Hypertrophic Cardiomyopathy: Essential Questions and Answers
Comprehensive answers about hypertrophic cardiomyopathy — causes, symptoms, diagnosis, treatment, lifestyle, and FAQs for better heart health.
Hypertrophic Cardiomyopathy: Answers to Your Most Important Questions
Hypertrophic cardiomyopathy (HCM) is a complex heart condition with significant health impacts. This article covers the most frequently asked questions about HCM, exploring its symptoms, causes, diagnostic strategies, treatment options, prognosis, and tips for living better with HCM. Our goal is to provide reliable, comprehensive information in clear language to empower patients and families.
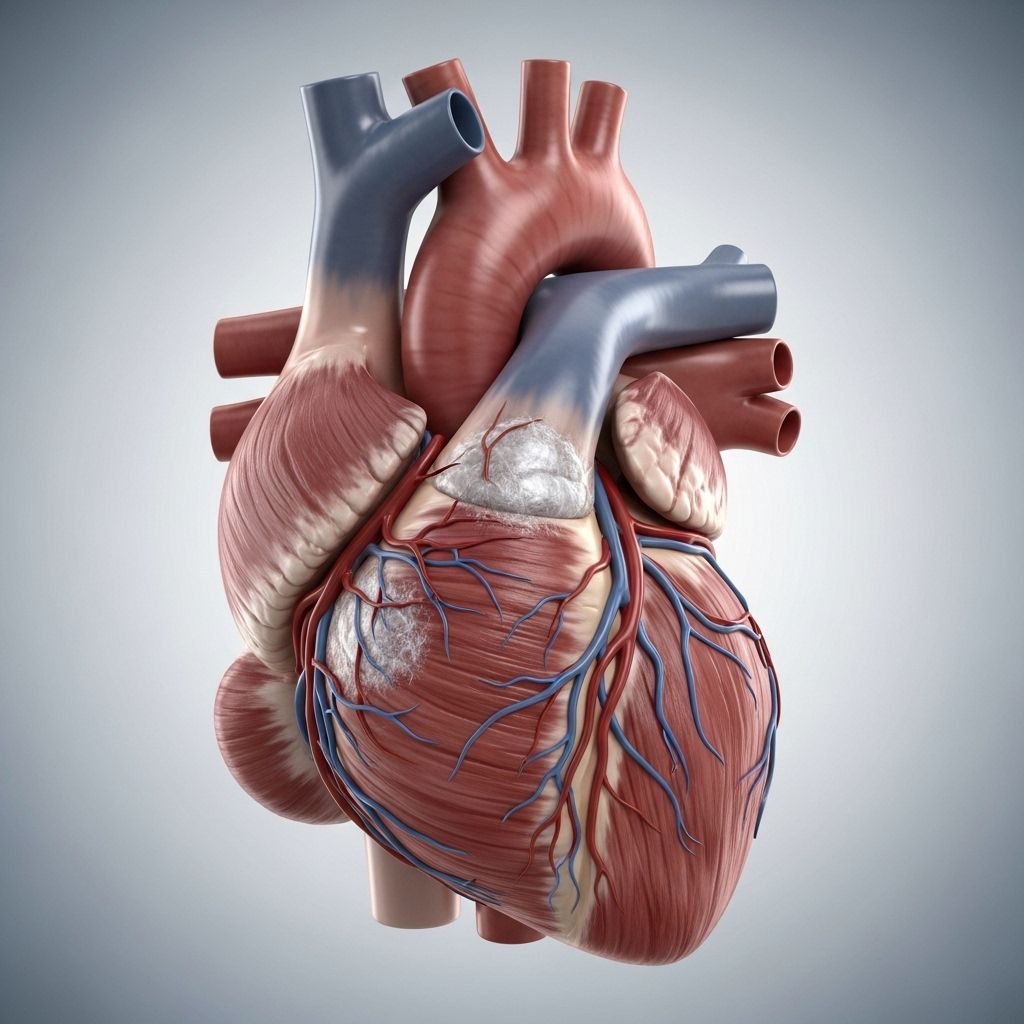
What Is Hypertrophic Cardiomyopathy?
Hypertrophic cardiomyopathy (HCM) is a heart disease characterized by abnormal thickening (hypertrophy) of the heart muscle, usually affecting the left ventricle. This thickening can obstruct blood flow and reduce the heart’s ability to pump efficiently, potentially leading to arrhythmias, heart failure, and, in rare cases, sudden cardiac death.
The primary cause of HCM is genetic mutations — most cases are inherited and linked to changes in genes that encode cardiac muscle proteins.
What Causes HCM?
- Genetics: Most HCM cases are inherited in an autosomal dominant pattern, meaning only one copy of an abnormal gene is needed to develop the condition. Over 27 genes related to cardiac sarcomere structure have been identified.
- Family History: Individuals with family members diagnosed with HCM have a higher risk. Genetic testing and family screening are recommended for first-degree relatives.
