Pulmonary Thromboendarterectomy: Treating Chronic Clots in the Lungs
Learn about pulmonary thromboendarterectomy, a life-saving surgery for chronic clot-related lung disease, including preparation, procedure, risks, and outcomes.
Pulmonary Thromboendarterectomy: Surgical Relief for Chronic Lung Blood Clots
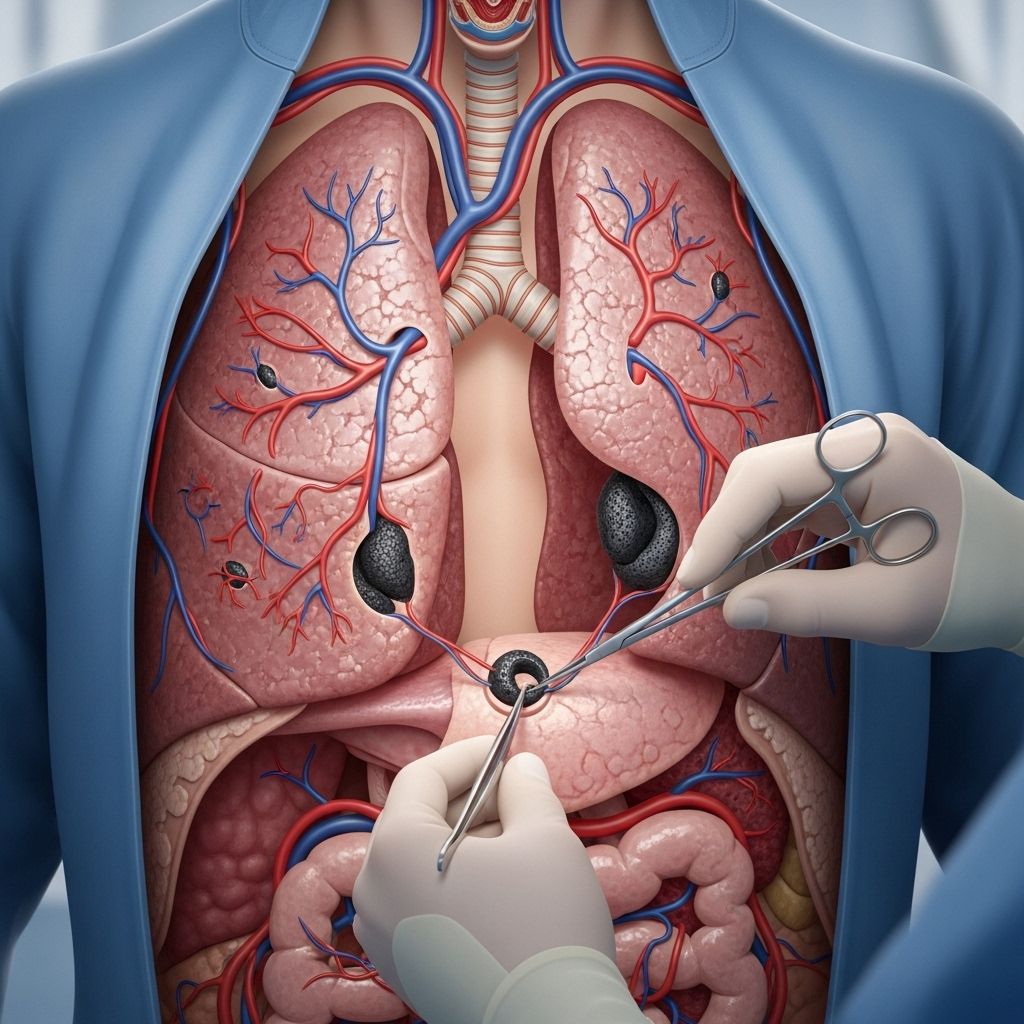
Pulmonary thromboendarterectomy (PTE)—sometimes called pulmonary endarterectomy—is a major heart and lung operation designed to remove organized blood clots and scar tissue from the pulmonary arteries. The procedure offers relief and restoration of healthy blood flow for patients suffering from chronic thromboembolic pulmonary hypertension (CTEPH), a rare but serious cause of high blood pressure in the lungs due to unresolved blood clots.
What Is Pulmonary Thromboendarterectomy?
Pulmonary thromboendarterectomy is a surgical intervention aimed at extracting chronic blood clots and the resulting fibrous tissue that obstructs the pulmonary arteries—the main blood vessels delivering blood from the heart to the lungs. Over time, these blockages can lead to severe pulmonary hypertension, right heart strain, and respiratory distress. PTE is regarded as the most definitive and potentially curative treatment for eligible patients with CTEPH.
