Proliferative Diabetic Retinopathy: Prevention, Symptoms, and Treatment
Everything you should know about the advanced stage of diabetic retinopathy, its risks, symptoms, and available treatments.
Proliferative Diabetic Retinopathy: What You Should Know
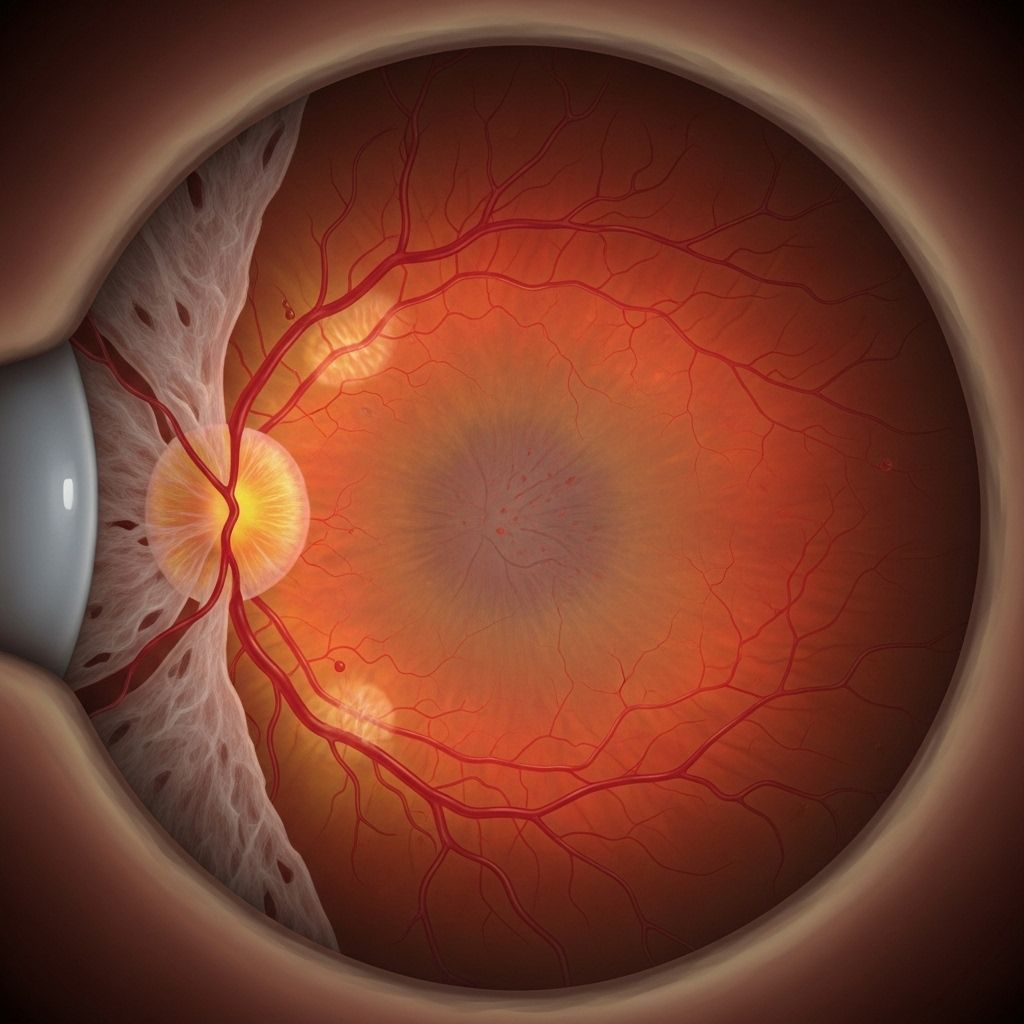
Proliferative diabetic retinopathy (PDR) is the advanced, vision-threatening stage of diabetic eye disease. People with diabetes, especially with poor blood sugar control, face increased risk of developing this serious condition that can eventually lead to vision loss or blindness if left untreated. In this comprehensive guide, you’ll learn how PDR develops, key symptoms to watch for, who’s most at risk, how it’s diagnosed, current treatment options, and important strategies to protect your vision.
About Diabetic Retinopathy
Diabetic retinopathy encompasses a spectrum of retinal complications caused by diabetes. Chronic elevated blood sugar damages the tiny blood vessels (capillaries) that nourish the retina, ultimately cutting off its blood supply. There are two major stages:
- Nonproliferative diabetic retinopathy (NPDR): The early, more common stage, marked by weakened blood vessels that may leak fluid and blood, causing retinal swelling or edema.
