Prolymphocytic Leukemia vs. CLL: Symptoms, Causes, Treatments
Comprehensive comparison of prolymphocytic leukemia and chronic lymphocytic leukemia, from symptoms to treatment and long-term outlook.
Prolymphocytic Leukemia vs. Chronic Lymphocytic Leukemia (CLL): Causes, Symptoms, Treatment, and More
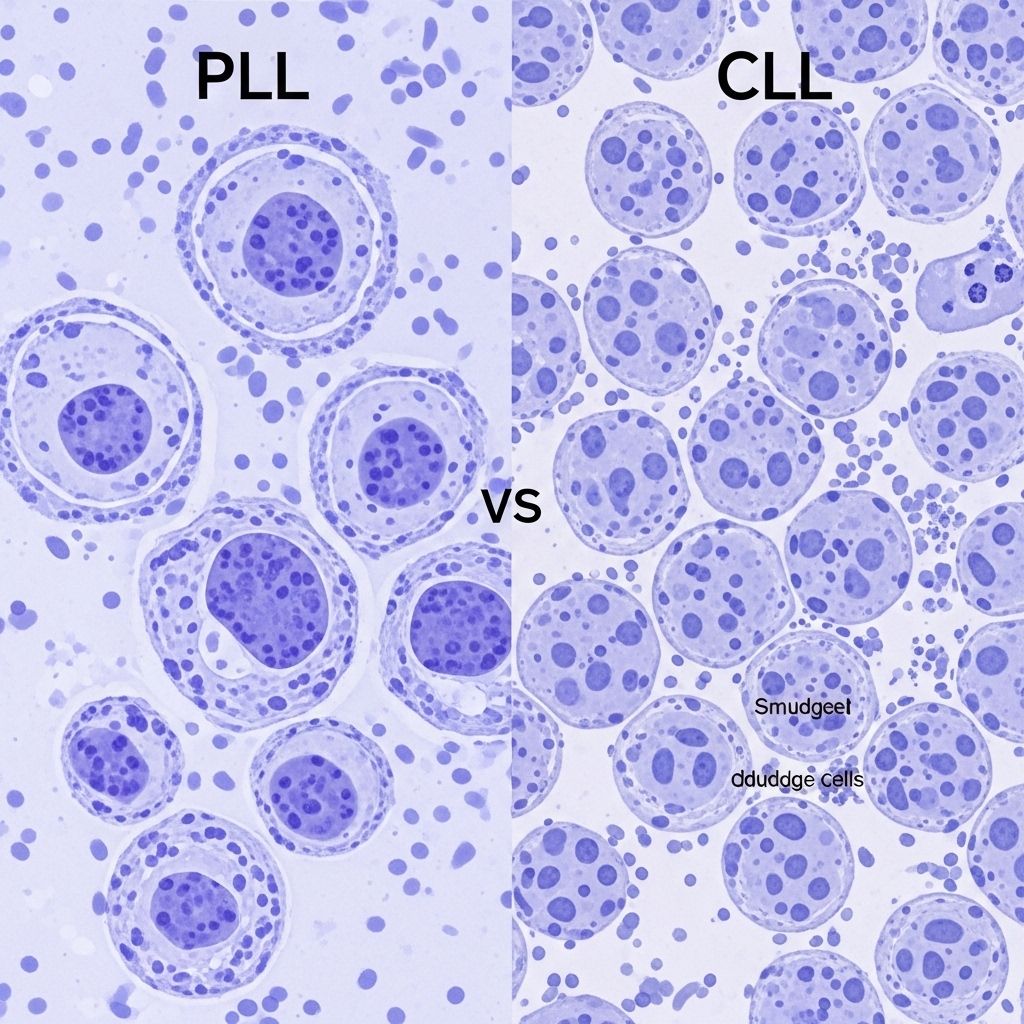
Chronic lymphocytic leukemia (CLL) and prolymphocytic leukemia (PLL) are types of blood cancer that affect white blood cells, yet they differ in aggressiveness, symptoms, causes, treatment, and prognosis. Understanding these differences is crucial for patients navigating diagnosis or seeking information about these rare malignancies.
What Are Prolymphocytic Leukemia (PLL) and Chronic Lymphocytic Leukemia (CLL)?
Leukemia is a broad category of cancers that originate in the tissues that create blood cells, primarily affecting the production and function of white blood cells. The classification of leukemia is based on the type of cell affected and the speed of disease progression.
Chronic lymphocytic leukemia (CLL) is the most common type of leukemia in adults. The term “chronic” denotes slow progression, while “lymphocytic” refers to its origin in lymphocytes, a subtype of white blood cells. CLL typically develops from B cells (a type of lymphocyte) and progresses over many years.
