Proton Therapy for Prostate Cancer: Precision Treatment and Patient Benefits
Explore how proton therapy delivers targeted prostate cancer treatment with fewer side effects and advancements in radiation technology.
Proton Therapy for Prostate Cancer
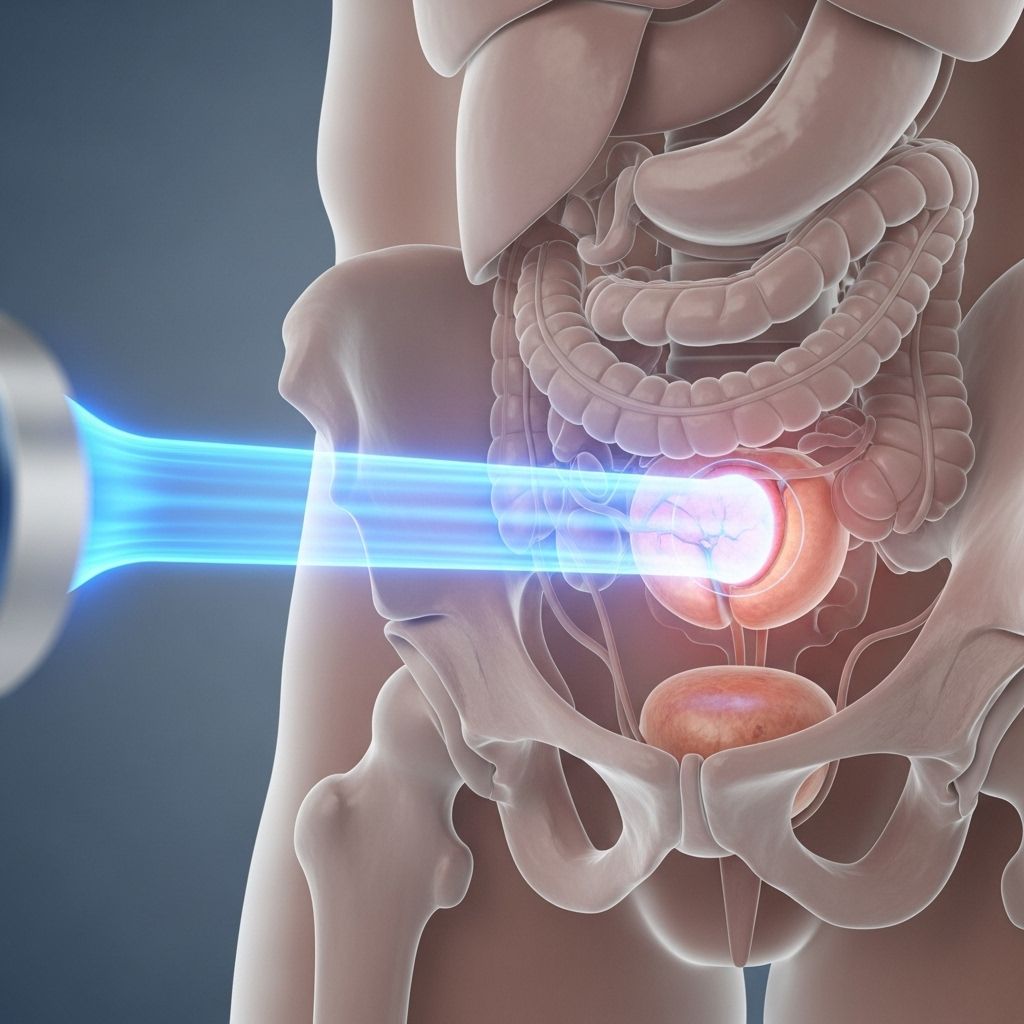
Proton therapy is an advanced form of radiation treatment that targets prostate cancer with remarkable precision. By harnessing the unique physical properties of protons, this therapy offers significant advantages, particularly in minimizing damage to surrounding healthy tissues when compared with traditional photon-based radiation techniques. As a result, proton therapy is increasingly chosen for treating prostate cancer, aiming to reduce side effects without sacrificing effectiveness.