- Purpose: Remove chronic clots from arteries in the lungs to restore blood flow and reduce high pressure.
- Target patients: Individuals with CTEPH or similar persistent clot-related lung vessel blockage.
- Main benefit: Can often completely resolve symptoms and improve survival rates.
Who Needs Pulmonary Thromboendarterectomy?
PTE is recommended for patients with chronic thromboembolic pulmonary hypertension, a condition where blood clots in the lungs fail to dissolve, causing scar tissue that narrows and blocks vessels. Not everyone with CTEPH will be a candidate, as the location and accessibility of the clots, overall health, and presence of other medical devices (such as pacemakers) can affect suitability.
- Common candidates: Adults with persistent blood clots in the lungs causing pulmonary hypertension.
- Clot features: Clots must be organized and accessible for surgical removal.
- Assessment factors: Health status, comorbidities, prior treatments, location of clots, and surgical risks.
Understanding CTEPH: The Disease Behind the Procedure
CTEPH is a rare, life-threatening form of pulmonary hypertension. Its hallmark is elevated lung blood pressure caused by chronic, unresolved blood clots—sometimes from earlier episodes of pulmonary embolism. Over time, these clots become fibrotic, impeding blood flow and causing strain on the right side of the heart. Symptoms range from shortness of breath, fatigue, chest pain, and swelling, often worsening with exertion.
| Feature | CTEPH Impact |
|---|---|
| Primary Cause | Chronic blood clots & scar tissue in pulmonary arteries |
| Major Symptom | Progressive shortness of breath |
| Risk | Right heart failure, respiratory failure, death |
| Definitive Treatment | Pulmonary thromboendarterectomy |
Preparing for Pulmonary Thromboendarterectomy
Preparation for PTE is extensive. Patients will undergo comprehensive cardiovascular and respiratory evaluation, imaging (such as pulmonary angiography and CT scans) to map the clots’ location, and blood tests to assess overall fitness.
- Preoperative visits: Evaluation by cardiologists, pulmonologists, and surgeons.
- Imaging: Angiograms, CT scans, and cardiac ultrasounds help plan the operation.
- Medication adjustments: Blood thinners and other relevant drugs may be modified.
- Fasting: Overnight fasting before surgery is generally required.
The Pulmonary Thromboendarterectomy Procedure: Step-by-Step
PTE is performed under general anesthesia and involves several key stages. The surgery may take several hours, and patients will be connected to a heart-lung machine (cardiopulmonary bypass) to keep blood flowing while the heart is temporarily stopped. Cooling of the blood and body is used for organ protection during periods of circulatory arrest, giving surgeons time to access and clear the clots.
- Incision: A vertical cut is made along the center of the chest, and the breastbone (sternum) is divided to access the heart and lung arteries.
- Heart-Lung Machine: Blood is rerouted through a machine that oxygenates and pumps blood, allowing the heart and lungs to be temporarily stopped.
- Cooling: Patient’s body cooled to around 20°C (68°F) to protect vital organs while blood flow is interrupted.
- Arterial Access: The surgeon opens the pulmonary artery to visualize the blocked areas.
- Clot Removal: Clots and accompanying scar tissue are carefully dissected out from the arteries with special microsurgical tools. This requires precise identification of the correct dissection plane—between the inner vessel layers.
- Restoration: The arteries are repaired, circulation is restored, and body temperature is returned to normal.
- Closure: The chest is closed, and the heart-lung machine is gradually withdrawn as heart and lung function resumes.
Surgical Techniques: Key Principles
- Bilaterality: Surgery is performed on both left and right pulmonary arteries through a median sternotomy.
- Visualization: Superb visualization is critical, achieved using cardiopulmonary bypass and short circulatory arrest periods.
- Dissection Plane: Correctly identifying the space between vessel layers ensures complete clot and tissue removal.
- Complete Endarterectomy: Surgeons meticulously extract all affected tissue until the vessel is clear, following each subsegmental branch.
PTE is a technically complex surgery requiring a highly experienced multidisciplinary team. The goal is a complete removal of all obstructive material. An incomplete procedure may not relieve all symptoms.
Risks and Possible Complications
As with any major open-heart surgery, pulmonary thromboendarterectomy carries significant risks. Serious complications are relatively uncommon in high-volume, experienced surgical centers.
- Bleeding: Risk of major bleeding during or after surgery.
