Pulmonary Thromboendarterectomy: Surgery for Chronic Thromboembolic Pulmonary Hypertension
A comprehensive guide to pulmonary thromboendarterectomy, detailing procedure, risks, preparation, and recovery for treating chronic thromboembolic pulmonary hypertension.
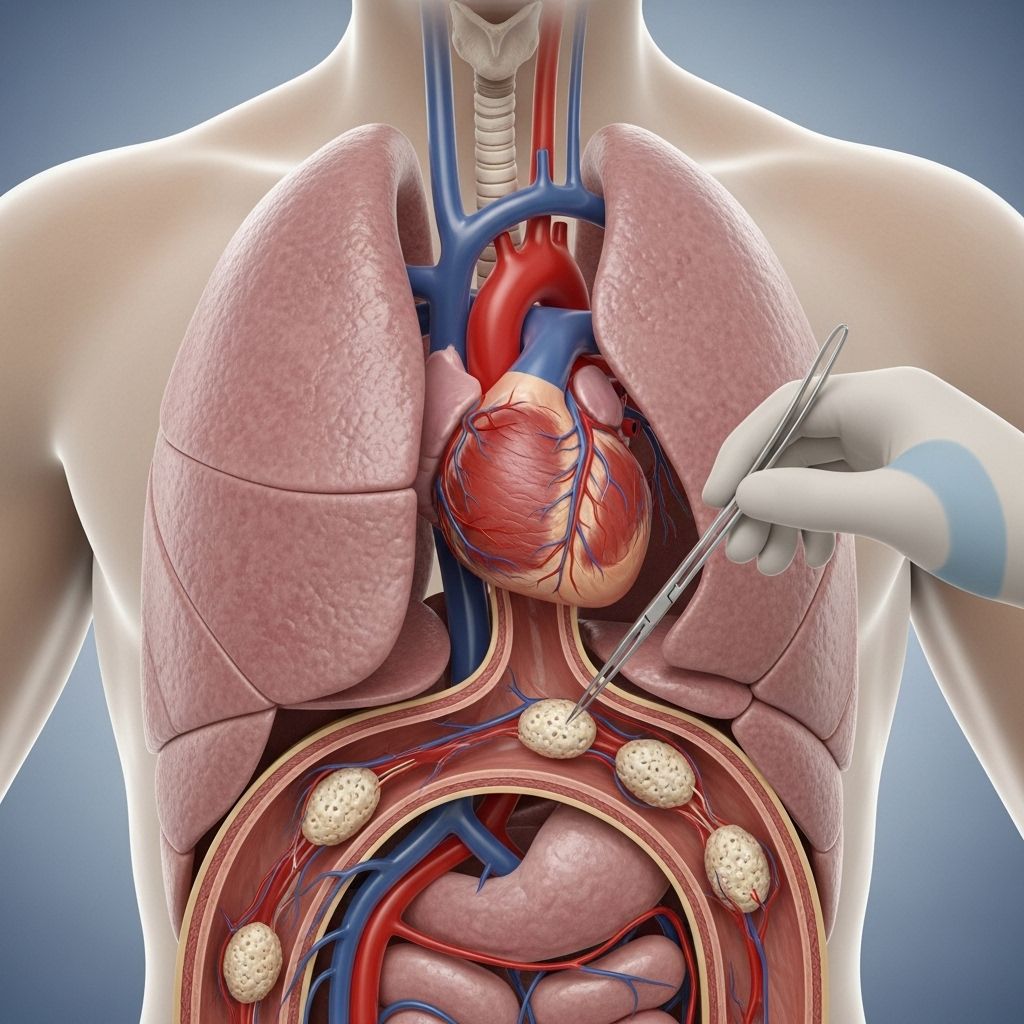
Pulmonary thromboendarterectomy (PTE)—also called pulmonary endarterectomy—is a highly specialized surgical procedure designed to remove chronic blood clots and scar tissue from the pulmonary arteries. This intervention is often considered the only curative treatment for chronic thromboembolic pulmonary hypertension (CTEPH), a rare but severe form of high blood pressure in the lungs caused by persistent blockage of the pulmonary arteries. The goal of this comprehensive guide is to provide an in-depth understanding of PTE, including the condition it treats, the surgical process, preparation, recovery expectations, results, and frequently asked questions.
What Is Pulmonary Thromboendarterectomy (PTE)?
Pulmonary thromboendarterectomy is an open-heart surgery that removes organized blood clots (thrombi) and associated scar tissue from the pulmonary arteries, restoring normal blood flow from the heart to the lungs. By relieving these obstructions, PTE reduces pulmonary artery pressure and improves overall heart and lung function.
- PTE is the definitive treatment for patients with CTEPH who are suitable surgical candidates.