- Other Factors: While in rare instances HCM can occur spontaneously due to a new genetic mutation, most cases involve hereditary transmission.
What Are the Symptoms of HCM?
Symptoms can vary greatly from person to person; many individuals remain asymptomatic, while others may experience pronounced difficulties. Symptoms may develop gradually over time, sometimes making them hard to recognize.
- Shortness of breath (dyspnea), especially with physical activity
- Chest pain or pressure, often resembling angina
- Palpitations (awareness of rapid or irregular heartbeats)
- Fatigue, reduced exercise tolerance
- Dizziness or fainting (syncope), particularly during exertion
- Swelling in the legs or abdomen (in advanced cases)
Notably, the most serious complication is sudden cardiac death, usually caused by dangerous arrhythmias, particularly in young and asymptomatic individuals.
How Is HCM Diagnosed?
- Physical Exam: May detect a heart murmur or abnormal sounds.
- Electrocardiogram (ECG): Records electrical activity and may show patterns suggestive of HCM.
- Echocardiogram: This ultrasound imaging is essential in measuring wall thickness and evaluating blood flow obstruction.
- Cardiac MRI: Provides detailed images to assess the extent and pattern of hypertrophy.
- Exercise Stress Testing: Assesses how the heart responds to physical exertion and can uncover arrhythmias or symptoms not apparent at rest.
- Genetic Testing: Especially important for confirming diagnosis in families with known HCM.
Often, HCM is discovered incidentally—during routine screening or when patients present with related symptoms or family history.
Types of Hypertrophic Cardiomyopathy
- Obstructive HCM (HOCM): Thickened heart muscle obstructs blood flow from the left ventricle to the aorta.
- Non-Obstructive HCM (HNCM): The heart muscle is thickened, but there is no significant obstruction to blood flow.
Identifying which type a patient has determines appropriate treatment and risk assessment strategies.
What Are the Risk Factors for HCM?
- Family history of HCM or sudden cardiac death
- Certain genetic mutations (detectable by genetic screening)
- Young age: While HCM can occur at any age, complications such as arrhythmias are especially concerning in younger patients
- Male gender: Some studies suggest higher prevalence and risk of complications in men
Patients should discuss risk factors with their healthcare team for personalized screening and management.
How Is HCM Treated?
The goals of treatment are to relieve symptoms, minimize risks (especially sudden cardiac death), and improve quality of life. Treatment is tailored based on symptom severity, the presence of obstruction, arrhythmias, and individual risk profile.
Medications
- Beta-blockers (e.g. metoprolol, propranolol, atenolol): Slow the heart rate and decrease contractility, making it easier for the heart to pump blood.
- Calcium channel blockers (e.g. verapamil, diltiazem): Relax heart muscle and reduce symptoms.
- Mavacamten (Camzyos): A newer medication specifically approved for symptomatic obstructive HCM in adults; reduces strain on the heart when conventional medicines can’t be used.
- Heart rhythm medications (e.g. amiodarone, disopyramide): Help control arrhythmias.
- Blood thinners (e.g. warfarin, dabigatran, rivaroxaban, apixaban): Reduce the risk of blood clots, particularly if atrial fibrillation is present.
Procedures and Surgeries
- Septal myectomy: An open-heart surgery removing part of the thickened septum to restore blood flow. Considered the gold standard for septal reduction; usually reserved for patients not responding to medical therapy.
- Alcohol septal ablation: A less invasive, catheter-based procedure used for high-risk or surgery-averse patients. Doctors inject alcohol into a targeted area to reduce septal thickness by causing a controlled, localized heart attack.
- Apical myectomy: For selective cases where thickening affects the heart’s apex (tip).
- Internal cardiac defibrillator (ICD) implantation: For patients at high risk of life-threatening arrhythmias or sudden cardiac death.
- Heart transplantation: Rare, final option for those with end-stage heart failure unresponsive to other treatments.
Managing Co-Existing Conditions
- Treatment of related heart conditions (e.g., coronary artery disease, hypertension, hyperlipidemia)
- Management of sleep apnea
What Is the Prognosis for HCM?
The prognosis for HCM varies. Most patients live normal or near-normal lives, especially when the disease is detected early and managed appropriately. However, some may develop serious complications, such as arrhythmias, heart failure, or sudden cardiac death. Close monitoring and individualized risk assessment are crucial.
- With proper medical management and regular follow-up, the risk of serious outcomes can be greatly reduced.
- Individuals with a high risk profile (young age, history of fainting, family history of sudden cardiac death, severe thickening) require more stringent monitoring and consideration for an ICD.
How Can You Lower Your Risk or Prevent HCM-Related Complications?
