Pseudoaneurysm After Cardiac Catheterization: Causes, Risks and Treatment
Understand what causes pseudoaneurysms, how they're linked to cardiac catheterization, signs, risks, and the latest medical treatments.
Pseudoaneurysm: Causes, Risks, and Treatments After Cardiac Catheterization
A pseudoaneurysm (sometimes called a false aneurysm) is a vascular complication that can occur after certain procedures, especially cardiac catheterization. Understanding pseudoaneurysms is important for anyone undergoing interventional procedures, as early detection and management are critical for preventing serious outcomes.
What is a Pseudoaneurysm?
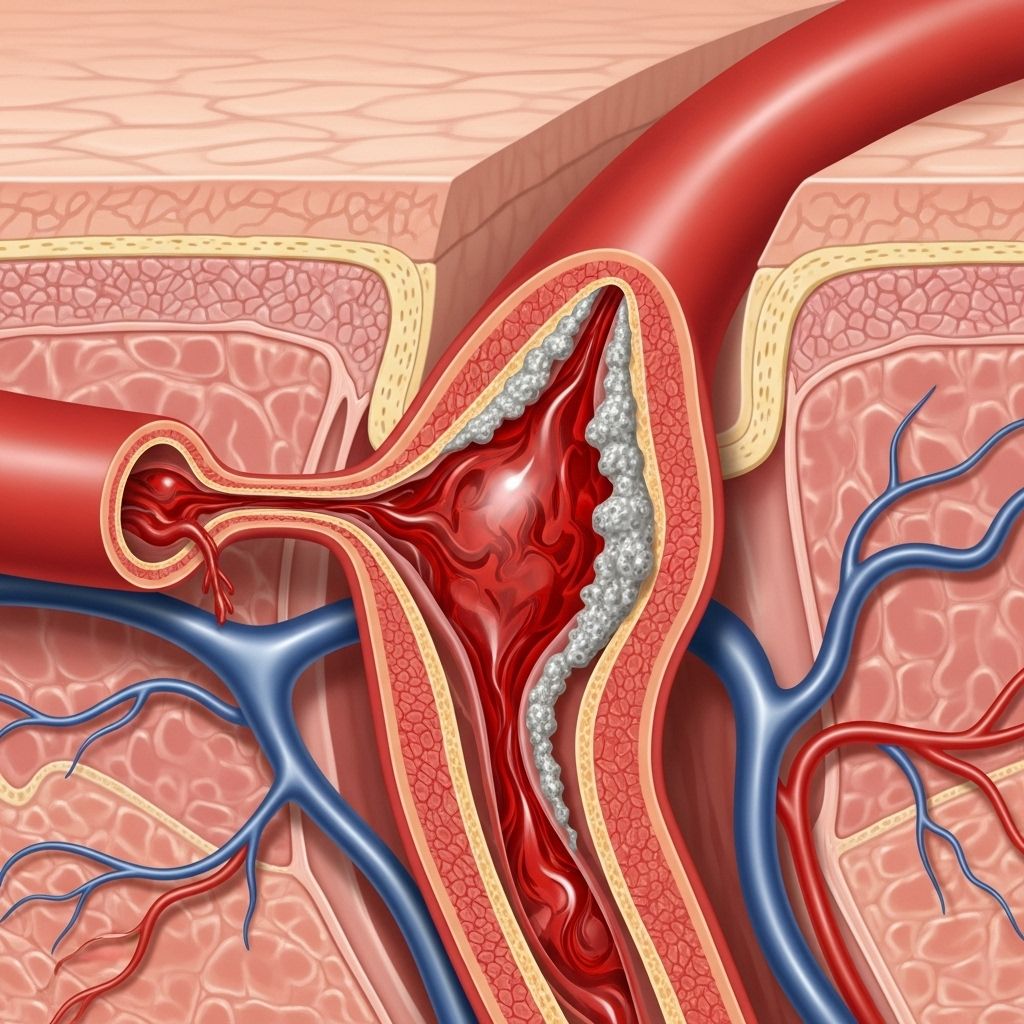
A pseudoaneurysm develops when a blood vessel wall is injured, allowing blood to leak out and collect in the surrounding tissue. Unlike a true aneurysm, where the vessel wall itself bulges, a pseudoaneurysm results from a breach in the vessel wall — the bleeding is contained by tissues outside the vessel and not by the vessel wall itself.
This collection of blood is usually surrounded by a fibrous capsule and can form a pulsatile mass near the site of vessel injury.
