Pseudomembranous Conjunctivitis: Causes, Symptoms, and Effective Treatment
Explore the causes, symptoms, diagnosis, and treatment of pseudomembranous conjunctivitis, a membrane-forming inflammatory eye condition.
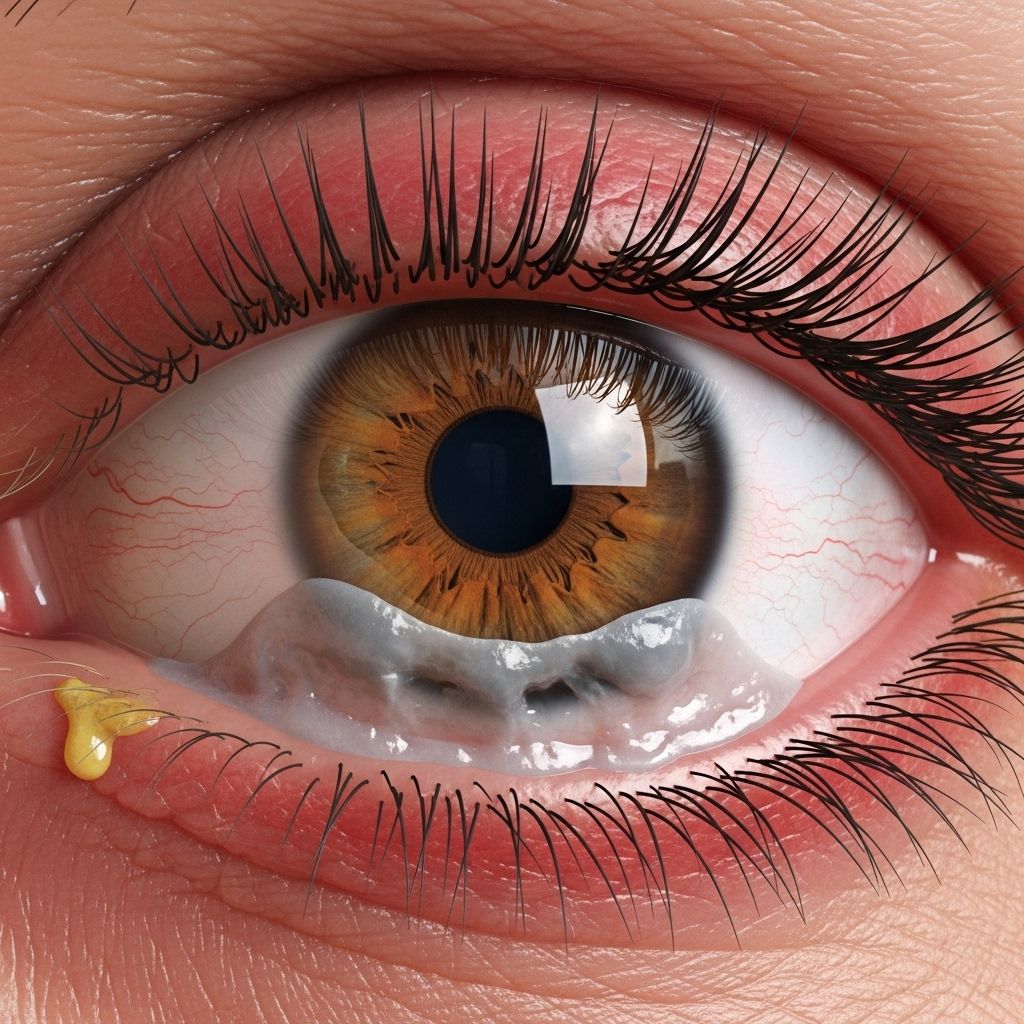
Pseudomembranous conjunctivitis is a specialized form of conjunctivitis characterized by the development of a thin, whitish-yellow membrane on the conjunctiva, the clear tissue covering the white part of the eye and lining the inside of the eyelids. This condition can arise from various infectious and noninfectious triggers, resulting in symptoms like eye discomfort, redness, noticeable discharge, and sometimes disturbances in vision. Understanding this condition is crucial for effective management and the prevention of complications.
What Is Pseudomembranous Conjunctivitis?
Pseudomembranous conjunctivitis is an inflammatory eye disorder in which a thin film—composed chiefly of fibrin and inflammatory cells—forms over the conjunctiva. This membrane is called a pseudomembrane: it can generally be peeled away from the underlying tissue without causing significant bleeding, unlike a true membrane, which is more firmly attached and bleeds when removed.
This relatively uncommon eye condition may affect one or both eyes and can present significant discomfort. Prompt diagnosis and management are important to prevent complications affecting vision and eye health.