- Proliferative diabetic retinopathy (PDR): The advanced, more severe stage, defined by the growth (“proliferation”) of abnormal new blood vessels in response to poor retinal circulation and oxygen deprivation.
While NPDR may cause mild symptoms—or none at all—PDR often leads to serious vision changes and complications.
What Is Proliferative Diabetic Retinopathy?
In PDR, new, fragile blood vessels grow inside the retina and sometimes into the vitreous—the clear, gel-like substance filling the eye. This abnormal growth is called neovascularization, a process triggered by lack of oxygen and poor circulation in the retinal tissue.
Unfortunately, these new vessels are structurally weak and highly prone to leaking or bleeding. If left untreated, the ongoing process can damage the retina, cause scarring and traction, and even lead to total vision loss.
- Bleeding (vitreous hemorrhage): Blood leaks into the center of the eye, blocking light and blurring vision.
- Tractional retinal detachment: Scar tissue from abnormal vessels can pull the retina away from the back of the eye.
- Glaucoma: New vessels sometimes block normal eye fluid drainage, causing increased pressure that damages the optic nerve.
How PDR Develops Over Time
Diabetic retinopathy is progressive. The transition from nonproliferative to proliferative stages often takes years. Early on, people may have no symptoms. As neovascularization advances, however, noticeable vision symptoms and complications emerge.
Who Is Most at Risk?
PDR affects people with both type 1 and type 2 diabetes. However, certain factors increase the risk:
- Longer duration of diabetes
- Poorly controlled blood sugar (high HbA1c levels)
- High blood pressure (hypertension)
- High cholesterol
- Diabetic kidney disease (nephropathy)
- Diabetic nerve damage (neuropathy)
- Tobacco use
- Pregnancy
- Younger people with insulin-dependent diabetes are particularly vulnerable
- Ethnic background: Black, Latino, and other minorities face higher risk
Symptoms of Proliferative Diabetic Retinopathy
The early stages of diabetic retinopathy, including PDR, may not cause symptoms. That’s why regular eye exams are essential for people with diabetes. As PDR worsens, common symptoms include:
- Eye floaters: Tiny dark specks or cobwebs that appear to drift through your vision
- Blurry or cloudy vision: Often due to bleeding or swelling within the retina
- Dark or empty spots: Central vision may be affected, leading to blind spots
- Trouble seeing at night: Night vision may be compromised
- Sudden, severe, painless vision loss: May occur if bleeding or retinal detachment happens abruptly
- Color vision changes: Colors may appear faded or distorted
Symptom severity often correlates with the degree and location of retinal damage. If you experience any sudden vision changes, seek prompt medical attention.
How Is Proliferative Diabetic Retinopathy Diagnosed?
Diagnosis requires an ophthalmologic examination, typically including:
- Dilated eye exam: Drops enlarge the pupil for a detailed view of the retina and blood vessels
- Retinal imaging: Techniques like Optical Coherence Tomography (OCT) assess retinal thickness and swelling, while fluorescein angiography highlights abnormal vessels and areas of leakage
- Vision tests: Evaluate how well you see, including central and peripheral vision
Regular screening is crucial for early detection. Even if you have no symptoms, most guidelines recommend annual comprehensive dilated eye exams for all people with diabetes.
Mild, Moderate, and Severe Stages
PDR is considered the advanced stage of diabetic retinopathy and follows mild and moderate nonproliferative forms. Here’s how progression is often described:
| Stage | Main Features | Symptoms |
|---|---|---|
| Mild NPDR | Microaneurysms, small areas of swelling/leakage | Often none |
| Moderate NPDR | Increased bleeding, fluid leakage; possible macular edema | Blurring, floaters |
| Severe NPDR | Many blocked vessels, severe bleeding and swelling | Significant blurring or vision loss |
| Proliferative DR (PDR) | Abnormal new vessel growth, possible retinal detachment | Floaters, spots, severe vision loss |
Is Proliferative Diabetic Retinopathy Curable?
PDR is not curable in the sense of reversing all retinal damage or restoring lost vision. However, with prompt and effective treatment, further progression can be slowed or stopped, stabilizing the condition and often preserving remaining sight.