- Infection: Potential for chest, lung, or wound infection.
- Stroke or Other Organ Injury: Rare risk due to temporary stoppage of blood flow.
- Heart rhythm problems: Temporary arrhythmias can occur.
- Residual hypertension: Not all patients experience complete normalization of lung blood pressure, particularly if some arteries are inaccessible.
Special considerations include people with comorbid heart or lung diseases, or those with mechanical devices such as pacemakers or vascular shunts. In some cases, the anatomy or the location of clots may prevent full surgical access.
Benefits of Pulmonary Thromboendarterectomy
PTE is widely considered the gold-standard, potentially curative therapy for eligible patients with CTEPH. When successful, patients often experience dramatic improvements in lung function, heart health, exercise capacity, and overall quality of life.
- Most patients see a marked reduction in pulmonary artery pressure.
- Right heart strain is relieved; symptoms of heart failure often resolve.
- Many can discontinue oxygen therapy and resume normal activities.
- Longevity and survival rates improve notably compared to untreated CTEPH.
Recovery After PTE Surgery
Postoperative recovery takes place in an intensive care unit (ICU) for close monitoring. The hospital stay typically lasts one to three weeks, depending on complications and recovery speed.
- Continuous monitoring of heart, lung, and kidney function is required.
- Early mobility and physical therapy are vital to prevent further clots and restore strength.
- Respiratory therapy helps clear airways and improves lung function.
- Medications may be needed to manage blood pressure and prevent new clots.
Most patients need several months of gradual recovery before full return to daily activities. Regular follow-up visits with cardiology and pulmonology specialists are essential to monitor lung and heart health.
Alternatives to Pulmonary Thromboendarterectomy
Some patients are not eligible for PTE due to technical or health reasons. Alternatives include:
- Medical therapy: Pulmonary hypertension-specific drugs, anticoagulants, and supportive care.
- Balloon pulmonary angioplasty: A catheter-based procedure for select inoperable cases.
- Lung transplantation: Considered only in end-stage disease when other options fail.
Frequently Asked Questions (FAQs)
What makes someone a good candidate for PTE?
Candidates typically have organized, accessible clots causing significant pulmonary hypertension and are healthy enough for major surgery. Evaluation by an experienced team is required.
Is PTE curative?
For many patients with CTEPH, PTE offers a cure, with marked improvement or complete resolution of symptoms and normalization of pulmonary pressure. Long-term monitoring remains important.
How long does the surgery take?
The procedure is lengthy, often taking several hours, due to the complexity and need for precise removal of clots.
What are the long-term outcomes?
Most patients experience sustained improvements in symptoms, exercise tolerance, and life expectancy. Some may remain on blood thinners or pulmonary hypertension medication, depending on surgical results.
Can blood clots return?
New blood clots can form if underlying risk factors persist. Lifelong follow-up and preventive blood thinners are often recommended.
What should I expect during recovery?
Recovery includes ICU care, gradual mobilization, respiratory support, and regular medical follow-up. Return to normal life generally takes several months.
Tips for Living with CTEPH and Preparing for PTE Surgery
- Stay informed: Discuss all treatment options with your care team, including risks and alternatives.
- Healthy habits: Quit smoking, eat a heart-healthy diet, and exercise as advised.
- Follow medication plans: Adhere to prescribed blood thinners and other relevant medications.
- Arrange support: Organize help for your recovery period—physical and emotional support is important.
- Keep follow-up visits: Attend all post-surgical checkups to ensure optimal recovery.
Summary
Pulmonary thromboendarterectomy is a lifesaving procedure for people suffering from chronic clot-related pulmonary hypertension. With careful preparation, skilled surgery, and diligent recovery, the operation offers hope for restored lung and heart function. Team-based care from experienced cardiac and pulmonary specialists is key to optimal outcomes.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5344471/
- https://www.medicalnewstoday.com/articles/pulmonary-thromboendarterectomy
- https://www.templehealth.org/services/treatments/pulmonary-thromboendarterectomy
- https://www.yalemedicine.org/clinical-keywords/pulmonary-thromboendarterectomy
- https://phassociation.org/about-cteph/pte-surgery/
- https://my.clevelandclinic.org/health/treatments/21024-pulmonary-thromboendarterectomy-surgery
- https://mmcts.org/tutorial/713
- https://www.svhlunghealth.com.au/procedures/procedures-treatments/pulmonary-endarterectomy
Read full bio of medha deb