Pseudomembranous Conjunctivitis Symptoms
Pseudomembranous conjunctivitis presents a spectrum of symptoms, some shared with other conjunctival disorders and some more distinct:
- Blurred vision
- Eye discomfort or irritation
- Mucopurulent discharge (a sticky, pus-containing eye discharge)
- Redness (conjunctival injection)
- Sensitivity to light (photophobia)
- Swelling of the conjunctiva
- Excessive tearing
The pseudomembrane itself may not always be visible, but when apparent, appears as a whitish or yellowish film on the conjunctival lining beneath the eyelid. The membrane can often be seen as a translucent sheet or film covering parts of the eye, especially in the inner eyelid area.
Severity and frequency of symptoms can vary by underlying cause and host factors, such as immune response and age.
What Does Pseudomembranous Conjunctivitis Look Like?
A close observation—often by an ophthalmologist—may reveal the hallmark thin, whitish-yellow film (pseudomembrane) over the conjunctiva. Medical professionals may use a slit-lamp microscope for better visualization. The membrane can often be gently peeled off, typically leaving little to no bleeding, which helps distinguish it from a true membrane (where bleeding is common upon removal).
Primary Causes of Pseudomembranous Conjunctivitis
Multiple etiologies may give rise to pseudomembranous conjunctivitis. Below are the most frequent causes:
- Bacterial Infections:
- Bacteria such as Corynebacterium diphtheriae, Neisseria gonorrhoeae, Streptococcus pyogenes, and Staphylococcus aureus are strongly linked to pseudomembrane formation. These bacteria incite an inflammatory response in the conjunctiva, leading to fibrin-rich exudate accumulation and eventual membrane formation.
- Viral Causes:
- Epidemic keratoconjunctivitis (EKC): This highly contagious infection is caused by the human adenovirus. In severe cases, adenoviral infection (typically EKC caused by serovars 8, 19, 37) can lead to the formation of pseudomembranes. EKC often presents with watery discharge, irritation, and photophobia.
If you're curious about how pseudomembranous conjunctivitis can be confused with other common eye conditions, check out our insightful article on what is commonly misdiagnosed as pink eye. This knowledge can help you recognize the signs and seek appropriate treatment more quickly. - Ligneous Conjunctivitis:
- This rare, noninfectious form is associated with abnormal wound healing and excess fibrin buildup after trauma or surgery, resulting in persistent, recurrent pseudomembranes. Ligneous conjunctivitis may be genetically linked to plasminogen deficiency, which impairs normal dissolution of fibrin.
- Ocular Graft-Versus-Host Disease (GVHD):
- This condition can arise after allogeneic stem cell transplantation. The immune system attacks the transplanted cells, causing various ocular manifestations, including pseudomembranous conjunctivitis.
- Stevens-Johnson Syndrome (SJS):
- SJS is a rare but critical skin and mucous membrane disorder, often triggered by medications or infections. It is characterized by skin and mucosal blistering, including the conjunctiva, and can rapidly lead to pseudomembranous or membranous conjunctivitis. SJS is an ophthalmic emergency requiring urgent treatment.
- Foreign Body and Toxic or Allergic Reactions:
- Occasionally, physical foreign bodies (such as plant matter or cotton from swabs) or chemical irritants can provoke localized conjunctival inflammation and secondary pseudomembrane formation. Some antibiotics and preservatives in eye drops, like gentamicin, may also be irritant causes in rare cases.
Table: Causes of Pseudomembranous Conjunctivitis
| Category | Examples | Notes |
|---|---|---|
| Bacterial | Corynebacterium diphtheriae, Neisseria gonorrhoeae, Streptococcus pyogenes, Staphylococcus aureus | Severe or untreated infections increase risk |
| Viral | Human adenovirus (EKC serovars 8, 19, 37) | Highly contagious; often associated with outbreaks |
| Noninfectious (Immune-mediated) | Ligneous conjunctivitis (plasminogen deficiency), Ocular GVHD, Stevens-Johnson Syndrome (SJS) | Often related to systemic illness or genetic conditions |
| Toxic/Allergic/Irritant | Gentamicin toxicity, chemical exposures, allergens, foreign bodies (cotton, vegetative matter) | Usually resolve on removal of offending agent |
How Is Pseudomembranous Conjunctivitis Diagnosed?
Diagnosis is primarily clinical, based on a detailed eye exam. Key elements include:
- History Taking: Investigating the onset, duration, and progression of symptoms plus any prior eye trauma, recent infections, medication use, allergies, or systemic illnesses.
- Physical Exam: Using slit-lamp biomicroscopy to assess the conjunctiva, detect membrane, and look for secondary signs like discharge, redness, or corneal involvement. Attempting gentle membrane peeling may help distinguish pseudomembranes from true membranes (little to no bleeding if pseudomembrane).
- Laboratory Tests: In unclear or severe cases, cultures or PCR testing of conjunctival swabs may identify infectious causes (bacteria, virus). In ligneous conjunctivitis, laboratory evaluation for plasminogen deficiency may be indicated. If systemic illness is suspected, additional blood or urine tests may be ordered.
