Proton Therapy for Lung Cancer: Benefits, Candidates, and Key Insights
Explore how proton therapy targets lung cancer with precision, reduces side effects, and offers new hope for treatment.
Proton Therapy for Lung Cancer: An In-Depth Guide
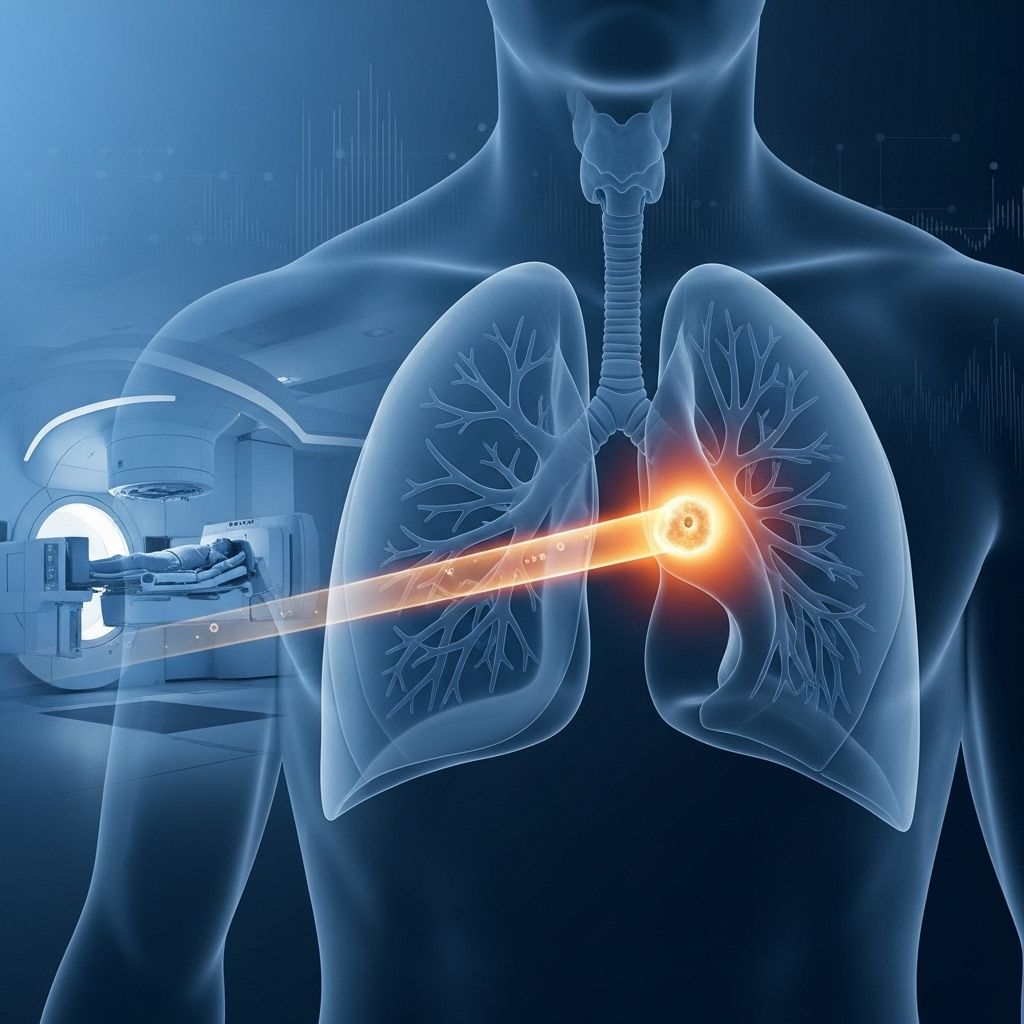
Proton therapy represents a significant advancement in the field of radiation oncology, offering a highly precise approach to treating lung cancer while aiming to minimize damage to healthy tissues. As cancer care evolves, understanding how proton therapy works, its unique benefits, and its role in treating various stages and types of lung cancer is essential for patients and healthcare providers.
Overview: The Role of Radiation Therapy in Lung Cancer
Radiation therapy remains a cornerstone of lung cancer treatment and is often employed alongside surgery, chemotherapy, and more recently, immunotherapy. Traditional external beam radiation uses high-energy waves (typically photons) to target and destroy cancer cells. However, this method can also affect the surrounding healthy tissues, potentially leading to notable side effects—especially since lung tumors often sit near critical organs such as the heart and esophagus.
What Is Proton Therapy for Lung Cancer?
Proton therapy (or proton beam therapy) harnesses the power of positively charged particles—protons—to eradicate malignant cells. While the concept dates back to 1946, technical advancements in the subsequent decades have made proton therapy available in select specialized cancer centers. The therapy’s unique Bragg peak property enables most of the proton’s energy to concentrate precisely at the tumor’s location, thereby delivering maximum destruction to cancer cells while sparing as much healthy tissue as possible.