Understanding Proton Therapy
Unlike standard radiation therapy—often referred to as photon or X-ray therapy—proton therapy uses charged particles called protons to deliver energy directly to tumors. The key distinction lies in how each type of treatment delivers and disperses energy as it passes through the body:
- X-ray (photon) therapy delivers radiation along its entire path through the body, including healthy tissues beyond the tumor.
- Proton therapy deposits most of its energy directly in the tumor, with minimal exit dose beyond the target.
This characteristic of protons is known as the Bragg peak, which allows for extremely localized radiation delivery, thus lowering the risk of injuring vital healthy tissues and organs near the prostate, such as the bladder and rectum.
How Proton Therapy Works
Proton therapy utilizes high-energy protons generated and precisely controlled by a device called a cyclotron or synchrotron. This advanced technology permits physicians to “paint” the tumor with radiation, layer by layer, conforming tightly to its three-dimensional shape. The major stages in proton therapy for prostate cancer include:
- Imaging and Planning: Advanced imaging techniques such as MRI and CT scans map the location, size, and shape of the prostate tumor.
- Treatment Simulation: Patients are positioned comfortably and immobilized to ensure precision. Simulation scans help define the optimal entry points and angles for the proton beams.
- Custom Treatment: Using sophisticated software, radiation oncologists design an individualized proton beam distribution that maximizes dose to cancer cells and spares healthy tissues.
- Delivery: During actual treatment (a process often lasting a few minutes per session), proton beams are delivered to the tumor from specific directions based on personalized planning. No incisions or anesthesia are needed.
Benefits of Proton Therapy for Prostate Cancer
- Highly Targeted Radiation: By leveraging the physics of protons, radiation exposure to non-cancerous tissues surrounding the prostate remains significantly lower than with traditional therapies.
- Reduced Side Effects: Limited radiation to the bladder, bowel, and sexual organs generally translates to fewer urinary, rectal, and sexual side effects associated with prostate cancer treatments.
- Lowered Risk of Secondary Cancers: With less overall exposure to radiation-sensitive tissues, the chance of radiation-induced secondary cancers later in life may be reduced.
- Suitability for Recurrent or Previous Radiation Cases: Proton therapy can sometimes be offered to patients who have previously undergone pelvic radiation, providing a treatment option where others may be limited.
- Non-Invasive and Painless: The treatment itself is non-surgical, requires no hospital stay, and is painless—a favorable alternative for many patients.
Comparing Proton Therapy to Conventional Radiation
| Aspect | Proton Therapy | Traditional Photon Therapy |
|---|---|---|
| Radiation Precision | High (Bragg peak, little exit dose) | Lower (more exit dose past tumor) |
| Damage to Nearby Tissues | Minimal | Significant (bladder, rectum, nerves) |
| Pain During Treatment | None | None |
| Usable after Previous Radiation? | Often possible | Usually more limited |
| Availability | Limited to specialized centers | Widely available |
| Cost | Generally higher | Lower |
| Long-Term Data | Emerging, but promising | Extensive |
Candidates for Proton Therapy
Not every prostate cancer patient is automatically a candidate for proton therapy. Selection depends on several factors, including:
- Stage and grade of prostate cancer
- Overall health and pre-existing conditions
- Location and size of the tumor
- Prior history of pelvic radiation
- Personal treatment goals and preferences
A multidisciplinary team will review all relevant information to ensure that proton therapy is appropriate and likely to yield optimal results for each individual.
What to Expect: The Proton Therapy Experience
Patients considering proton therapy for prostate cancer can expect the following general timeline and process:
- Consultation: A comprehensive evaluation to review diagnosis, imaging, and treatment options.
- Treatment Planning: Detailed imaging and simulation visits to develop a tailored approach.
- Daily Treatments: Most patients undergo proton therapy five days a week for several weeks, with each session lasting between 15 and 30 minutes.
- Minimal Disruption: Since treatments are non-invasive and require no recovery time, most patients maintain normal daily activities throughout.
- Follow-Up: Regular check-ins and imaging to monitor response and manage any side effects.