Treatment for Pseudomembranous Conjunctivitis
Treatment strategies are dictated by the underlying cause and severity. Common approaches include:
- Removal of the Pseudomembrane: Peeling or gently removing the membrane under sterile conditions often relieves symptoms and may help speed recovery.
- Antibiotic Eye Drops or Ointments: Bacterial cases require targeted antibiotics, especially for severe or high-risk pathogens (diphtheria, gonorrhea, group A strep).
- Antiviral Therapy: There is no specific antiviral treatment for adenoviral conjunctivitis, but supportive care is essential. Severe or sight-threatening viral infections may rarely need special interventions.
- Corticosteroids: Topical steroid eye drops may be prescribed for significant inflammation or when membrane formation is persistent, especially in immune-mediated or ligneous causes. Use is closely monitored due to potential side effects (e.g., increased eye pressure, risk of infection).
- Supportive Care: Application of cool compresses, artificial tears, and pain relief medications helps alleviate discomfort. In allergic, irritant, or drug-induced cases, removing the offending agent is crucial.
- Treatment of Underlying Systemic Conditions: In cases associated with SJS, GVHD, or systemic infections, prompt coordination with medical and subspecialist teams is required for best outcomes.
Complications to Watch For
- Persistent pseudomembrane recurrence
- Corneal involvement (keratitis, ulceration)
- Scarring or symblepharon (adhesion of the eyelid to the eyeball)
- Secondary bacterial infection
- Potential for decreased vision if inflammation or scarring involves the visual axis
Prevention and Prognosis
Prevention hinges on robust infection control and timely treatment of infectious conjunctivitis:
- Practice frequent, thorough hand-washing
- Avoid touching or rubbing the eyes with unwashed hands
- Do not share towels, eye drops, or cosmetics
- Promptly treat bacterial or viral conjunctivitis as recommended by a healthcare provider
- Seek immediate medical attention for eye injuries, chemical splashes, or symptoms following stem cell transplantation or medication exposure
Most cases resolve without permanent effect if the cause is identified and appropriately treated. However, severe or chronic forms—especially those associated with SJS, severe bacterial infections, GVHD, or ligneous conjunctivitis—require close specialist care. Failure to treat can lead to scarring, vision loss, or other complications.
Frequently Asked Questions (FAQs)
Q: Is pseudomembranous conjunctivitis contagious?
A: Contagiousness depends on the underlying cause. If caused by bacteria (such as Neisseria gonorrhoeae or group A strep) or viruses (such as adenovirus in EKC), it can be very contagious. Noninfectious or immune-mediated forms are not spread person-to-person.
Q: How can I tell pseudomembranous conjunctivitis apart from other conjunctivitis types?
A: The presence of a visible, peelable membrane on the conjunctiva strongly suggests pseudomembranous conjunctivitis. However, a medical exam is always necessary to confirm the diagnosis and find the underlying cause.
Q: Can pseudomembranous conjunctivitis affect vision permanently?
A: Permanent vision impact is rare with timely and appropriate treatment. However, inadequate or delayed care, especially in cases with severe inflammation or scarring, can result in long-term visual impairment.
Q: What should I do if I suspect I have this condition?
A: Seek prompt eye evaluation from an ophthalmologist or healthcare provider. Early intervention minimizes complications and ensures optimal recovery.
Q: Are there any home remedies for pseudomembranous conjunctivitis?
A: Home care (such as artificial tears, cold compresses, and proper hygiene) may provide symptom relief but does not address serious causes. Professional evaluation and treatment are imperative for suspected pseudomembranous conjunctivitis.
Q: When should I seek urgent medical care?
A: See a healthcare provider immediately if you experience intense pain, severe vision loss, new blistering or rash, or have a history suggesting immune compromise (e.g., recent transplant, systemic illness).
Summary
Pseudomembranous conjunctivitis is an uncommon but clinically important eye condition marked by the formation of a thin, removable conjunctival membrane. Causes range from severe bacterial and viral infections to immune-mediated processes and toxic exposures. With prompt diagnosis and appropriate care, prognosis is generally favorable, though vigilant follow-up is needed for severe or recurrent cases. If you have symptoms of conjunctivitis with persistent discomfort or visible eye film, consult an eye care provider promptly.
References
- https://www.healthline.com/health/eye-health/pseudomembranous-conjunctivitis
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7299555/
- https://www.merckmanuals.com/professional/eye-disorders/conjunctival-and-scleral-disorders/viral-conjunctivitis
- https://www.ncbi.nlm.nih.gov/books/NBK541034/
- https://www.reviewofoptometry.com/article/ro-0317-a-sticky-situation
- https://www.mayoclinic.org/diseases-conditions/pink-eye/symptoms-causes/syc-20376355
- https://www.consultant360.com/articles/conjunctivitis-pseudomembrane
- https://my.clevelandclinic.org/health/diseases/pink-eye-conjunctivitis
Read full bio of Sneha Tete












