Primary Membranous Nephropathy: Symptoms, Causes, Diagnosis, and Treatment
Primary membranous nephropathy is a rare autoimmune disease affecting kidney filters, causing nephrotic syndrome and chronic complications.
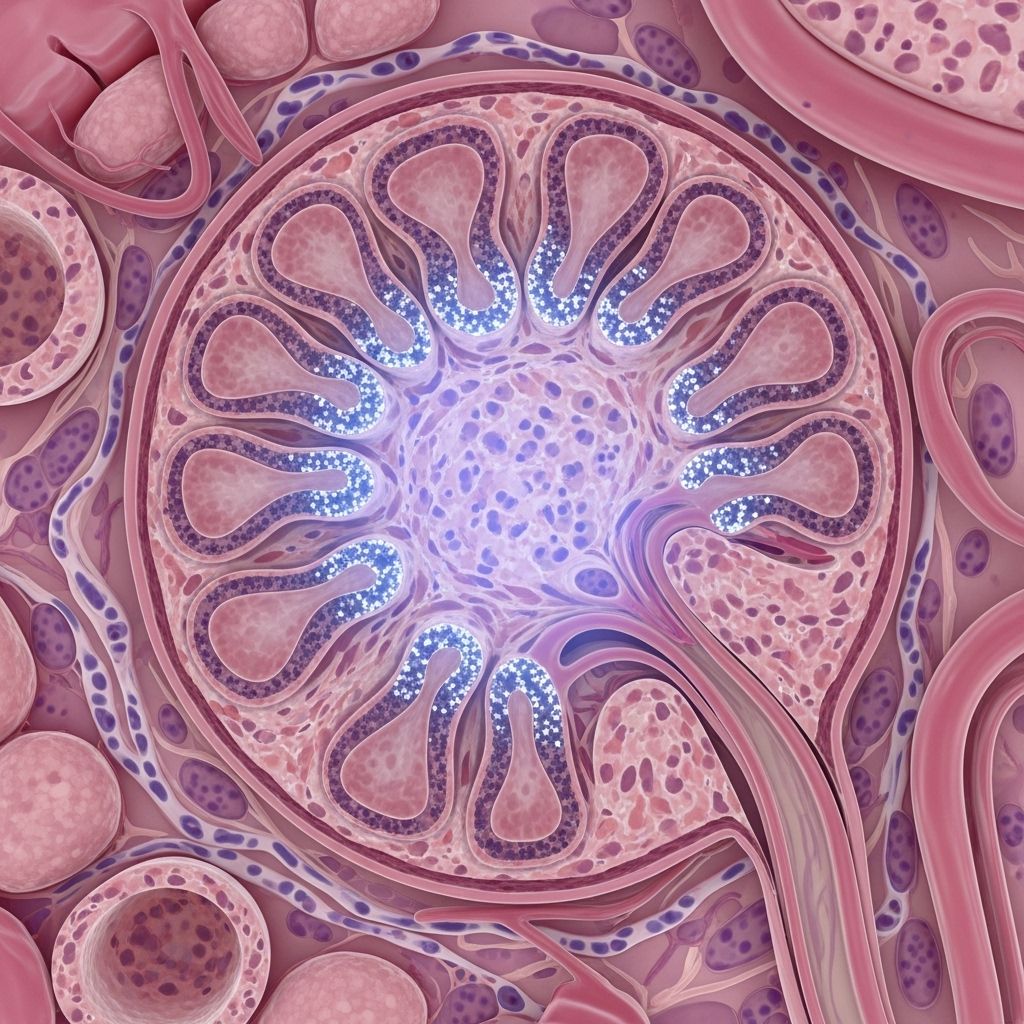
What Is Primary Membranous Nephropathy?
Primary membranous nephropathy (PMN) is a rare, chronic autoimmune kidney disease. In PMN, the immune system mistakenly attacks the glomeruli—the tiny filtering units in the kidneys that remove waste from the blood—leading to progressive kidney damage. PMN accounts for roughly 75-80% of all cases of membranous nephropathy, with the remainder classified as secondary membranous nephropathy when caused by another underlying condition.
Nephrotic syndrome, a collection of symptoms signified by high levels of protein in urine, swelling (edema), and altered blood chemistry, is the most common outcome of PMN.