How Does Traditional Radiation Therapy Work?
- Conventional radiation typically uses photons, which are packets of light energy generated from quickly accelerated electrons.
- Photons pass through the body, depositing energy (and damaging both cancerous and healthy tissue) throughout the pathway.
- The goal is to break the DNA in cancer cells, inhibiting their ability to replicate and grow.
While this approach is effective, the inability to precisely confine radiation energy to the tumor can result in collateral damage to crucial organs nearby, limiting the amount of radiation that can safely be delivered.
How Is Proton Therapy Different?
- Protons are much heavier (about 800 times more massive than electrons) and can be precisely delivered using special accelerators known as synchrotrons or cyclotrons.
- The penetration depth of protons is carefully calibrated so that the maximum amount of energy is released at the tumor site (the Bragg peak), with minimal exit dose beyond the cancerous tissue.
- This concentrated dose reduces harm to surrounding healthy tissues, which is especially valuable when the tumor is close to sensitive structures like the heart, lungs, or spinal cord.
What Are the Advantages of Proton Therapy for Lung Cancer?
Proton therapy offers several distinct advantages over traditional photon-based radiation, especially for lung cancers located near critical organs or in patients who are sensitive to side effects:
- Reduces damage to vital organs: Research demonstrates that proton therapy can decrease injury to the esophagus, healthy lung tissue, and heart compared to conventional radiation. This is particularly important since these organs are often at risk during treatment.
- Potential for higher radiation doses: By sparing healthy tissues, proton therapy sometimes allows clinicians to safely deliver higher, potentially more effective doses of radiation to the tumor.
- Improved survival rates for certain groups: Some studies highlight improved overall survival in people with locally advanced non-small cell lung cancer (NSCLC) who receive proton therapy.
- Lower toxicity and fewer side effects: Proton therapy may reduce both immediate and long-term side effects, including painful swallowing, radiation pneumonitis, and cardiac issues.
- An alternative when surgery is not feasible: For specific tumors that cannot be safely removed via surgery, such as ground glass opacity lung cancers, proton therapy provides a valuable alternative.
- Facilitates combined treatment: The reduced toxicity profile may allow for intensification of chemotherapy alongside radiation, improving overall treatment outcomes in some instances.
Evidence-Based Benefits of Proton Therapy
| Benefit | Evidence/Study |
|---|---|
| Reduced organ damage | 2018 study: Lower rates of harm to esophagus, lung tissue, heart versus traditional therapy |
| Better survival | 2021 study: Higher survival rates and low toxicity in certain advances of NSCLC |
| Comparable to surgery for early stage | 2017 study: Equal or better outcomes for early-stage NSCLC, with less toxicity |
| Alternative to surgery | 2020 study: Effective where surgery is not possible, especially in ground glass opacity lung cancer |
| Supports more intensive therapy regimens | Early studies: Allows for more aggressive chemoradiation strategies |
Who Is an Ideal Candidate for Proton Therapy?
Not every patient with lung cancer will benefit equally from proton therapy. Ideal candidates generally include:
- People with locally advanced non-small cell lung cancer (NSCLC): Especially those with tumors near vital organs
- Elderly or medically inoperable patients: Individuals for whom surgery presents a high risk due to other health issues
- Patients requiring retreatment: When cancer recurs in an area previously treated with radiation, proton therapy’s precise targeting can help lower cumulative side effects
- Patients with small cell lung cancer: Certain cases may benefit based on tumor location and medical history
- Cases near sensitive tissues: Cancer located close to the heart, spinal cord, esophagus, or remaining healthy lung tissue
Each case requires careful assessment by a multidisciplinary oncology team to determine if proton therapy offers a meaningful advantage over other modalities based on tumor anatomy, staging, and individual health factors.
Types of Lung Cancer Treated with Proton Therapy
- Non-small cell lung cancer (NSCLC): Stages I, II, and III are commonly considered for proton treatment, especially locally advanced or inoperable cases.
- Small cell lung cancer: Although less common, proton therapy is an option for some.
- Other rare tumors: Tumors adjacent to critical organs, recurrent lesions, or unique anatomical challenges may also be considered.
Potential Side Effects of Proton Therapy
Although proton therapy is known for its ability to reduce side effects compared to conventional radiation, no cancer treatment is without some risks or adverse reactions. The specific experience depends on the amount of radiation delivered, tumor location, overall health, and whether treatment is combined with chemotherapy or immunotherapy.
Possible Side Effects Include:
- Fatigue: A common side effect during and shortly after therapy
- Irritation of the lung tissue (pneumonitis): Shortness of breath, cough, or mild chest pain arising weeks to months after completing therapy
- Esophagitis: Difficulty or pain with swallowing, mainly if the treated area is near the esophagus
- Skin changes: Mild redness, itching, or dryness at the entrance site of the proton beam
- Cardiac risk: This risk is generally much lower with proton therapy but still possible if tumors are adjacent to the heart
Most side effects are temporary and manageable, and serious long-term complications are less likely with proton therapy compared to traditional radiation, thanks to greater control over where the dose ends within the body.
