Primary Open-Angle Glaucoma: Causes, Symptoms, Diagnosis, and Treatment
Learn about primary open-angle glaucoma, its causes, symptoms, diagnosis, treatment options, and strategies for prevention.
What to Know About Primary Open-Angle Glaucoma
Primary open-angle glaucoma (POAG) is the most prevalent form of glaucoma worldwide, responsible for the majority of cases that result in gradual vision loss and potential blindness if left untreated. Glaucoma impacts approximately 70 million people globally, with POAG accounting for around 80% of glaucoma cases in the United States. Understanding this condition is key to preserving eye health and sight.
Quick Facts about POAG
- Second-leading cause of blindness worldwide
- Progressive and often asymptomatic in early stages
- Most common type of glaucoma
- Can cause permanent vision loss if untreated
- Detections rely on regular eye exams
Understanding Glaucoma: A Brief Overview
Glaucoma refers to a group of eye diseases that damage the optic nerve—typically due to increased intraocular pressure (IOP)—which can result in vision impairment. There are several forms of glaucoma, but two main categories are recognized:
- Open-angle glaucoma: Includes primary and secondary forms; the drainage angle remains open.
- Closed-angle glaucoma: The drainage angle is blocked or narrowed, requiring urgent treatment.
What Is Primary Open-Angle Glaucoma?
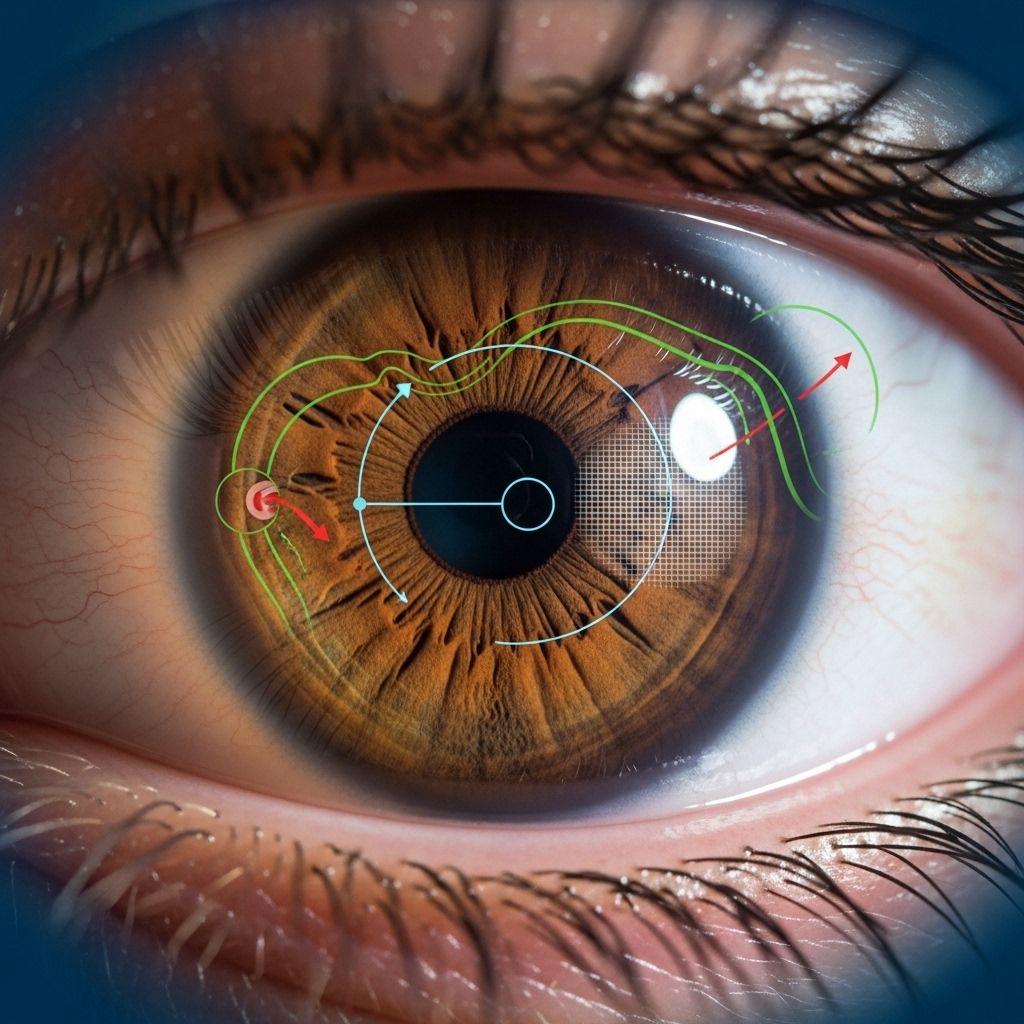
Primary open-angle glaucoma is a chronic eye disease (“primary” meaning no underlying cause) where the eye’s drainage angle stays open, but the normal outflow of fluid (aqueous humor) is gradually reduced due to subtle blockages in the optic drainage system. This leads to a slow increase in eye pressure, which damages the optic nerve over time.
