Understanding the Progression of Diabetic Macular Edema
Explore symptoms, risks, and treatment options for diabetic macular edema and learn how to slow or prevent vision loss.
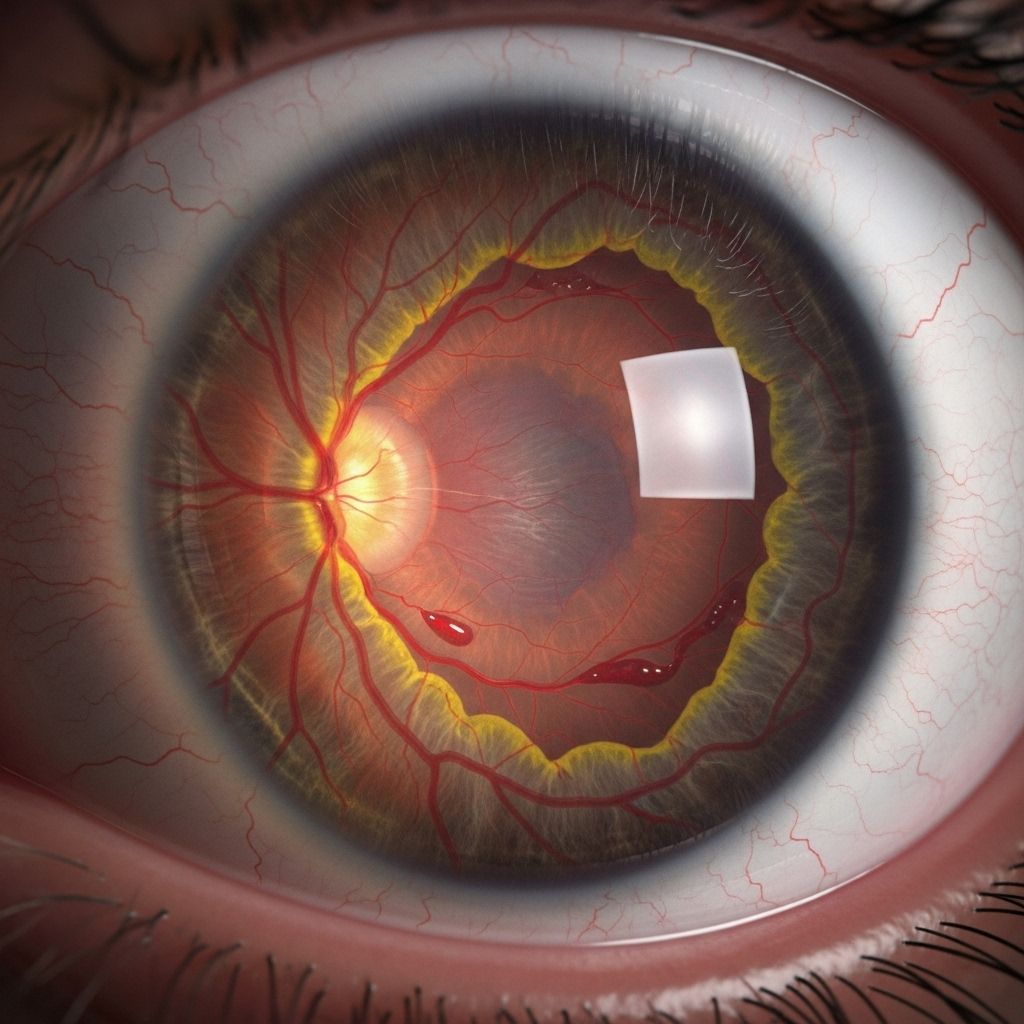
Diabetic macular edema (DME) is a common and potentially sight-threatening complication of diabetes. When blood sugar remains consistently high, it can cause damage to the tiny blood vessels of the eye, leading to swelling in the macula—a part of the retina essential for sharp, central vision. Recognizing how DME develops, progresses, and is managed can help people with diabetes preserve their eyesight.
What Is Diabetic Macular Edema?