- This procedure is highly specialized and performed only at experienced centers with multidisciplinary teams.
- PTE significantly improves symptoms, quality of life, and survival in eligible patients with CTEPH.
Understanding Chronic Thromboembolic Pulmonary Hypertension (CTEPH)
CTEPH is a rare but serious medical condition where persistent or recurrent blood clots obstruct the pulmonary arteries, leading to elevated blood pressure in these vessels. Over time, this causes the right side of the heart to work harder, potentially resulting in heart failure if left untreated.
| Aspect | Description |
|---|---|
| Cause | Chronic blood clots and associated scar tissue blocking the pulmonary arteries |
| Symptoms |
Understanding the foundational aspects of treatment approaches for pulmonary embolism can equip you with knowledge on managing this critical condition. Discover strategies that target immediate care and long-term solutions, ensuring you can navigate your health with confidence. |
| Risks | Untreated CTEPH can result in right heart failure and death |
| Prevalence | Occurs in about 3% of patients who have had a pulmonary embolism |
Who Needs a Pulmonary Thromboendarterectomy?
The primary reason for undergoing PTE is the diagnosis of CTEPH that has caused significant blockages in the pulmonary arteries and is not responsive to medication alone. Not all patients with CTEPH are suitable candidates; comprehensive evaluation is required to determine eligibility.
- Patients with chronic blood clots in accessible areas of the pulmonary arteries
- Those experiencing moderate to severe symptoms—such as shortness of breath and exercise intolerance—despite optimal medical therapy
- Individuals whose overall health allows them to tolerate major heart and lung surgery
- Patients who do not have other prohibitive medical conditions (such as advanced age, severe comorbidities, or disease located in very small arteries out of reach for surgery)
Careful selection and assessment is essential, involving right heart catheterization, imaging studies (CT, MRI, echocardiogram), and multidisciplinary consultation.
Preparing for Pulmonary Thromboendarterectomy
Preparing for PTE involves a range of preoperative tests and consultations to determine the patient’s eligibility and minimize surgical risk.
Key Steps in Preparation
- Medical Assessment: A complete evaluation of heart and lung function, general health, and the extent/location of clots.
- Imaging:
- CT pulmonary angiography
- Echocardiogram
- Right heart catheterization
- Ventilation/perfusion (V/Q) scan
- Blood tests: Assess kidney, liver, and coagulation function.
- Discussion: The surgeon explains the procedure, expected outcomes, risks, and answers questions; written informed consent is obtained.
- Preparation steps: Patients may need to stop certain medications (such as blood thinners) and fast for a period before surgery.
How Pulmonary Thromboendarterectomy Is Performed
PTE is an extensive open-heart procedure that requires a highly experienced surgical team. The surgery is typically performed under general anesthesia and can last several hours.
Step-by-Step Overview of the Surgical Process
- Incision: A median sternotomy (splitting of the breastbone) is made to provide access to the heart and lungs.
- Cardiopulmonary Bypass: The patient is connected to a heart-lung machine which takes over the function of circulating and oxygenating the blood during the operation.
- Cooling the Body: The patient’s body temperature is lowered to about 18–20°C (64–68°F) to protect organs and brain function during circulatory arrest.
- Controlled Circulatory Arrest: Blood flow is briefly and intermittently stopped (for periods up to 20 minutes at a time) to allow excellent visualization inside the pulmonary arteries, minimizing blood obscuring the surgeons’ view.
- Removal of Clots and Scar Tissue: The surgeon carefully dissects and removes the organized clots and fibrous tissue from both the right and left pulmonary arteries, often working through fine arterial branches.
- Arteriotomy Closure: After the arteries are cleared, they are meticulously sutured closed.
- Rewarming and Restarting the Heart: The body and heart are gradually rewarmed, and normal circulation is restored.
- Completion: The chest is closed and the patient is transferred to the intensive care unit (ICU) for close monitoring and postoperative care.
Surgical Techniques and Considerations
Success depends on complete removal of the obstructing material, proper visualization, careful management of the patient’s temperature, and the skills of an experienced team. Incomplete removal can result in persistent pulmonary hypertension and ongoing symptoms.
Recovery After Pulmonary Thromboendarterectomy
Recovery from PTE surgery takes several weeks to months and involves a staged rehabilitation process. Immediately after the operation, patients remain in the ICU for monitoring and support.
- Hospital Stay: Most patients stay in the hospital for 2–3 weeks post-surgery, with the initial days spent in the ICU for close observation.
- Pain Control: Pain at the surgical site is managed with medications.
- Monitoring:
- Continuous heart and lung monitoring
- Blood pressure and oxygen level checks
- Screening for possible complications
- Rehabilitation: Gradual increase in physical activity and respiratory therapy to regain strength and function.