How Does a Pseudoaneurysm Differ from a True Aneurysm?
| Aspect | Pseudoaneurysm (False Aneurysm) | True Aneurysm |
|---|---|---|
| Wall Structure | Blood escapes through a vessel wall defect, contained by surrounding tissues only. | Wall remains intact but weakens and bulges outward. |
| Containment | Via fibrous tissue or hematoma, not vessel wall. | By all three layers of the artery wall. |
| Typical Cause | Vessel wall injury (e.g., procedures, trauma). | Degeneration or chronic disease causing wall weakness. |
What Causes a Pseudoaneurysm?
Pseudoaneurysms can develop in any artery or vessel following an injury that disrupts the vessel wall. The most common scenarios include:
- Cardiac catheterization: When a catheter is inserted (typically into the femoral artery in the groin), blood can sometimes leak from the vessel wall at the puncture site if it does not close properly, leading to a pseudoaneurysm.
- Surgical procedures: Blood vessel injury during vascular or other surgeries may cause a pseudoaneurysm.
- Infection: Infection at an arterial site may damage the vessel wall, resulting in a pseudoaneurysm.
- Trauma: Direct blows or penetrating injuries to arteries can disrupt the vessel wall.
- Rupture of an existing aneurysm: If an existing aneurysm ruptures, it may lead to the formation of a pseudoaneurysm.
Any procedure involving arterial access — such as diagnostic angiograms, stent placement, or intervention for vascular disease — carries a risk, though careful technique and monitoring have reduced pseudoaneurysm rates in recent years.
Why is Cardiac Catheterization a Risk?
Cardiac catheterization, a procedure commonly performed to diagnose or treat heart conditions, involves threading a thin tube (catheter) through an artery in the groin (femoral) or wrist. If the arterial puncture does not seal properly, blood may leak out into surrounding tissues. This is especially likely in patients taking blood-thinning medications or those with certain vascular conditions.
Symptoms and Signs of Pseudoaneurysm
The symptoms of a pseudoaneurysm usually develop shortly after the vessel injury, but in some cases, they may not be noticeable for several days or weeks. Symptoms depend on the size, location, and rate of blood leakage. Common signs include:
- A swelling or lump: Typically in the groin area (if related to femoral artery catheterization), which may be tender or pulsatile.
- Pain: Localized pain at the procedure site or radiating to nearby areas.
- Bruising: Hematoma formation around the site of vessel injury.
- Redness or warmth: The overlying skin may appear red or feel warm.
- Pulsating mass: A mass that throbs or pulses in time with the heartbeat.
Occasionally, a pseudoaneurysm may go unnoticed, especially if it is very small and not causing symptoms. For this reason, routine examination and ultrasound imaging are often performed after procedures that have a known risk.
When Should a Pseudoaneurysm Be Treated?
Whether a pseudoaneurysm requires treatment depends on its size, symptoms, and risk factors like the use of blood thinners:
- Small pseudoaneurysms (less than 2 cm): Often monitored with watchful waiting and may resolve on their own. Periodic ultrasound testing is used to monitor the size and check for complications.
- Larger pseudoaneurysms (greater than 2 cm): More likely to require treatment due to higher risks of rupture, ongoing bleeding, or compression of nearby structures.
- People on blood thinners: Anticoagulant therapy increases the risk of bleeding complications, making intervention more likely.
If the pseudoaneurysm is enlarging, acutely symptomatic, or still present after several weeks, active treatment is generally recommended.
Potential Complications of Untreated Pseudoaneurysm
- Rupture: May result in life-threatening internal bleeding.
- Compression of nearby nerves or tissues: Can cause pain, numbness, or swelling.
- Infection: Especially if the overlying skin is compromised.
- Blood clots (thromboembolism): Detached clots may travel and block blood vessels elsewhere.
Prompt recognition and management are key to preventing these complications.
How Are Pseudoaneurysms Diagnosed?
Diagnosis typically relies upon:
- Physical examination: Checking for pulsatile masses, swelling, or pain near recent arterial access sites.
- Duplex ultrasound: The imaging test of choice for detecting and measuring pseudoaneurysms. It visualizes blood flow and vessel structure in real time.
- Angiography: Occasionally used for difficult cases or when a more precise map of blood vessels is needed, especially if interventions are being planned.
- CT or MRI: Advanced imaging may be used for pseudoaneurysms in less accessible locations.
Treatment Options for Pseudoaneurysm
Treatment decisions are based on the pseudoaneurysm’s size, location, associated symptoms, and any underlying medical conditions. Approaches include:
- Observation (Watchful Waiting):
- Recommended for small, stable pseudoaneurysms without symptoms or for patients in whom intervention carries high risk.
