Prolymphocytic Leukemia: Causes, Symptoms, Diagnosis, and Treatment Options
Learn about prolymphocytic leukemia, its symptoms, risk factors, diagnosis, and the latest treatment and management options.
Prolymphocytic Leukemia: Understanding a Rare and Fast-Growing Blood Cancer
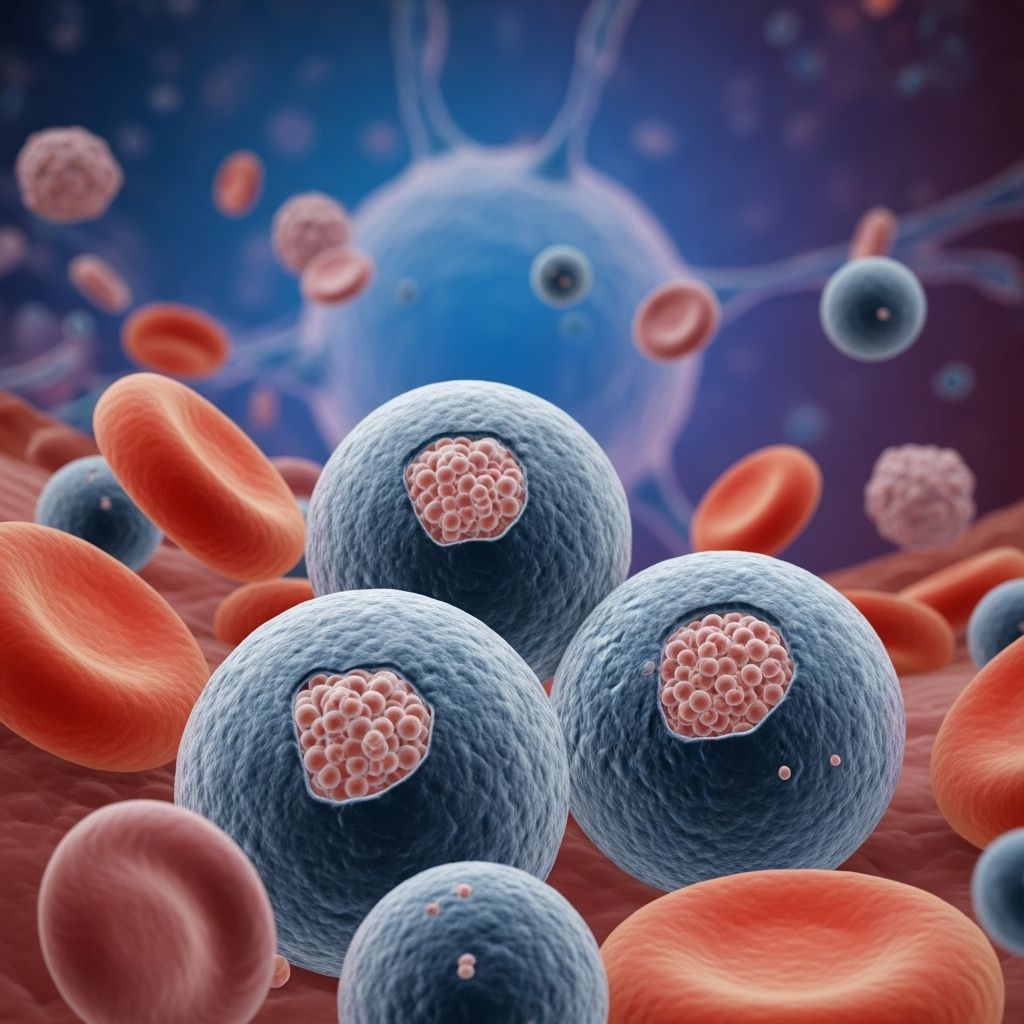
Prolymphocytic leukemia (PLL) is a rare and aggressive type of leukemia characterized by the uncontrolled proliferation of immature lymphocytes called prolymphocytes. Affecting both B-cells and T-cells, PLL can progress rapidly and requires prompt diagnosis and intervention. This article provides a comprehensive overview of PLL: its causes, symptoms, risk factors, diagnosis, available treatments, and advice on living with this condition.
What Is Prolymphocytic Leukemia?
Prolymphocytic leukemia is a cancer that arises from white blood cells—either B-lymphocytes or T-lymphocytes—in their immature prolymphocyte stage. These abnormal cells multiply uncontrollably, overwhelming the bone marrow and bloodstream, and may infiltrate organs such as the liver, spleen, and lymph nodes. PLL differs from other forms of leukemia by its highly aggressive nature and distinctive pathological features.
- B-cell prolymphocytic leukemia (B-PLL): Accounts for most cases, originates from malignant B-lymphocytes.