Understanding Kidney Filters: The Role of the Glomeruli
The glomeruli are microscopic filters located inside the kidneys, responsible for filtering waste, toxins, and excess fluids from the blood. PMN damages these filters, making them leaky and inefficient, resulting in a variety of downstream symptoms.
- Glomerular injury leads to proteinuria (excess protein in urine).
- Loss of protein in blood causes fluid retention and swelling.
- Dysfunction contributes to high blood pressure and changes in kidney function over time.
Types of Membranous Nephropathy
| Type | Description | Prevalence |
|---|---|---|
| Primary Membranous Nephropathy (PMN) | Autoimmune, with no secondary cause; body forms antibodies against kidney filters. | 75–80% |
| Secondary Membranous Nephropathy | Result of another disease, infection, drug, or toxin affecting kidneys. | 20–25% |
Causes of Primary Membranous Nephropathy
PMN is an autoimmune disease—the immune system attacks healthy kidney tissue by mistake.
The most common molecular targets implicated in PMN include:
- Phospholipase A2 receptor (PLA2R) antibodies (70–80% of primary cases)
- Neural epidermal growth factor-like 1 (NELL)
- Thrombospondin type-1 domain-containing 7A (THSD7A)
In PMN, autoantibodies bind to the glomerular membrane and activate the immune response, causing inflammation, thickening of the basement membrane, and leakage of proteins into the urine.
For secondary membranous nephropathy, triggers can include:
- Chronic infections (e.g., hepatitis B/C, HIV, syphilis, malaria)
- Autoimmune diseases (e.g., lupus, rheumatoid arthritis, Sjogren’s syndrome)
- Certain drugs (NSAIDs, penicillamine, gold, anti-TNF agents, probenecid)
- Heavy metals (e.g., mercury)
- Malignancies (primarily cancers of the lung, gastrointestinal tract, or hematological disorders)
- Miscellaneous: transplants, diabetes
Signs and Symptoms of Primary Membranous Nephropathy
Early stages of PMN may be asymptomatic, but signs often emerge as kidney damage progresses. The most common and earliest symptom is swelling (edema)—usually noticed first in the feet, ankles, and legs, and may later extend to the face, abdomen, and other areas. Additional symptoms include:
- Foamy/frothy urine: due to high protein content
- Increased urination (polyuria)
- High blood pressure (hypertension)
- High cholesterol levels
- Unintended weight gain (often from fluid retention)
- Fatigue and reduced energy
- Trouble breathing or shortness of breath (when fluid accumulates in lungs)
- Poor appetite
If left untreated, symptoms may worsen and eventually progress to chronic kidney disease or, in rare cases, kidney failure.
Who Gets Primary Membranous Nephropathy?
- PMN is rare, affecting approximately 1 out of every 5,000 people.
- Occurs most frequently in white men over age 40, with a peak between ages 50 and 60.
- In women, children, or other ethnic groups, PMN is less common and often secondary to another health condition (such as lupus).
Diagnosing Primary Membranous Nephropathy
Diagnosing PMN requires a combination of clinical assessments and laboratory tests. Initial evaluation is typically conducted by a nephrologist and includes:
- Urine tests: To measure protein loss, such as the urine albumin-to-creatinine ratio (uACR)
- Blood tests: To assess kidney function, including estimating glomerular filtration rate (eGFR) and measuring creatinine levels
If kidney damage or nephrotic syndrome is confirmed, further tests are conducted to identify the cause:
- Serum antibody tests – Detecting antibodies for PLA2R, THSD7A, and/or NELL
- Kidney biopsy – Examines kidney tissue for immune deposits and confirms PMN diagnosis. Can also be used when antibody tests are inconclusive.
If both nephrotic syndrome and a positive PLA2R or THSD7A antibody result are found, a kidney biopsy may not be required for diagnosis. However, if tests are negative, a biopsy is the gold standard for diagnosis.
Treatment Options for Primary Membranous Nephropathy
The goals of PMN treatment are to induce remission, slow disease progression, and manage symptoms. There are two main approaches:
- Lifestyle changes
- Medications
Lifestyle Changes for PMN Management
- Sodium restriction: Reduces fluid retention and controls blood pressure.
- Protein management: Individualized, as excessive protein intake may stress kidneys.
- Low cholesterol/fat diet: Helps manage lipid levels due to high cholesterol risk.
- Smoking cessation: Decreases risk of further kidney damage.
- Regular exercise: Promotes overall health and cardiovascular stability.