Prolymphocytic leukemia (PLL) is much rarer and tends to be more aggressive. Once considered a variant of CLL, PLL is now recognized as a separate disease entity. PLL arises from mature lymphocytes called prolymphocytes and is further divided into B-cell and T-cell subtypes, though recent classifications have redefined the B-cell form under related lymphoma categories, such as mantle cell lymphoma.
Symptoms: How Do PLL and CLL Differ?
Both PLL and CLL present with symptoms that can overlap and may be general or vague, making diagnosis challenging without laboratory testing. However, there are distinguishing features related to disease progression and cell types involved.
Symptoms of Prolymphocytic Leukemia (PLL)
- Swollen lymph nodes
- Enlarged liver or spleen (hepatosplenomegaly)
- Night sweats
- Unintentional weight loss
- Skin rashes or lesions
- Abnormal blood counts:
- Elevated white blood cell count
- Low red blood cell count (anemia)
- Low platelet count (thrombocytopenia)
Symptoms of Chronic Lymphocytic Leukemia (CLL)
- Progressive fatigue
- Shortness of breath
- Night sweats
- Low-grade fever
- Lymph node enlargement
- Loss of appetite
- Unintentional weight loss
- Decreased red blood cell count (anemia)
- Increased susceptibility to infections
- Enlarged spleen or liver
Notably, CLL symptoms often develop slowly and may be mistaken for other conditions or simply signs of aging, while PLL symptoms are typically more severe and progress rapidly, reflecting PLL’s aggressive nature.
What Causes Prolymphocytic Leukemia and CLL?
Both PLL and CLL result from genetic mutations that lead to uncontrolled replication of abnormal lymphocytes. However, the precise triggers for these mutations remain largely unknown for both conditions.
Causes of Prolymphocytic Leukemia (PLL)
- Arises from mature T cells (T-cell PLL) or previously, mature B cells (B-cell PLL), although B-cell PLL is now less commonly diagnosed due to reclassification.
- Usually, no clearly identifiable cause.
- Genetic alterations drive the abnormal growth and replication of prolymphocytes.
- In T-cell PLL, aggressive behavior is typical, with limited understanding of environmental or hereditary triggers.
Causes of Chronic Lymphocytic Leukemia (CLL)
- Develops from genetic changes in B lymphocytes.
- Exact causes remain uncertain, and like PLL, most cases occur without a clear precipitating factor.
- Underlying genetic mutations result in excessive proliferation of lymphocytes in the bone marrow and blood.
Risk Factors for Developing PLL or CLL
While direct causes are elusive, certain risk factors increase the likelihood of developing these blood cancers, especially CLL.
Risk Factors for CLL
- Age: Most patients are diagnosed over age 60.
- Gender: More prevalent in men than in women.
- Race/ethnicity: Higher incidence in people of European descent.
- Family history: Increased risk with a close family member diagnosed with CLL or related lymphoid cancers.
- Exposure to certain chemicals: Such as those found in herbicides or pesticides (e.g., Agent Orange), although the association remains weak.
Due to its rarity, risk factors for PLL are less well-defined but are presumed to overlap with those of CLL in some cases. However, PLL does not show the same clear association with age, gender, or family history as CLL.
Getting Medical Care: When to See a Doctor
If you experience persistent symptoms such as unexplained fatigue, recurrent infections, swollen lymph nodes, or constant night sweats, it is important to seek medical evaluation. Early detection can improve management outcomes, even for aggressive diseases like PLL.
How Are Prolymphocytic Leukemia and CLL Diagnosed?
Diagnosis for both diseases involves a combination of clinical examination, laboratory tests, and advanced imaging. Because symptoms can be nonspecific and overlap with other conditions or leukemia subtypes, accurate diagnosis is essential to guide treatment.
Diagnostic Approaches
- Blood tests: Evaluate complete blood count (CBC), presence of atypical lymphocytes, and levels of red cells and platelets.
- Peripheral blood smear: Used to assess the appearance and proportions of lymphocytes, prolymphocytes, and other blood cells.
- Bone marrow biopsy and aspirate: Determines the extent of disease and cell type.
- Immunophenotyping by flow cytometry: Distinguishes between different types of lymphocytes by their surface markers (e.g., CD5, CD19, CD23 in CLL; different patterns in PLL).
- Genetic and cytogenetic testing: Identifies chromosomal abnormalities and specific gene mutations that define prognosis or influence treatment.
- Imaging studies: Such as ultrasound or CT scan to detect lymph node enlargement and organ involvement.
Advanced genetic and molecular diagnostics now allow for more precise classification, especially distinguishing B-PLL from other indolent or aggressive B-cell lymphomas.