Comparison: Proton Therapy vs. Traditional Radiation Therapy
| Aspect | Proton Therapy | Traditional Radiation (Photon/X-ray) |
|---|---|---|
| Type of Particle | Protons (positive charge) | Photons (X-rays, neutral) |
| Energy Distribution | Major energy at tumor site (Bragg peak) | Energy distributed along entry and exit path |
| Impact on Healthy Tissue | Significantly minimized | Higher risk, especially near vital organs |
| Suitability | Tumors near critical organs; pts needing retreatment; inoperable tumors | Most lung cancers, especially accessible or not adjacent to highly sensitive organs |
| Availability | Limited, found at specialized centers | Widely available at cancer treatment facilities |
| Side Effect Profile | Generally lower | Potentially higher, especially with higher doses |
Frequently Asked Questions (FAQs)
How is proton therapy delivered for lung cancer?
Proton therapy is administered at specialized cancer centers using advanced machines (synchrotrons or cyclotrons) that accelerate protons to energies sufficient to penetrate to the lung tumor. The process is non-invasive, similar in physical sensation to traditional radiation sessions, and generally occurs Monday through Friday for several weeks, depending on the cancer stage and treatment plan.
Does proton therapy cure lung cancer?
While proton therapy is a curative treatment in many early-stage cases and those unsuitable for surgery, its overall effectiveness—like all lung cancer therapies—depends on the cancer stage, tumor location, and patient health. It is often combined with chemotherapy and/or surgery to maximize outcomes.
Is proton therapy covered by insurance?
Certain insurance plans may cover proton therapy, particularly if it is determined to offer a clear benefit over other radiation modalities (such as for tumors located near critical structures). However, coverage criteria vary, and preauthorization is typically required. Patients should speak with their treatment center and insurance provider early in the process.
Are there limitations to proton therapy?
- Not all cancer centers have the equipment or expertise to provide proton therapy, limiting its availability.
- More clinical research is still underway to determine which lung cancer patients benefit the most over other forms of radiation.
- The cost of proton therapy is often higher than traditional approaches.
Can proton therapy be combined with other treatments?
Yes, proton therapy is frequently used alongside chemotherapy, and in selected cases, surgery or immunotherapy. The ability to combine treatments safely often depends on reducing overlapping side effects, which is a key benefit of protons’ precise delivery.
Takeaway: Is Proton Therapy Right for You?
For many patients, proton therapy represents a state-of-the-art option that can offer finely-targeted lung cancer treatment while aiming to preserve normal breathing, heart function, and overall quality of life. The best candidates are those whose tumors are located near critical organs or those who cannot undergo surgery. However, due to limited availability and higher cost, proton therapy’s use is often reserved for select cases after multidisciplinary evaluation. Always discuss all treatment options, benefits, and risks with your oncologist to find the most appropriate approach tailored to your unique situation.
Frequently Asked Questions (FAQ)
Q: Who should consider proton therapy for lung cancer?
A: People with tumors near vital organs, those ineligible for surgery, or those who need retreatment may benefit most. A thorough evaluation by a specialized cancer care team is necessary.
Q: Are the side effects of proton therapy permanent?
A: Most side effects—such as fatigue, mild skin changes, or irritation of lung tissues—are temporary and resolve after treatment ends. Long-term risks are lower compared to traditional radiation, but some late effects are still possible.
Q: How does proton therapy compare in cost to traditional radiation?
A: Proton therapy can be considerably more expensive due to the complex equipment and technology required. Insurance coverage varies, so patients should check with their provider and treatment center regarding costs and eligibility.
Q: Where is proton therapy for lung cancer available?
A: Proton therapy is available at major cancer centers that have the necessary specialized equipment and trained staff. Facilities are more common in major cities and university-affiliated hospitals.
Q: Can proton therapy be repeated if cancer recurs?
A: Proton therapy’s precise delivery can sometimes allow for safe retreatment, but this depends on the location of the recurrence and prior radiation exposure. Each case must be individually assessed by radiation oncology specialists.
References
- https://www.healthline.com/health/lung-cancer/proton-therapy-for-lung-cancer
- https://www.protoncenter.nm.org/en/cancers-tumors-treated/lung-cancer
- https://www.floridaproton.org/ppc/lung-small-cell
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6050808/
- https://www.healthline.com/health/external-beam-radiation-therapy
- https://californiahealthline.org/news/boom-in-proton-therapy-is-a-bust-for-some-blame-a-shortage-of-patients/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7066957/
- https://onlinelibrary.wiley.com/doi/10.1111/j.1759-7714.2011.00098.x
Read full bio of Sneha Tete












