Precursor B-Cell Acute Lymphoblastic Leukemia (Pre-B-ALL): Symptoms, Causes, and Treatment
Explore symptoms, risks, complications, and treatment of precursor B-cell acute lymphoblastic leukemia in children and adults.
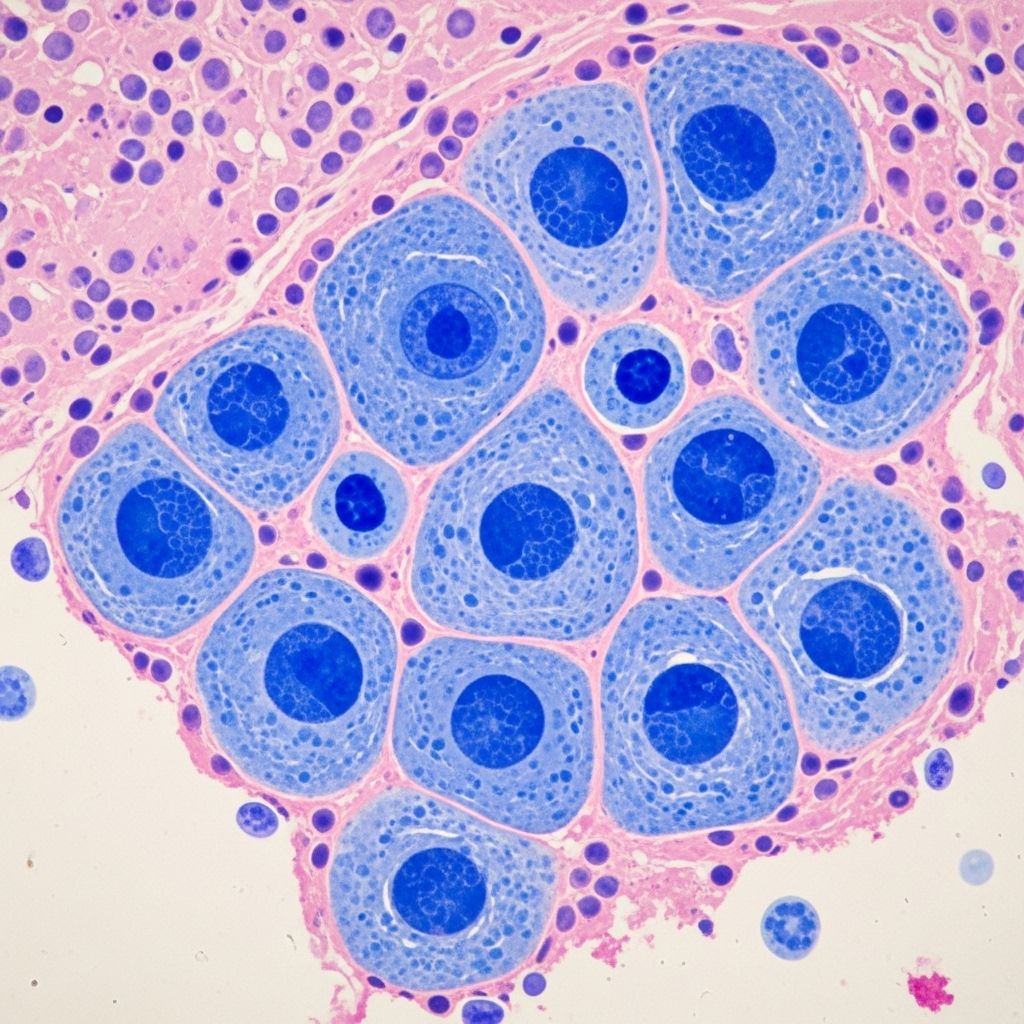
Precursor B-cell acute lymphoblastic leukemia (Pre-B-ALL) is a fast-growing cancer of the blood and bone marrow that affects immature B cells, a type of white blood cell vital to the immune system. Most often seen in children but also found in adults, Pre-B-ALL requires prompt diagnosis and treatment to improve patient outcomes.
What Is Precursor B-Cell Acute Lymphoblastic Leukemia?
Pre-B-ALL is a subtype of acute lymphoblastic leukemia (ALL), a cancer characterized by the overproduction and accumulation of immature lymphocytes (lymphoblasts). In Pre-B-ALL, these abnormal cells originate from early B-cell precursors in the bone marrow. The condition progresses rapidly, crowding out healthy blood cells and leading to various symptoms due to the impaired function of blood and immune systems.
ALL is the most common type of childhood leukemia, and Pre-B-ALL makes up more than 80% of ALL diagnoses in children. However, Pre-B-ALL can occur at any age, and the disease tends to be more aggressive in adults.
Causes and Risk Factors of Pre-B-ALL
Pre-B-ALL arises due to genetic mutations in immature B cells, which prevent their maturation and prompt them to grow uncontrollably. While the exact cause often remains unclear, several risk factors have been identified:
- Age: Higher incidence in children, especially ages 2–5, and in adults over 50.
- Sex: More frequent in males than females.
- Genetic conditions: Increased risk with inherited disorders such as Down syndrome, Fanconi anemia, and Li-Fraumeni syndrome.
- Environmental exposures: Prior exposure to high levels of radiation, previous chemotherapy, or chemicals like benzene raises the risk.