Medications for Primary Membranous Nephropathy
- Immunosuppressants: Reduce immune system activity and autoantibody production.
- Steroids: Control inflammation and immune response; often used with other immunosuppressants.
- Blood pressure medications: ACE inhibitors or ARBs help protect kidneys and lower blood pressure.
- Statins: Used to control cholesterol and reduce cardiovascular risks.
- Diuretics: Help reduce swelling and manage fluid retention.
- Anticoagulants: May be considered due to increased risk of blood clots (thromboembolic complications).
Potential Complications
- Chronic kidney disease: Gradual loss of kidney function over time.
- Kidney failure: Rare, but possible in severe or untreated PMN; may require dialysis or transplant.
- Thromboembolic events: Increased risk for blood clots, especially in veins.
- Higher cardiovascular risk: Due to chronic hypertension and dyslipidemia.
- Infections: Loss of immune-focused proteins may reduce resistance to some bacterial infections.
Prognosis and Living With Primary Membranous Nephropathy
PMN is a chronic disease that can be managed successfully with early detection and appropriate treatment. Outcomes vary:
- Roughly one-third of people achieve complete remission with treatment.
- Another third achieve partial remission but may require ongoing management of symptoms.
- The remainder may see progressive decline in kidney function, requiring close monitoring and possible interventions like dialysis.
Quality of life depends heavily on controlling blood pressure, limiting proteinuria, and managing associated symptoms. Regular follow-up with kidney specialists, dietary changes, and medication adherence are crucial.
Preventive steps to avoid infections, maintain cardiovascular health, and support emotional wellness are important for long-term living with PMN.
Frequently Asked Questions (FAQs)
Q: What is the difference between primary and secondary membranous nephropathy?
A: Primary membranous nephropathy is an autoimmune disease with no identifiable secondary cause, while secondary membranous nephropathy results from another condition (infection, autoimmune disease, certain drugs, or toxins).
Q: Is primary membranous nephropathy curable?
A: PMN is not currently curable, but it can often be managed. Many people go into remission with treatment and lifestyle adjustments.
Q: Who is most likely to get primary membranous nephropathy?
A: PMN is most common in white men over forty, especially between fifty and sixty years old. Women and children are more likely to have secondary forms, often related to another disease.
Q: What does “nephrotic syndrome” mean?
A: Nephrotic syndrome refers to a group of symptoms caused by kidney filter leakage: high urine protein, swelling, high cholesterol, and low blood albumin.
Q: Will I need dialysis if I have PMN?
A: Most patients with PMN do not need dialysis, especially if treated early. Severe or progressive cases may eventually need dialysis or a transplant.
Q: How often should someone with PMN see their doctor?
A: Frequent follow-up is recommended—typically every few months—until remission is achieved, then less frequently for ongoing monitoring.
Resources and Support
- National Kidney Foundation resources for patients and families
- Local nephrology care teams and patient support groups
- Dieticians for managing kidney-friendly diets
- Mental health services for coping with chronic illness
Summary Table: Key Facts on Primary Membranous Nephropathy
| Feature | Primary Membranous Nephropathy |
|---|---|
| Status | Chronic autoimmune kidney disease |
| Main Symptom | Swelling (edema) and proteinuria |
| Diagnosis | Antibody tests (PLA2R, THSD7A, NELL), kidney biopsy |
| Treatment | Lifestyle + medications (immunosuppressants, BP meds, statins, diuretics) |
| Prognosis | Varies: complete or partial remission possible, chronic monitoring needed |
References
- https://www.kidneyfund.org/all-about-kidneys/other-kidney-diseases/pmn
- https://www.webmd.com/a-to-z-guides/what-is-membranous-nephropathy
- https://www.ncbi.nlm.nih.gov/books/NBK559169/
- https://unckidneycenter.org/kidneyhealthlibrary/glomerular-disease/membranous-nephropathy/
- https://my.clevelandclinic.org/health/diseases/21154-membranous-nephropathy
- https://www.mountsinai.org/health-library/diseases-conditions/membranous-nephropathy
- https://www.reboot-study.org/about-primary-membranous-nephropathy
- https://www.rarediseasesnetwork.org/diseases/121/membranous-nephropathy
- https://arupconsult.com/content/primary-membranous-nephropathy-idiopathic-membranous-glomerulonephritis
Read full bio of Sneha Tete