- Medications: Anticoagulation (blood thinners) is usually continued after surgery to prevent recurrence of clots.
Risks and Complications of Pulmonary Thromboendarterectomy
Every major surgery, especially cardiac procedures like PTE, carries potential risks. However, in experienced centers, mortality rates are low and the majority of patients benefit greatly from the procedure.
Potential Risks Include:
- Infection
- Bleeding
- Arrhythmias (abnormal heart rhythms)
- Kidney injury
- Stroke or neurological effects
- Reperfusion pulmonary edema (fluid in the lungs after reestablishment of blood flow)
- Persistent or recurrent pulmonary hypertension if complete endarterectomy is not achieved
Careful preoperative preparation, surgical expertise, and dedicated postoperative care are critical in minimizing these risks and managing any complications that arise.
Expected Results and Prognosis
Pulmonary thromboendarterectomy can be life-changing for patients with CTEPH. Most individuals experience dramatic improvement in symptoms, exercise capacity, and quality of life. Many are able to discontinue supplemental oxygen and resume normal activities. The procedure is often curative for CTEPH when all obstructing material can be removed.
| Outcome | Details |
|---|---|
| Symptom Relief | Marked reduction or elimination of breathlessness, fatigue, and leg swelling for most patients |
| Survival | Marked improvement compared to patients who do not undergo surgery; 5-year survival exceeding 90% for successful procedures |
| Long-Term Outcomes | Improved heart function, oxygen delivery, and overall quality of life |
| Potential for Recurrence | Rare, but regular follow-up is needed to monitor for new clots or residual pulmonary hypertension |
Living With CTEPH and After PTE Surgery
Patients who have undergone successful PTE often experience tremendous relief from the burden of CTEPH. However, they should remain vigilant about long-term care to optimize surgical results and prevent recurrence.
Self-Care and Monitoring
- Regular follow-up with a cardiologist or pulmonary hypertension specialist
- Continued use of anticoagulant medications as prescribed
- Participation in cardiac or pulmonary rehabilitation programs
- Monitoring for symptoms of recurrent pulmonary hypertension
- Healthy lifestyle habits (including not smoking and regular exercise as tolerated)
Frequently Asked Questions (FAQs) About Pulmonary Thromboendarterectomy
What is the difference between a pulmonary thromboendarterectomy and a pulmonary embolectomy?
Pulmonary thromboendarterectomy (PTE) removes chronic, organized clots and scar tissue from the pulmonary arteries and is intended for chronic disease (CTEPH). Pulmonary embolectomy is usually performed emergently, removing fresh clots from the pulmonary arteries in cases of acute pulmonary embolism. PTE addresses long-standing, complex disease, requiring specialized surgical skills.
How long does the surgery take?
PTE is a lengthy operation, typically taking 6–10 hours to complete due to the complexity of the procedure, the use of circulatory arrest, and the need to clear both right and left pulmonary arteries thoroughly.
What is the typical success rate?
Success rates in experienced centers are high, with the majority of patients experiencing significant improvement in symptoms. The mortality rate is typically less than 5% in specialist centers.
Are there alternatives to PTE?
Alternatives include lifelong blood-thinning medications, balloon pulmonary angioplasty for inoperable disease, and lung transplantation in select severe cases, but none are as definitively curative as PTE for suitable patients.
How soon can I return to normal activities?
Most patients begin resuming regular activities in 2–3 months, although full recovery and optimal improvement in exercise capacity may take up to 6 months post-surgery.
Does CTEPH always require surgery?
No. Some cases can be managed with medications alone or treated with less invasive procedures if surgery is not possible. However, PTE remains the gold standard and only curative option for eligible patients with operable disease.
Resources and Support
- Pulmonary Hypertension Association: Patient resources and support groups
- Centers specializing in CTEPH and PTE: Seek care at institutions with documented expertise in these complex procedures
- Rehabilitation and Counseling: Support to aid in physical and emotional recovery after open-heart surgery
If you or a loved one have been diagnosed with CTEPH, request a referral to a center experienced in PTE evaluation and treatment. Early diagnosis and timely intervention can dramatically improve quality of life and outlook.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5344471/
- https://www.templehealth.org/services/treatments/pulmonary-thromboendarterectomy
- https://www.yalemedicine.org/clinical-keywords/pulmonary-thromboendarterectomy
- https://www.ottawaheart.ca/test-procedure/pulmonary-thromboendarterectomy
- https://my.clevelandclinic.org/health/treatments/21024-pulmonary-thromboendarterectomy-surgery
- https://phassociation.org/about-cteph/pte-surgery/
- https://mmcts.org/tutorial/713
- https://www.svhlunghealth.com.au/procedures/procedures-treatments/pulmonary-endarterectomy
Read full bio of medha deb