- Requires regular monitoring via ultrasound to ensure it is not growing or causing complications.
- Ultrasound-Guided Compression Repair:
- Uses ultrasound to locate the pseudoaneurysm.
- Direct, manual pressure is applied to the area with the ultrasound probe to promote clotting and closure of the defect.
- Can be uncomfortable and may require several attempts.
- Less effective if the patient is on blood thinners, or if the neck of the pseudoaneurysm is short.
- Ultrasound-Guided Injection of Medication (Thrombin):
- Thrombin, a clot-promoting medication, is injected directly into the pseudoaneurysm under ultrasound guidance.
- Leads to rapid clot formation and sealing of the leaking vessel.
- Especially effective for femoral artery pseudoaneurysms.
- Minimally invasive, very high success rate, but carries a small risk of clot traveling to other tissues (embolization).
- Surgical Repair:
- Reserved for cases where other treatments have failed or are not feasible, or if the pseudoaneurysm is complicated by rupture, infection, or rapid enlargement.
- May involve open surgery, vascular repair, or endovascular techniques like coil embolization or stent placement.
- Emergency surgery may be necessary if there is active bleeding or risk of rupture.
What You Should Do If You Suspect a Pseudoaneurysm
If you have recently undergone any type of catheterization or arterial procedure and experience the following symptoms, contact your healthcare provider right away:
- Tenderness or swelling at the catheter site
- Development of a lump or pulsating mass
- Unexplained pain or bruising at the access point
Early medical attention can greatly reduce the risk of serious complications.
Frequently Asked Questions (FAQs)
What is the prognosis after treatment for a pseudoaneurysm?
When diagnosed early and treated appropriately, most patients make a complete recovery. The recurrence rate is low, and minimally invasive treatments have high success rates.
Can a pseudoaneurysm resolve without treatment?
Yes, small pseudoaneurysms, especially those less than 2 cm, often resolve on their own. Regular ultrasound monitoring ensures that the lesion is not growing.
What increases the risk of developing a pseudoaneurysm after catheterization?
- Multiple punctures during the procedure
- Larger sheath (catheter) sizes
- Use of blood-thinning medications
- Underlying vascular disease or fragile vessel walls
- Poor post-procedure compression of the puncture site
How can the risk be minimized?
Using appropriate puncture techniques, applying adequate pressure post-procedure, using imaging to guide interventions, and careful patient selection all help lower the risk. Patients should be observed for swelling or bleeding, especially in the hours to days after catheterization.
What is the usual recovery timeline?
Most minimally invasive treatments allow for rapid recovery (within days to weeks). If surgery is needed, recovery may take longer depending on the extent of the repair and underlying health conditions.
Key Takeaways
- Pseudoaneurysms most commonly occur as rare complications after procedures like cardiac catheterization.
- They result from a blood vessel wall injury allowing blood to leak and pool outside the artery.
- Small pseudoaneurysms may not require treatment, but larger or symptomatic ones do.
- Diagnosis is usually made with ultrasound imaging.
- Treatment may be observation, ultrasound-guided compression, thrombin injection, or surgery depending on the case.
- Prompt recognition ensures the best outcomes and minimizes complications.
References
This article is based on clinical guidelines and expert advice, primarily adapted from Mayo Clinic and related expert sources. For more information or personalized advice, always consult your healthcare provider.
References
- https://www.mymlc.com/health-information/faqs/p/pseudoaneurysm-what-causes-it/
- https://www.mayoclinic.org/tests-procedures/cardiac-catheterization/expert-answers/pseudoaneurysm/faq-20058420
- https://www.ncbi.nlm.nih.gov/books/NBK542244/
- https://my.clevelandclinic.org/health/diseases/23250-pseudoaneurysm
- https://www.mayoclinic.org/tests-procedures/cardiac-catheterization/about/pac-20384695
- https://www.mayoclinic.org/tests-procedures/cardiac-catheterization/care-at-mayo-clinic/pcc-20384697
- https://www.kuh.ku.edu.tr/mayo-clinic-care-network/mayo-clinic-health-information-library/faqs/pseudoaneurysm-what-causes-it
- https://www.mayoclinic.org/tests-procedures/cardiac-catheterization/doctors-departments/pdc-20384696
- https://www.ahajournals.org/doi/full/10.1161/circulationaha.111.043984?doi=10.1161%2FCIRCULATIONAHA.111.043984
Read full bio of Sneha Tete