How Does POAG Affect the Eye?
- The trabecular meshwork, a spongy tissue near the cornea and iris, facilitates fluid drainage from the eye.
- In POAG, this meshwork is less effective, causing fluid buildup and increased IOP.
- Chronic high IOP gradually impairs the optic nerve, leading to progressive vision loss.
POAG often occurs slowly, and most people do not notice symptoms until damage has advanced.
Primary vs. Secondary Glaucoma
| Type | Definition | Common Causes |
|---|---|---|
| Primary Open-Angle Glaucoma | Develops on its own, no obvious external cause | Unknown (idiopathic) |
| Secondary Open-Angle Glaucoma | Develops due to another eye condition or injury | Cataracts, inflammation, trauma, steroids |
Most cases of glaucoma are primary open-angle glaucoma. Secondary open-angle glaucoma results from factors such as eye injury, underlying eye diseases, or drug side effects.
Causes and Risk Factors
There’s no single identifiable cause for POAG, yet several factors can increase individual risk:
- Age: Higher risk after age 40
- Family history: Genetic predisposition, notably mutations in the MYOC gene
- Ethnicity: African, Afro-Caribbean, and Latino populations have increased risk
- Medical conditions: High blood pressure, diabetes, and myopia (nearsightedness)
- Other factors: Thin corneas and prolonged steroid medications usage
Most glaucomas are thought to result from a combination of genetic and environmental factors. POAG may occasionally be associated with mutations in the MYOC gene, which can affect eye pressure regulation.
Open-Angle vs. Closed-Angle (Angle-Closure) Glaucoma
| Feature | Open-Angle | Closed-Angle |
|---|---|---|
| Drainage Angle | Open and normal | Narrowed or blocked |
| Onset | Progressive, slow | Sudden or gradual, sometimes emergency |
| Symptoms | Often silent until advanced | Pain, nausea, blurred vision, halos |
| Treatment urgency | Regular follow-up | Emergency if acute |
POAG is usually silent and slowly progressive. In contrast, closed-angle glaucoma can cause an abrupt increase in eye pressure, with acute symptoms requiring immediate medical attention.
Symptoms of Primary Open-Angle Glaucoma
Early stages: Most people with POAG experience no symptoms. The disease is sometimes called the “silent thief of sight.”
- No pain or discomfort
- No noticeable changes in vision at first
Advanced stages: As POAG progresses, symptoms begin to develop:
- Gradual loss of peripheral vision (side vision)
- Narrowed field of vision
- Blurred vision in one or both eyes
- Eventually, central vision may be affected
- If untreated, irreversible blindness
How Is POAG Diagnosed?
Regular eye screenings are essential for early detection. Ophthalmologists and optometrists use several diagnostic tests:
- Tonometry: Measures intraocular pressure after numbing the eye with drops.
- Ophthalmoscopy: Eye drops dilate the pupil to allow examination of the optic nerve for signs of damage.