- T-cell prolymphocytic leukemia (T-PLL): Less common, derives from malignant T-lymphocytes and is known for its aggressiveness.
How Common Is Prolymphocytic Leukemia?
PLL is extremely rare, affecting only a small fraction of all chronic lymphocytic leukemias. It more often impacts people above the age of 60, but can occur at other ages as well. Men are slightly more likely to be diagnosed with PLL than women.
B-Cells and T-Cells: The Cells Involved
Understanding the underlying cell types helps clarify the disease process:
- B-lymphocytes (B-cells): A type of immune cell whose main function is to produce antibodies to fight infection.
- T-lymphocytes (T-cells): Another immune cell type, T-cells help destroy infected or abnormal cells and assist other immune processes.
In PLL, the transformation and rapid multiplication of immature versions of these cells (prolymphocytes) drive disease progression.
Types of Prolymphocytic Leukemia
| Type | Description | Prevalence |
|---|---|---|
| B-cell Prolymphocytic Leukemia (B-PLL) | Originates from abnormal B-cells, most common form. | ~80% of cases |
| T-cell Prolymphocytic Leukemia (T-PLL) | Arises from abnormal T-cells, especially aggressive. | ~20% of cases |
Symptoms and Signs of Prolymphocytic Leukemia
The symptoms of PLL can be nonspecific at first and may vary between individuals. However, as the disease progresses, certain features become prominent:
- Fatigue
- Fever and night sweats
- Unintentional weight loss
- Enlarged lymph nodes (neck, armpits, groin)
- Swollen spleen or liver (hepatosplenomegaly)
- Paleness and anemia (from decreased red blood cell production)
- Easy bruising or bleeding (due to low platelet counts)
- Frequent, severe, or prolonged infections
- Shortness of breath
- Bone or joint pain
- Skin rashes or lesions
- Pain or fullness in the abdomen (from organ enlargement)
- Persistent cough
Not everyone will experience all symptoms, and some signs may be subtle—prompt evaluation is essential if any concerning symptoms appear.
How Is Prolymphocytic Leukemia Diagnosed?
Diagnosis involves several steps aimed at confirming PLL, distinguishing it from other blood cancers, and assessing disease severity. The key diagnostic tests include:
- Physical examination: Checking for lymph node, spleen, or liver enlargement.
- Blood tests: Complete blood count (CBC) often reveals high lymphocyte counts with abnormal cells.
- Blood smear: Microscopic inspection of blood cells to identify prolymphocytes.
- Immunophenotyping: Laboratory techniques (like flow cytometry) distinguish B-PLL from T-PLL and other leukemias.
- Bone marrow biopsy: Examines marrow tissue for cancerous cells.
- Genetic studies: Identifies chromosomal or genetic changes linked to PLL types, such as TP53 mutations in B-PLL or TCL1A and ATM mutations in T-PLL.
- Imaging studies: CT or ultrasound to assess internal organ involvement.
Causes and Risk Factors
The exact cause of PLL remains unclear. Researchers believe a combination of genetic and possibly environmental factors contribute:
- Genetic mutations: Inherited or acquired changes in genes such as TP53 (for B-PLL) or TCL1A and ATM (for T-PLL) can drive abnormal cell growth.
- Age: PLL is most common in those over age 60.
- Male sex: Slightly higher risk in men.
- History of other hematological disorders: Rare instances of PLL developing after other blood cancers, but this link is not strong.
Currently, there are no well-established environmental risk factors or preventive measures.
Complications of Prolymphocytic Leukemia
Possible complications stem both from the cancer itself and the effects of treatment:
- Severe infections: Due to an impaired immune system.
- Anemia and low platelets: Leading to weakness, fatigue, easy bruising, and bleeding.
- Organ dysfunction: From invasion of liver, spleen, bone marrow.
- Other cancers: Slightly increased risk of secondary malignancies, especially after certain treatments.
- Treatment side effects: Chemotherapy, immunotherapy, and transplant can cause short- and long-term adverse effects.
Treatment Options for Prolymphocytic Leukemia
Therapy is tailored to each person’s form of PLL, overall health, age, and disease characteristics. Management often involves a multidisciplinary team of specialists.
Initial Management: Watchful Waiting
Some PLL patients without significant symptoms or with slow-progressing disease may be monitored closely rather than treated immediately. This approach, 7atchful waiting, relies on regular checkups, blood tests, and symptom monitoring. Active treatment begins if progression occurs or symptoms worsen.
Active Treatments
- Chemotherapy: Combination chemotherapy drugs are used to reduce the number of abnormal prolymphocytes. B-PLL in particular can be resistant to standard chemotherapy due to TP53 mutations, so treatment regimens may be customized for each patient.
- Immunotherapy: Medications like alemtuzumab target specific proteins on leukemia cells, helping the immune system destroy them. Alemtuzumab is often used as first-line treatment in T-PLL and is considered highly effective initially.