Diabetic macular edema (DME) occurs when blood vessels in the retina leak fluid into the macula, leading to swelling and impaired vision. The macula is crucial for reading, driving, and seeing fine details. DME can develop at any stage of diabetic retinopathy, which is the broader term for diabetes-related retinal disease.
- Type 1 and type 2 diabetes both increase the risk of DME.
- DME is a leading cause of vision loss in people with diabetes.
- Maintaining optimal blood sugar control is key to preventing or slowing progression.
How Does Diabetic Macular Edema Progress?
The progression of DME is closely linked to the stages of diabetic retinopathy, the underlying retinal disease caused by diabetes. The condition usually advances slowly but can deteriorate more rapidly if left unmanaged.
Stages of Diabetic Retinopathy (and DME Risk)
| Stage | Description | Risk/Symptoms |
|---|---|---|
| Mild Nonproliferative Retinopathy | Early stage with small bulges (microaneurysms) in retinal blood vessels. | No symptoms or subtle vision changes. DME risk begins here. |
| Moderate Nonproliferative Retinopathy | More microaneurysms, swelling, and small hemorrhages; progression of retinal damage. | Blurry vision, trouble focusing, colors appear faded, increased DME risk. |
| Severe Nonproliferative Retinopathy | Blocked blood vessels cause further ischemia and swelling; large areas of retina affected. | Possible floaters, darker spots, vision loss, DME diagnosed or worsening. |
| Proliferative Retinopathy | Retina develops new, fragile blood vessels; high risk of severe bleeding and scar formation. | Severe vision loss, risk of blindness; DME often advanced. |
Symptoms and Signs of Diabetic Macular Edema
DME may cause mild symptoms in its early stages but can rapidly progress to significant visual impairment. Recognizing the signs early can facilitate timely treatment.
- Blurry or distorted central vision
- Colors may appear faded or washed out
- Difficulty reading or recognizing faces
- Dark or empty spots appearing in the center of vision
- Frequent changes in glasses prescription
It is important to note that DME can develop without noticeable symptoms, especially in the early phases. This underscores the importance of regular eye examinations for individuals with diabetes.
Who Is at Risk of Developing DME?
Anyone with diabetes can develop DME, but certain factors increase risk and the pace of progression:
- Long duration of diabetes (the longer you have diabetes, the higher the risk)
- Poor blood sugar control
- High blood pressure
- High cholesterol levels
- Kidney disease
- Poor management of diabetes-related health concerns
Additional risk factors include pregnancy and a family history of diabetic eye disease.
How Is Diabetic Macular Edema Diagnosed?
DME can only be definitively diagnosed by an eye specialist using specific examination techniques. Early detection is crucial for preventing irreversible vision loss.
- Dilated eye exam: Eye drops enlarge the pupil to allow a comprehensive view of the retina. The doctor inspects for swelling, leaking blood vessels, and changes in the macula.
- Optical coherence tomography (OCT): A painless imaging test that provides a cross-sectional view of the retina and quantifies macular swelling or edema.
- Fluorescein angiography: A special dye is injected into the bloodstream to highlight leaking or abnormal blood vessels in the retina.
- Visual acuity tests: Assess how well you can see letters and details at various distances, tracking any changes over time.
Routine screenings—even in the absence of symptoms—are essential for all people with diabetes.
Potential Complications of Untreated DME
If diabetic macular edema is not treated promptly, it can result in several serious complications, including:
- Permanent vision loss or even blindness
- Development of proliferative diabetic retinopathy (new, abnormal blood vessel growth)
- Formation of scar tissue, which can detach the retina
- Increased risk of secondary conditions like glaucoma
How Quickly Does DME Progress?
The rate at which DME progresses varies widely. Key factors include the duration of diabetes, degree of blood sugar control, and how early the disease is detected and managed. In some individuals, DME develops slowly over years; in others, it can worsen more rapidly, especially if underlying diabetes is poorly controlled or if retinopathy is already at an advanced stage.
Progression may be faster with:
- Uncontrolled blood sugar levels
- Coexisting high blood pressure or kidney problems
- Advanced stages of diabetic retinopathy
Regular checkups can help detect changes early and slow disease advancement.
