Treatment Approaches for Pulmonary Embolism: A Comprehensive Guide
Explore medications, procedures, and lifestyle strategies for treating pulmonary embolism effectively and preventing recurrence.
Pulmonary Embolism Treatment: An In-Depth Overview
Pulmonary embolism (PE) is a critical and potentially life-threatening condition in which a blood clot blocks one or more arteries in the lungs. Timely and effective treatment is vital to increase survival rates and minimize long-term complications. This guide details all current treatment strategies, alternatives for high-risk cases, ongoing care, and answers to frequently asked questions.
What is Pulmonary Embolism?
Pulmonary embolism occurs when a blood clot, often originating in the deep veins of the legs (a condition called deep vein thrombosis or DVT), travels to the lungs and obstructs blood flow. PE can range in severity from minor symptoms to sudden death, making rapid diagnosis and intervention crucial.
Objectives of Pulmonary Embolism Treatment
- Prevent the blood clot from increasing in size
- Stop new clots from forming
- Restore blood flow to affected parts of the lung
- Reduce risk of recurrence
- Minimize or prevent long-term complications, such as pulmonary hypertension
Medications for Pulmonary Embolism
Medications play a primary role in both immediate and long-term management of PE. The choice of medication depends on the clot’s size, the patient’s risk for bleeding, existing medical conditions, and urgency of intervention.
1. Anticoagulants (Blood Thinners)
Anticoagulants are the first-line therapy for most cases. They work by inhibiting further clotting and allowing the body to gradually dissolve existing clots.
- Heparin: Typically administered intravenously or subcutaneously, acts quickly and is often used in hospital settings.
- Low Molecular Weight Heparin (LMWH): Such as enoxaparin, can be injected under the skin and may be used outside of a hospital.
- Warfarin (Coumadin): An oral anticoagulant, often started together with heparin until effective blood thinning is established. Requires regular blood testing (INR) and monitoring for interactions.
- Direct Oral Anticoagulants (DOACs): Include drugs like rivaroxaban, apixaban, edoxaban, and dabigatran. These have predictable effects, fewer interactions, and do not usually require routine blood test monitoring. Some DOACs can be started directly without needing heparin first.
Important note: All anticoagulants carry a risk of bleeding, including potentially serious internal bleeding.
2. Thrombolytics (Clot-Dissolving Drugs)
Thrombolytic agents, sometimes called “clot busters”, dissolve existing clots much faster than anticoagulants, but carry a higher risk of dangerous bleeding. Their use is typically limited to life-threatening, massive PEs or cases with severe instability.
- Examples: Alteplase, streptokinase, tenecteplase
- Method of delivery: Usually administered intravenously in a hospital under intensive monitoring.
- Risks: Include major bleeding and are generally reserved for high-risk PE where benefits outweigh risks.
3. Other Medications
Supportive medications might include pain relievers (for chest discomfort), supplemental oxygen (if blood oxygen is low), or medications to support blood pressure in severe cases. These do not treat the clot directly but may enhance recovery and comfort.