- Regular follow-ups with a cardiologist familiar with HCM
- Genetic screening for first-degree relatives
- Compliance with medications and recommended therapies
- Awareness of symptom changes (such as new or worsening chest pain, fainting, palpitations)
- Healthy lifestyle choices:
- Avoiding excessive or very strenuous exercise (may increase risk of arrhythmias)
- Managing weight, blood pressure, and cholesterol
- Avoiding dehydration, which can worsen obstruction
- Limiting alcohol and avoiding recreational drugs
- Smoking cessation
Discuss exercise and lifestyle recommendations with your cardiology team. Individual advice varies with severity of disease and risk profile.
How Does HCM Affect Daily Life?
Living with HCM often requires some adjustments. Most individuals can lead active lives but may need to tailor exercise routines, monitor for symptoms, and keep up with regular cardiology assessments.
- Inform coaches, teachers, or activity coordinators about your condition.
- Set realistic expectations and learn to listen to your body.
- Know the symptoms that require urgent medical attention: sudden chest pain, fainting, palpitations, or extreme shortness of breath.
- Maintain mental and emotional wellbeing. Consider support groups or counseling if HCM causes anxiety or lifestyle limitations.
How Should Family Members Be Involved?
- Genetic testing and screening for all first-degree relatives
- Education about warning signs of HCM and sudden cardiac death
- Support in maintaining healthy lifestyle habits
- Participation in regular checkups if a familial mutation is identified
Frequently Asked Questions (FAQs) About Hypertrophic Cardiomyopathy
Q: Can I exercise with HCM?
A: Exercise is generally safe for many HCM patients, but high-intensity or competitive sports may not be advisable, especially with obstruction or risk factors present. Consult your cardiologist for individualized recommendations.
Q: Is HCM curable?
A: HCM is currently not curable, but it is manageable. Early diagnosis and appropriate treatment allow most people to live normal or near-normal lives.
Q: Can children get HCM?
A: Yes. While HCM is often diagnosed in adults, children and adolescents can also be affected, especially in families with genetic mutations. Pediatric evaluation is recommended for at-risk children.
Q: What is the difference between dilated and hypertrophic cardiomyopathy?
A: Dilated cardiomyopathy involves thinning and stretching of the heart muscle, leading to a weakened pump. Hypertrophic cardiomyopathy involves thickening of heart muscle, potentially obstructing flow and leading to arrhythmias.
Q: Should my family get genetic testing if I’m diagnosed with HCM?
A: Yes. Genetic testing is recommended for first-degree relatives, as it helps detect risk early and guides monitoring.
Q: Are all medications safe for people with HCM?
A: Some medications, such as certain blood pressure drugs or stimulants, may worsen symptoms in HCM. Treatment should always be guided by a cardiologist familiar with the disease — never discontinue or start medications without consulting your specialist.
Q: What symptoms require immediate medical attention?
- Sudden fainting or loss of consciousness
- Severe or sudden chest pain
- Increased palpitations or rapid heartbeat
- Severe shortness of breath or swelling
If you experience these symptoms, contact emergency services immediately, as these may signal a life-threatening arrhythmia or cardiac event.
Hypertrophic Cardiomyopathy: Quick Reference Comparison Table
| Feature | Obstructive HCM (HOCM) | Non-Obstructive HCM (HNCM) |
|---|---|---|
| Blood Flow Obstruction | Present; may cause symptoms | Absent |
| Typical Symptoms | Chest pain, shortness of breath, fainting | Milder or absent; can develop later |
| Primary Treatments | Medications, septal myectomy, or ablation | Medications |
| Prognosis | Good with proper management; increased risk if untreated | Generally good; regular monitoring needed |
Key Takeaways for Patients and Families
- HCM is a lifelong condition but usually manageable with the right care and lifestyle adjustments.
- Screening and monitoring are crucial, especially for family members.
- Effective treatments exist for most forms and complications.
- Empowering yourself with knowledge and regular medical care is the best path to optimizing heart health.
Resources and Support
- Ask your healthcare provider about support groups for HCM patients and families.
- Stay informed about HCM research and new treatment approaches.
- Reliable sources include major heart health organizations, patient advocacy groups, and specialized cardiology centers.
References
- https://healthcare.utah.edu/cardiovascular/programs/hypertrophic-cardiomyopathy-program/treatment
- https://www.mayoclinic.org/diseases-conditions/hypertrophic-cardiomyopathy/diagnosis-treatment/drc-20350204
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3078548/
- https://my.clevelandclinic.org/health/diseases/17116-hypertrophic-cardiomyopathy
- https://www.mayoclinic.org/diseases-conditions/hypertrophic-cardiomyopathy/symptoms-causes/syc-20350198
- https://www.heart.org/en/health-topics/cardiomyopathy/what-is-cardiomyopathy-in-adults/hypertrophic-cardiomyopathy
- https://www.pennmedicine.org/conditions/hypertrophic-cardiomyopathy
- https://my.clevelandclinic.org/health/diseases/16841-cardiomyopathy
Read full bio of Sneha Tete