- Visual field test: Assesses peripheral vision loss via a flashing lights test.
- Pachymetry: Measures corneal thickness, which can affect pressure readings.
- Gonioscopy: Uses a contact lens to determine if the drainage angle is open or closed.
Treatment of Primary Open-Angle Glaucoma
POAG cannot be cured, and lost vision cannot be restored. However, available treatments can slow the progression and help prevent further vision loss:
- Medications: Eye drops remain the first-line therapy to lower intraocular pressure. Various drug classes include prostaglandin analogs, beta blockers, alpha agonists, and carbonic anhydrase inhibitors.
- Oral medications: Sometimes prescribed if drops are insufficient.
- Laser therapy: Laser trabeculoplasty improves drainage through the trabecular meshwork.
- Surgical procedures: In severe cases, surgery may be necessary (e.g., trabeculectomy, glaucoma drainage devices).
Most people manage POAG with lifelong therapy and regular follow-up; early detection leads to better outcomes.
Goals of Treatment
- Lower intraocular pressure
- Prevent further optic nerve damage
- Preserve remaining vision
Can POAG Be Prevented?
There’s no guaranteed way to prevent POAG, but steps can help lower individual risk and aid early detection:
- Schedule regular eye exams (especially over age 40 or with risk factors)
- Know your family history; inform your eye care provider
- Control systemic conditions like blood pressure and diabetes
- Use medications only as prescribed
Early detection and proactive management are key to preventing irreversible vision loss.
Summary: Key Takeaways
- Primary open-angle glaucoma is a chronic, progressive eye disease often without early symptoms.
- It gradually impairs peripheral vision and, if untreated, can cause blindness.
- Treatment can slow progression but cannot reverse vision loss.
- Regular comprehensive eye exams are critical for early detection.
- Certain populations are at higher risk—ethnic background, age, family history, and systemic health play vital roles.
Frequently Asked Questions (FAQ)
Can I tell if I have glaucoma before I lose vision?
No. Primary open-angle glaucoma rarely causes noticeable symptoms before vision loss occurs, making regular eye exams essential.
Who is at greatest risk for POAG?
People over age 40, those with a family history of glaucoma, African and Latino descent, and those with conditions like diabetes or high blood pressure carry greater risk.
Is vision loss from POAG reversible?
No. Any sight lost from glaucoma is permanent, which is why early detection and treatment are so vital.
How often should I get my eyes checked?
If you have risk factors, annual comprehensive eye exams are recommended. Others can discuss frequency with their provider.
What is the prognosis if POAG is detected early?
With timely diagnosis and treatment, most people can maintain useful vision throughout life.
SEO Table: Summary of POAG Differences
| Aspect | Primary Open-Angle Glaucoma | Angle-Closure Glaucoma |
|---|---|---|
| Frequency | Most common (80-90%) | Less common |
| Symptoms | No early symptoms | Pain, blurred vision, nausea |
| Progression | Slow, chronic | Rapid, acute or gradual |
| Urgency | Managed with regular care | Often requires emergency treatment |
Bottom Line
Primary open-angle glaucoma is a leading cause of irreversible blindness globally. Since the condition progresses silently, regular eye screenings and awareness of risk factors are the most powerful tools for preserving sight. If diagnosed, diligent management with medications, procedures, and ongoing care can prevent further vision loss and maintain quality of life.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3700399/
- https://www.healthline.com/health/eye-health/primary-open-angle-glaucoma
- https://www.allaboutvision.com/conditions/glaucoma/primary-open-angle/
- https://glaucoma.org/types/open-angle-glaucoma
- https://www.healthline.com/health/glaucoma
- https://www.medicalnewstoday.com/articles/open-vs-closed-angle-glaucoma
- https://www.healthlinejournal.org/ojs/healthline/article/view/H565
- https://eyewiki.org/Primary_Open-Angle_Glaucoma
- https://www.brightfocus.org/resource/primary-open-angle-glaucoma/
- https://glaucoma.org/types
Read full bio of Sneha Tete