Crucially, control of underlying diabetes—especially blood sugar, blood pressure, and cholesterol—is vital for better outcomes.
Treatment Options for Proliferative Diabetic Retinopathy
Several medical and surgical approaches are available. Your eye care specialist will recommend options based on the extent and location of injury.
- Laser therapy (panretinal photocoagulation): The standard treatment for PDR. Laser light cauterizes abnormal vessels, reducing further growth and risk of bleeding.
- Anti-VEGF injections: Medications injected directly into the eye block vascular endothelial growth factor (VEGF), a signal that drives abnormal blood vessel formation. Examples include ranibizumab, aflibercept, and bevacizumab.
- Vitrectomy surgery: Used when there is significant bleeding or retinal detachment. The procedure removes blood and scar tissue from the vitreous and can help reattach the retina.
- Lifestyle management: Tight blood sugar control, management of blood pressure and cholesterol, and smoking cessation all slow the progression of retinopathy.
Early treatment matters: Treatments are much more effective when PDR is found early, before extensive retinal damage or detachment occurs.
Prevention and Vision Protection
While not all diabetic eye disease is preventable, the following steps substantially reduce risk:
- Monitor and control blood sugar (HbA1c) consistently
- Maintain healthy blood pressure and cholesterol
- Schedule regular annual dilated eye exams—even if asymptomatic
- Follow your diabetes care plan, including medications and lifestyle modifications
- Avoid smoking and manage other chronic health risks
- Report any new vision changes or symptoms promptly
Key fact: Vision loss from PDR can be prevented or minimized for most people who receive timely, appropriate treatment alongside good diabetes management.
Frequently Asked Questions About Proliferative Diabetic Retinopathy
Q1: Who typically develops proliferative diabetic retinopathy?
PDR develops in people who have had diabetes for many years, especially those with poor blood sugar control. Younger people with type 1 diabetes, long-term type 2 diabetes patients, and those with related complications like kidney damage or neuropathy are at higher risk.
Q2: How is proliferative diabetic retinopathy detected?
It’s diagnosed by an ophthalmologist during a dilated eye exam, which may be supplemented by retinal imaging tests such as OCT or fluorescein angiography to evaluate blood vessel growth and areas of leakage.
Q3: Can proliferative diabetic retinopathy be reversed?
Vision already lost due to extensive retinal damage or detachment may not be restored. However, progression of PDR can be slowed and further sight preserved through laser therapy, injection treatments, and careful diabetes management.
Q4: What are the warning signs I should never ignore?
- Sudden appearance of floaters or flashes
- Painless, rapid loss of vision
- Dark or empty spots in the field of vision
If you notice any of these, contact your eye care provider immediately.
Q5: What can I do to protect my vision if I have diabetes?
- Get annual eye exams—even without symptoms
- Keep your blood sugar, blood pressure, and cholesterol under control
- Follow your treatment plan and communicate any changes to your symptoms
Key Takeaways
- Proliferative diabetic retinopathy is a sight-threatening complication of diabetes that requires prompt attention
- Early detection: Regular eye exams make a difference in preventing irreversible vision loss
- Treatment: Laser therapy and anti-VEGF injections are standard, often combined with advanced surgery for severe cases
- Lifestyle: Blood sugar, blood pressure, and cholesterol control are critical for prevention and management
- Awareness: Know the warning signs and seek prompt care for new visual changes
References & Further Reading
- Mayo Clinic: Causes and symptoms of diabetic retinopathy
- UChicago Medicine: Overview and management of diabetic retinopathy
- Bay Area Retina Associates: Insights into PDR and patient risk factors
- Healthline: Comprehensive details on proliferative diabetic retinopathy, symptoms, and modern treatment options
References
- https://www.mayoclinic.org/diseases-conditions/diabetic-retinopathy/symptoms-causes/syc-20371611
- https://www.uchicagomedicine.org/conditions-services/ophthalmology/diabetic-retinopathy
- https://www.healthline.com/health/diabetes/proliferative-diabetic-retinopathy
- https://www.bayarearetina.com/proliferative-diabetic-retinopathy
- https://www.merckmanuals.com/professional/eye-disorders/retinal-disorders/diabetic-retinopathy
- https://my.clevelandclinic.org/health/diseases/8591-diabetic-retinopathy
- https://www.nhs.uk/conditions/diabetic-retinopathy/
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/diabetic-retinopathy
Read full bio of medha deb