How Are Prolymphocytic Leukemia and CLL Treated?
Treatment strategies depend on the disease subtype, degree of aggressiveness, stage at diagnosis, patient comorbidities, and molecular/genetic features revealed through testing.
General Treatment Principles
- Observation (“watch and wait”): Often used in CLL, especially for early-stage, asymptomatic disease.
- Chemotherapy: Common regimens include alkylating agents, purine analogs, and combination therapies. More frequently needed for symptomatic or advanced CLL and virtually always for PLL.
- Targeted therapies: Newer drugs such as BTK inhibitors (e.g., ibrutinib), BCL-2 inhibitors (e.g., venetoclax), and PI3K inhibitors are increasingly replacing traditional chemotherapy, especially in relapsed or refractory CLL.
- Immunotherapy: Monoclonal antibodies targeting CD20 (e.g., rituximab, obinutuzumab) or other cell surface proteins, are often used in combination therapy.
- Stem cell transplantation: May be considered in younger, fit patients with poor-risk disease, particularly in relapsed PLL.
- Supportive care: Includes transfusions, antibiotics for infection prevention, and treatments for anemia or thrombocytopenia.
| Treatment Approach | Chronic Lymphocytic Leukemia (CLL) | Prolymphocytic Leukemia (PLL) |
|---|---|---|
| Observation | Common in early-stage/smoldering CLL | Rarely used; disease usually aggressive |
| Chemotherapy | Varied regimens, often in advanced or symptomatic disease | Common, usually combined with immunotherapy |
| Targeted Therapies | BTK/BCL-2/PI3K inhibitors | Some cases use similar agents |
| Immunotherapy | Rituximab, obinutuzumab, etc. | May be used, especially anti-CD52 antibody (alemtuzumab) in T-PLL |
| Transplantation | Rare, reserved for relapsed/refractory disease | Considered in eligible cases |
| Supportive Care | Important in infection prevention and cytopenias | Essential due to high symptom burden |
Prognosis: What Is the Outlook for PLL and CLL?
The prognosis for CLL and PLL varies considerably, chiefly due to differences in progression rates and response to treatment.
Chronic Lymphocytic Leukemia (CLL)
- CLL typically progresses slowly. Many patients live for years or even decades following diagnosis.
- Median survival ranges from 8–12 years, dependent on genetic mutations, disease stage, and response to newer therapies.
Prolymphocytic Leukemia (PLL)
- PLL is more aggressive, with a median survival of 2–3 years for T-PLL and previously reported 3–5 years for B-PLL, though newer therapies may improve survival in select cases.
- Risk stratification models consider genetic mutations, such as MYC and 17p abnormalities, to guide prognosis.
- Response to standard therapies is often poorer compared to CLL.
Can Prolymphocytic Leukemia and CLL Be Prevented?
Currently, there are no proven strategies to prevent PLL or CLL, largely because the primary causes remain unknown. General recommendations for health maintenance, including delaying exposure to potential carcinogens and regular medical checkups for those at higher risk, may help identify illness early but do not guarantee prevention.
Frequently Asked Questions
Q: What is the main difference between PLL and CLL?
A: PLL is typically a more aggressive cancer involving mature prolymphocytes, whereas CLL usually progresses slowly and arises from mature B lymphocytes.
Q: Is prolymphocytic leukemia the same as CLL?
A: No. PLL was once considered a subtype of CLL but is now recognized as a separate entity, especially in the case of T-PLL. B-cell PLL has been reclassified under different lymphoma types in recent guidelines.
Q: Can CLL turn into PLL?
A: Rarely, CLL can transform into a more aggressive form similar to PLL, but most PLL cases arise independently. Such transformations are often linked to changes in cell type and appearance.
Q: How are these leukemias treated?
A: CLL is often managed with a watch-and-wait approach in early cases, with more advanced stages treated using chemotherapy, targeted drugs, or immunotherapies. PLL, being more aggressive, usually requires immediate and intensive treatment, potentially including stem cell transplantation.
Q: What is the long-term outlook?
A: CLL has a relatively favorable prognosis for many patients, but PLL unfortunately has a poorer outlook due to its aggressive nature and lower responsiveness to available treatments.
Summary
Both CLL and PLL are rare hematologic cancers with overlapping but distinct features. CLL is common in older adults and progresses slowly, often allowing patients to live normal or near-normal lifespans. In contrast, PLL is much rarer and typically aggressive, especially in its T-cell form, demanding prompt diagnosis and intensive therapy. Ongoing research into genetics, immunophenotyping, and new therapies continues to reshape understanding and management of these complex blood cancers.
References
Read full bio of medha deb