Possible Side Effects and Management
As with all forms of radiation, proton therapy carries the potential for side effects, but these are often less frequent and less severe. Some possible effects include:
- Urinary symptoms (frequency, urgency, discomfort)
- Rectal symptoms (mild bleeding, irritation, diarrhea)
- Fatigue (mild and temporary)
- Rarely, sexual side effects such as erectile dysfunction, though studies suggest these may be less common than with traditional radiation
Many patients find that symptoms resolve within a short period following treatment, and supportive care is available to help manage any discomfort.
Technological Advances in Proton Therapy
Modern proton therapy centers, such as the Johns Hopkins Proton Therapy Center, utilize state-of-the-art technology:
- Pencil Beam Scanning: This method “paints” the tumor with narrow, focused proton streams, further optimizing dose delivery and reducing exposure to nearby organs.
- Robust Imaging Integration: Up-to-date imaging ensures the prostate is accurately targeted while adjusting for any slight movement (such as patient breathing or organ filling).
- Large Research Initiatives: Johns Hopkins and other major institutions are leading large studies to compare the effectiveness and side effect profiles of proton therapy versus conventional treatments for prostate cancer.
Outcomes: Survival, Cure Rates, and Quality of Life
Proton therapy achieves cancer control rates comparable to those of other radiation options for prostate cancer, with up to 90% or more of men with early-stage disease remaining cancer-free several years after treatment. Key outcomes include:
- Cure/Remission Rates: Comparable to other high-quality radiation therapies when used in appropriate patient groups.
- Quality of Life: Preservation of urinary, rectal, and sexual function is often reported as better or similar compared to other modalities.
- Long-Term Safety: Lower rates of severe complications to bladder, rectum, and surrounding tissues.
It is important to note that while the theoretical and early clinical advantages of proton therapy are substantial, ongoing and future randomized trials are necessary to definitively establish its benefits over other radiation methods—especially in light of higher costs and limited availability.
Deciding If Proton Therapy Is Right for You
Selecting the best treatment for prostate cancer is a personal decision, requiring careful consideration of all available options. Factors influencing this choice include:
- Tumor characteristics and stage
- General health and coexisting medical issues
- Risk of side effects and impact on daily life
- Access to specialized centers
- Insurance coverage and cost considerations
Making an informed choice with a trusted medical team—including urologists, radiation oncologists, and oncology nurses—ensures personalized care and the best chance for an optimal outcome.
Frequently Asked Questions About Proton Therapy for Prostate Cancer
Q: What is the main advantage of proton therapy over standard radiation?
A: Proton therapy delivers a highly focused radiation dose to the cancer with almost no radiation passing beyond the tumor, which reduces potential injury to the bladder, rectum, and nerves critical for urinary and sexual function.
Q: Is proton therapy suitable for all prostate cancer patients?
A: Not every patient is an ideal candidate. Factors such as cancer stage, tumor location, previous treatments, and overall health determine eligibility. Consult a proton therapy center for a comprehensive assessment.
Q: What are the side effects of proton therapy for prostate cancer?
A: Most side effects are mild and temporary, including mild urinary or rectal symptoms and fatigue. Severe complications are uncommon, especially when advanced planning and technology are used.
Q: How long does proton therapy take, and what is the schedule?
A: Treatment sessions are typically given five days a week over 4–8 weeks. Each session usually lasts between 15 and 30 minutes, and most patients can return to regular activities immediately afterward.
Q: Is proton therapy covered by insurance?
A: Many insurance plans—especially for prostate cancer—cover proton therapy, but it is wise to verify details with your provider, as costs and coverage may vary.
Q: Are there ongoing studies comparing proton therapy to conventional radiation for prostate cancer?
A: Yes. Several national studies, including those led by major cancer centers, are underway to further clarify differences in outcomes, side effects, and cost-effectiveness for men with prostate cancer.
Conclusion
Proton therapy for prostate cancer represents a major step forward in the evolution of cancer care, combining precision targeting with a proven track record of effectiveness. Its ability to minimize harm to healthy organs and support a good quality of life makes it a compelling option for many patients. However, treatment must be individualized, taking into account each patient’s unique situation, clinical needs, and access to specialized centers.
References
Read full bio of Sneha Tete