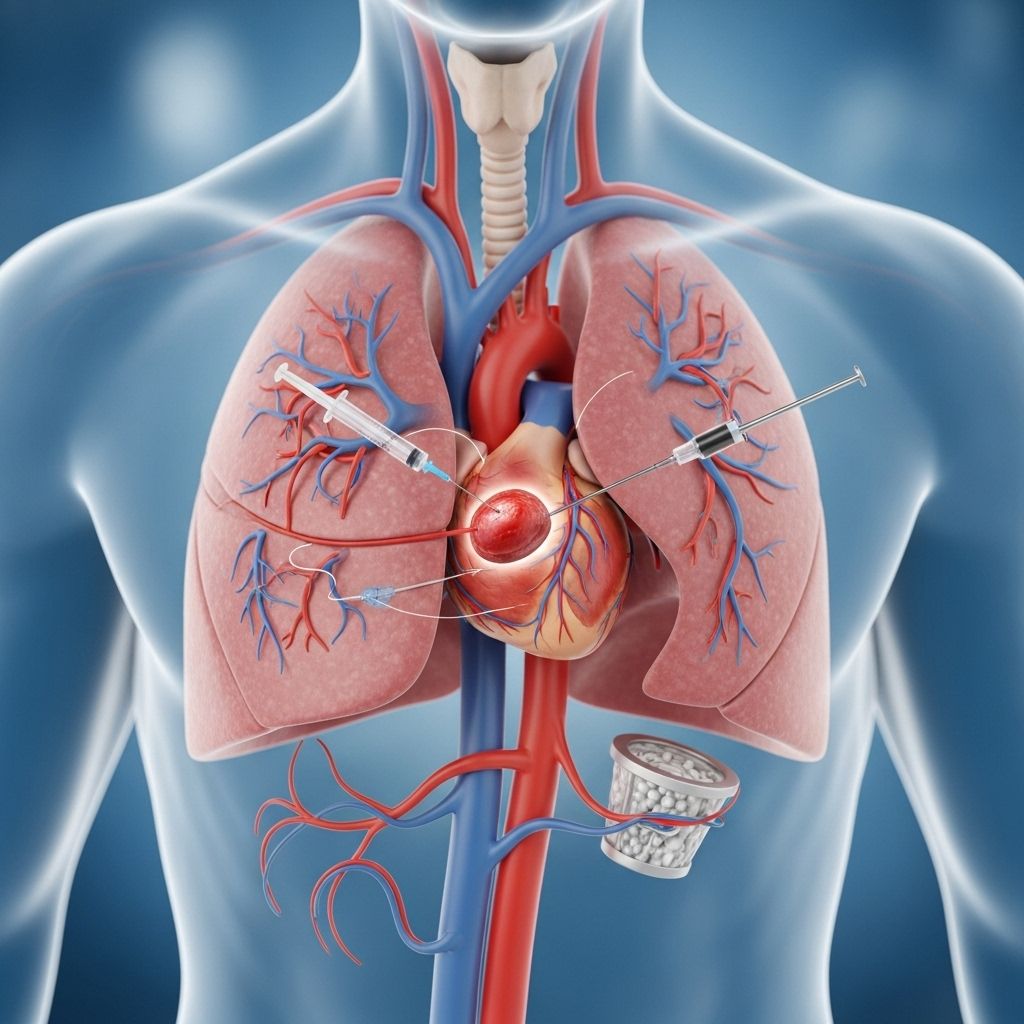
Surgical and Minimally Invasive Procedures
When medications are unsuitable or insufficient—such as when someone cannot have anticoagulants due to bleeding risk, or in cases of massive/life-threatening PEs—specialized procedures may be considered.
1. Catheter-Directed Thrombolysis
This minimally invasive technique involves threading a thin, flexible tube (catheter) into the lung arteries (usually through a vein in the groin, neck, or behind the knee) and delivering thrombolytic agent directly into the clot. This can result in higher concentrations of clot-dissolving medication at the blockage, using lower overall drug doses and potentially reducing the risk of bleeding complications compared to systemic thrombolysis.
2. Catheter-Based Thrombus Removal (Mechanical Thrombectomy)
In this approach, devices attached to a catheter are used to physically break apart or suction out the clot. This is often performed under X-ray guidance in a specially equipped lab (catheterization suite).
- Beneficial for patients with large, obstructive clots or those who cannot take thrombolytic medications.
- Helps restore blood flow quickly and may rapidly improve symptoms and heart/lung function.
3. Surgical Embolectomy
This traditional surgical option is reserved for the most severe, unstable, or medicine-resistant PE cases. Surgeons open the chest to locate and remove the clot directly from the pulmonary arteries. This is rarely required and is performed only in specialized centers with critical care and cardiac surgery resources.
4. Vein (Inferior Vena Cava) Filter Placement
An inferior vena cava (IVC) filter is a small, cage-like device placed via a catheter into the body’s main vein (vena cava) below the heart. It acts as a barrier, catching large clots before they can reach the lungs. These filters are mainly used for patients who:
- Cannot take anticoagulant medications due to bleeding risks.
- Continue to develop clots despite blood thinners.
IVC filters may be temporary or permanent, depending on the risk profile and changes in patient condition over time. They do not dissolve or treat existing clots, only prevent further embolization.
