.
Can renal parenchymal disease be reversed?
Acute forms may be reversible with prompt identification and treatment of the underlying cause. Chronic disease generally causes permanent changes, but early intervention can significantly slow progress and reduce complications.
Who is at the highest risk of developing renal parenchymal disease?
Individuals with longstanding high blood pressure, diabetes, a family history of kidney conditions, recurrent urinary tract infections, or chronic use of nephrotoxic drugs are most at risk.
How often should a person with this condition see a doctor?
People diagnosed with renal parenchymal disease should have regular follow-ups—at intervals decided by their healthcare provider—depending on severity, rate of progression, and presence of associated risks or complications.
Are there early warning signs to watch for?
Early warning signs can be minimal or nonspecific, like tiredness or mild swelling. Any unexplained increase in blood pressure, changes in urinary habits, or presence of blood in urine should prompt medical evaluation.
Takeaway
Renal parenchymal disease encompasses a broad spectrum of conditions affecting the key tissue responsible for kidney filtration. While early forms may go unnoticed, vigilance regarding risk factors, timely diagnosis, and proactive management can preserve kidney function and prevent severe complications. Open communication with a healthcare professional and individualized care plans are central to effective long-term management.
References
- https://healthmatch.io/kidney-disease/parenchymal-disease
- https://ckbirlahospitals.com/rbh/blog/renal-parenchymal-disease-is-it-dangerous
- https://www.healthline.com/health/kidney-disease/renal-parenchymal-disease
- https://www.nicklauschildrens.org/conditions/renal-parenchymal-diseases
- https://www.mayoclinic.org/diseases-conditions/chronic-kidney-disease/diagnosis-treatment/drc-20354527
- https://www.nhs.uk/conditions/kidney-disease/
- https://www.kidneyfund.org/all-about-kidneys/stages-kidney-disease/stage-1-chronic-kidney-disease
Read full bio of Sneha Tete