Managing and Treating Diabetic Macular Edema
Effective management of DME focuses on both treating the underlying diabetes and directly addressing eye swelling. Treatment plans are tailored to the severity of the condition and the patient’s overall health profile.
Medical Treatments for DME
- Anti-VEGF injections: Medications injected into the eye that block vascular endothelial growth factor (VEGF), reducing abnormal vessel leakage and swelling. Commonly used drugs include ranibizumab, aflibercept, and bevacizumab.
- Steroid injections or implants: These reduce inflammation and swelling in the macula. They may be considered if anti-VEGF medications are not effective or appropriate.
- Laser therapy: Focal or grid laser treatment seals leaking blood vessels and can stabilize vision, though it is less commonly used as an initial therapy than before the introduction of anti-VEGF drugs.
Controlling Underlying Health Issues
- Tight blood glucose control: Monitoring and regulating blood sugar levels can slow the progression of both DME and diabetic retinopathy.
- Managing hypertension and cholesterol: High blood pressure and elevated lipid levels increase the risk for DME. Medications or lifestyle modifications may be required.
- Kidney health: Addressing kidney problems helps decrease DME risk and progression.
Lifestyle Approaches
- Stop smoking
- Maintain a healthy weight
- Exercise regularly (as medically advised)
- Follow a diabetes-appropriate diet
Can DME Be Prevented?
While DME cannot always be completely prevented, the risk can be substantially reduced through effective diabetes management and routine eye care. Key prevention strategies include:
- Staying within your individualized blood sugar targets
- Controlling blood pressure and cholesterol
- Attending annual or more frequent eye exams
- Reporting changes in vision to your healthcare provider promptly
Frequently Asked Questions About Diabetic Macular Edema
Q: Is diabetic macular edema common?
A: Yes, DME is a leading cause of vision loss among people with diabetes. The risk increases the longer a person has diabetes and the less controlled their blood sugar levels are.
Q: Can DME lead to blindness?
A: If left untreated, DME can cause permanent vision loss and even total blindness. However, treatments are effective at slowing or stopping progression if started early.
Q: Does DME always cause symptoms at the start?
A: No, DME can develop without any noticeable symptoms in its earliest stages. Regular eye exams are essential for early detection, even if your vision seems unchanged.
Q: How often should I have my eyes checked if I have diabetes?
A: Most adults with diabetes should have a comprehensive, dilated eye exam at least once a year. More frequent visits may be necessary if DME or diabetic retinopathy has already developed.
Q: Can good diabetes management prevent DME from getting worse?
A: Yes, keeping blood sugar, blood pressure, and cholesterol at healthy levels is crucial for slowing the progression of DME and reducing the risk of severe vision problems.
When to Seek Immediate Medical Attention
If you have diabetes and experience sudden vision changes, severe blurring, a dark curtain over your field of view, or eye pain, seek emergency eye care. Early intervention is the best defense against irreversible vision loss.
Key Takeaways
- Diabetic macular edema is a major cause of diabetes-related vision loss.
- It can develop at any stage of diabetic retinopathy, with risk increasing alongside poor blood sugar control and longer diabetes duration.
- Early detection, medical management, and lifestyle changes can preserve vision and quality of life.
- Annual eye exams are essential for people with diabetes.
To protect your eyesight, work with your healthcare team to keep diabetes well-managed and never skip recommended eye appointments.
References
- https://resources.healthgrades.com/right-care/diabetes/understanding-the-four-stages-of-diabetic-retinopathy
- https://www.riverside-eye-center-maine.com/diabetic-retinopathy-stages-norway/
- https://newjerseyvision.com/diabetic-retinopathy-stages-nj/
- https://modernod.com/articles/2019-june/the-four-stages-of-diabeticretinopathy
- https://www.healthline.com/health/diabetes/progression-diabetic-macular-edema
- https://www.webmd.com/diabetes/diabetic-macular-edema-progression
- https://eyewiki.org/Diabetic_Macular_Edema
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9655436/
- https://my.clevelandclinic.org/health/diseases/24733-diabetes-related-macular-edema
Read full bio of medha deb