5. Balloon Pulmonary Angioplasty (BPA)
BPA is a specialized catheter-based treatment increasingly used for chronic, organized clots obstructing smaller pulmonary arteries, especially in patients who are not candidates for surgery. During BPA, a deflated balloon is guided to the affected arteries and gently inflated to break up and move the clot, restoring blood flow. This advanced procedure is offered at select, highly specialized centers.
Ongoing Care and Long-Term Management
After stabilization and initial treatment, preventing recurrence and monitoring for complications is critical.
- Continued anticoagulation: Many patients require blood thinners for several months, sometimes indefinitely, based on risk factors and recurrence likelihood.
- Monitoring: Regular medical follow-up, blood tests (if on warfarin), and periodic reassessment to monitor side effects and treatment efficacy.
- Lifestyle modifications: Addressing underlying contributors like immobility, obesity, cancer, or hormone use reduces future clot risks.
- Compression stockings: May be recommended to lower the risk of DVT, especially in those with limited mobility.
For patients with persistent symptoms or signs of chronic thromboembolic pulmonary hypertension (CTEPH), further specialized evaluation and treatment, such as BPA or surgical pulmonary endarterectomy, may be required.
Risks and Complications of Treatment
While treatment for PE is often lifesaving, there are notable risks and potential complications depending on the strategy used.
- Bleeding: All anticoagulants increase bleeding risks, ranging from minor bruising to dangerous internal bleeding.
- Drug interactions: Especially with warfarin, which requires careful monitoring to maintain effective levels.
- Complications from procedures: Such as infection, injury to blood vessels, or allergic reactions.
- IVC filter issues: Rare complications include filter migration, breakage, or causing new blood clots within the filter device itself.
Prevention of Pulmonary Embolism
Preventing PE, especially for those at high risk, is a key component of ongoing care. Strategies include:
- Ensuring early movement after surgery or during long hospital stays
- Use of compression stockings when advised
- Treating underlying risk factors such as cancer, heart failure, or immobility
- Regular follow-up to assess ongoing risk of recurrence
Frequently Asked Questions (FAQs)
What is the most common initial treatment for pulmonary embolism?
The primary initial treatment for most people with PE is anticoagulant medication, intended to prevent the clot from growing and to lower the risk of new clots forming. The choice between heparin, LMWH, or DOACs depends on several clinical factors.
Can all pulmonary embolisms be treated without surgery?
Most PEs are managed effectively with medications. Surgery or catheter-based procedures are typically reserved for cases when medications fail, when bleeding risk is too high, or when the patient is unstable or at immediate risk.
Are there long-term effects after a pulmonary embolism?
While many recover fully, some may develop chronic problems like CTEPH (chronic thromboembolic pulmonary hypertension) or suffer from persistent shortness of breath or leg swelling after a large PE. Careful follow-up and monitoring are essential.
How long do I have to take blood thinners after a PE?
The duration of anticoagulation depends on the size and cause of the PE, as well as the risk of recurrence. It can range from 3 months to lifelong, based on individual risk assessments.
What are the warning signs that I might be having another PE?
Seek immediate care if you notice new or worsening shortness of breath, chest pain, rapid heart rate, coughing up blood, or unexplained fainting, as these could be signs of a recurrent clot.
Key Takeaways
- Pulmonary embolism is a serious medical emergency, requiring fast diagnosis and appropriate care.
- Most cases respond well to anticoagulant medications, but advanced or minimally invasive procedures and surgery may be necessary in severe or resistant cases.
- Long-term management and prevention strategies are crucial to reduce the risk of recurrence.
- Regular medical follow-up and adherence to prescribed treatments optimize recovery and outcomes.
References
- https://www.mayoclinic.org/diseases-conditions/pulmonary-embolism/diagnosis-treatment/drc-20354653
- https://www.uofmhealth.org/conditions-treatments/pulmonary-embolism-and-cteph/1000
- https://www.ncbi.nlm.nih.gov/books/NBK560551/
- https://eurointervention.pcronline.com/article/percutaneous-interventions-for-pulmonary-embolism
- https://my.clevelandclinic.org/health/diseases/17400-pulmonary-embolism
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/pulmonary-embolism/treating-and-managing
- https://www.uscjournal.com/articles/advanced-management-options-massive-and-submassive-pulmonary-embolism?language_content_entity=en
Read full bio of medha deb