- Targeted therapies: Newer medications that disrupt molecular pathways driving leukemia growth are in development and may be available through clinical trials.
- Stem cell transplantation (bone marrow transplant): For eligible, fit patients, an allogeneic (donor) stem cell transplant can provide a chance for long-term remission, especially in younger individuals. However, the majority of patients are ineligible for transplant because of age or health status.
Each treatment option carries potential side effects and risks. Your doctor will review the benefits and drawbacks based on your circumstances.
Symptom and Supportive Management
- Infection prevention and management: Prompt treatment of infections and, in many cases, prophylactic (preventive) antibiotics or antifungals.
- Blood transfusions: May be given to help combat anemia or low platelets.
- Medications: To relieve symptoms such as pain, fever, or nausea.
- Emotional support and counseling: Coping with a cancer diagnosis is stressful and support groups, counseling, or social work services can help.
Outlook and Prognosis
Prolymphocytic leukemia is considered an aggressive leukemia with a poorer prognosis than many other leukemias. The outlook varies by type:
- B-PLL: Survival is quite variable but generally ranges from several months to a few years, even with treatment.
- T-PLL: Has a very rapid course. Median survival is usually less than 1 years after diagnosis for most patients, despite recent advances.
Participation in clinical trials and early access to new treatments may improve outcomes. Ongoing follow-up is crucial even after remission, as relapses are common.
Living With Prolymphocytic Leukemia
A diagnosis of prolymphocytic leukemia can be overwhelming for you and your loved ones. Practical steps can help manage day-to-day life:
- Follow your treatment plan: Adhere closely to medications and appointments.
- Monitor for infection: Watch for fevers, cough, and other signs that require urgent medical attention.
- Maintain good nutrition and rest: A balanced diet and sleep can help boost energy and immune function.
- Seek emotional support: Join support groups, counseling, or talk openly with family and friends.
- Plan for the future: Consider advanced care planning; discuss wishes with your healthcare provider and family members.
Frequently Asked Questions (FAQs)
Q: Is prolymphocytic leukemia curable?
A: Currently, prolymphocytic leukemia is not considered curable for most patients. Treatment can help control symptoms and extend life, and ongoing research may offer more options in the future.
Q: What is the difference between B-PLL and T-PLL?
A: The main difference lies in the cell origin: B-PLL arises from B-lymphocytes and is the more common form, while T-PLL originates from T-lymphocytes and usually has a more aggressive clinical course.
Q: What tests are used to diagnose prolymphocytic leukemia?
A: Diagnosis typically involves blood tests, blood smear, immunophenotyping, bone marrow biopsy, genetic studies, and imaging scans.
Q: Can prolymphocytic leukemia be inherited?
A: There is currently no evidence that prolymphocytic leukemia is directly inherited. However, certain genetic mutations acquired during a person’s life increase susceptibility.
Q: Are there experimental or new treatments available?
A: Yes. Clinical trials are ongoing for new drugs and therapies, particularly targeted therapies and improved transplant methods. Patients may be eligible to participate in these research studies.
Key Takeaways
- Prolymphocytic leukemia is a rare, aggressive cancer of lymphocytes, most commonly affecting older adults.
- Symptoms often include fatigue, fevers, weight loss, swollen nodes, and frequent infections.
- Diagnosis is based on blood and marrow tests, as well as genetic analysis.
- Treatment may involve a combination of watchful waiting, chemotherapy, immunotherapy, and, in select cases, stem cell transplantation.
- Ongoing research is expanding the range of available therapies for this challenging disease.
Resources and Support
- Talk with your healthcare team about treatment options and supportive care.
- Connect with patient support groups and advocacy organizations for additional information and emotional support.
- Consider participating in clinical trials if eligible.
References
- https://withoutaribbon.org/prolymphocytic-leukemia-symptoms-treatment-support/
- https://en.wikipedia.org/wiki/B-cell_prolymphocytic_leukemia
- https://healthtree.org/b-cell-prolymphocytic-leukemia/community/what-are-the-signs-and-symptoms-of-b-cell-prolymphocytic-leukemia
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10419310/
- https://www.leukaemiacare.org.uk/support-and-information/information-about-blood-cancer/blood-cancer-information/leukaemia/prolymphocytic-leukaemia-pll/
- https://www.medicalnewstoday.com/articles/prolymphocytic-leukemia
- https://rarediseases.info.nih.gov/diseases/13731/t-cell-prolymphocytic-leukemia
- https://www.healthline.com/health/leukemia/t-cell-leukemia
- https://healthtree.org/t-cell-prolymphocytic-leukemia/community/what-are-the-signs-and-symptoms-of-t-cell-prolymphocytic-leukemia
Read full bio of medha deb