- Family history: Having a close relative with leukemia may slightly increase risk.
Mutations in genes that control cell growth, development, and division are central to the transformation of normal precursor B cells into leukemic cells.
Symptoms of Pre-B-ALL
The symptoms of Pre-B-ALL mainly result from the replacement of normal bloodforming cells in the bone marrow with leukemia cells. The decline in healthy red blood cells, white blood cells, and platelets leads to a range of symptoms:
Due to Low Red Blood Cells (Anemia):
- Fatigue and weakness
- Shortness of breath
- Dizziness or lightheadedness
- Pale skin
Due to Low White Blood Cells (Leukopenia):
- Frequent infections
- Recurring fevers
- Slow healing of wounds
Due to Low Platelets (Thrombocytopenia):
- Easy bruising
- Frequent or severe nosebleeds
- Bleeding gums
- Heavier or prolonged menstrual periods
Other Common Symptoms:
- Reduced appetite and unintentional weight loss
- Night sweats
- Swollen lymph nodes (often in the neck, underarm, or groin)
- Enlargement of the spleen or liver, causing abdominal discomfort
- Chest pain (especially if lymphoblasts collect in the chest area)
- Bone or joint pain (from marrow expansion by leukemia cells)
- Generalized aches or feeling of malaise
These symptoms typically appear rapidly, developing within days or weeks before diagnosis. In rare cases, Pre-B-ALL may be discovered during routine bloodwork in seemingly healthy individuals.
Potential Complications of Pre-B-ALL
Without prompt treatment, Pre-B-ALL can cause several serious complications:
- Severe infections: Weakened immunity makes even minor infections dangerous and in some cases life-threatening.
- Serious bleeding: Low platelets increase the risk of spontaneous and hard-to-control bleeds, including internally.
- Cancer spread (metastasis): Leukemia cells may migrate to the brain and spinal cord, causing neurological symptoms such as severe headaches, vision or balance problems, and seizures.
- Tumor lysis syndrome: A potentially life-threatening condition due to the rapid destruction of cancer cells during initial treatment, resulting in a sudden release of cell contents into the blood, affecting the kidneys and heart.
Signs and Symptoms of Tumor Lysis Syndrome
- Nausea and vomiting
- Muscle cramping
- Heart palpitations
- Numbness or tingling
- Seizures
Pre-B-ALL in Children
Although ALL can affect all ages, children—especially those between 2 and 5—are at the highest risk. Of all pediatric cancers, ALL accounts for about 30%, and of these, over 80% are Pre-B-ALL. The disease is less common but more aggressive in adults.
Children with Pre-B-ALL typically experience:
- Fatigue and paleness
- Unexplained fevers
- Bruising or bleeding easily
- Bone pain or joint discomfort
- Enlarged lymph nodes or abdominal swelling from organ involvement
Outcomes in children with Pre-B-ALL are generally more favorable. The improved outlook is attributed to differences in leukemia biology and children’s ability to tolerate intensive treatments.
Diagnosis of Pre-B-ALL
Confirmation of Pre-B-ALL diagnosis involves several specialized tests. A combination of these investigations helps establish the diagnosis, rule out other conditions, and guide treatment planning:
- Complete blood count (CBC): Often shows anemia, low platelets, and abnormal white blood cells.
- Peripheral blood smear: Examination under a microscope detects the abnormal lymphoblasts characteristic of ALL.
- Bone marrow aspiration and biopsy: Definitive test confirming the presence and type of leukemia cells in the bone marrow.
- Immunophenotyping/flow cytometry: Laboratory techniques that distinguish Pre-B-ALL from other leukemia types based on cell surface markers.
- Cytogenetic and molecular testing: Identifies genetic mutations or chromosomal abnormalities that may affect prognosis and therapy.
- Imaging: Chest X-rays, ultrasound, or CT scans detect organ enlargement or lymph node involvement.
- Lumbar puncture: Assesses possible spread to the central nervous system by analyzing cerebrospinal fluid.
Proper diagnosis is crucial, as Pre-B-ALL can resemble other blood cancers but requires different treatment.
Treatment Options for Pre-B-ALL
Treatment for Pre-B-ALL has advanced significantly, resulting in improved survival, especially in children. Therapy is typically tailored to each individual based on age, leukemia subtype, genetic findings, and overall health. The main components are:
Chemotherapy
This is the primary treatment, using a combination of drugs in different phases:
- Induction: An intensive initial phase aiming for complete remission by killing as many leukemia cells as possible.
- Consolidation (intensification): Additional chemotherapy to destroy remaining leukemia cells and prevent relapse.
- Maintenance: Lower-dose, long-term chemotherapy to maintain remission.
Targeted Therapy
Some cases of Pre-B-ALL involve specific genetic changes (such as the Philadelphia chromosome), which may be treated with targeted drugs that disrupt abnormal cell signaling.
Immunotherapy
- Monoclonal antibodies (e.g., blinatumomab, inotuzumab ozogamicin): These therapies target specific proteins on leukemia cells, directing the patient’s immune system to destroy them.
- CAR T-cell therapy: Involves engineering the patient’s own T cells to better target and kill leukemia cells; typically used for relapsed or resistant Pre-B-ALL.
Radiation Therapy
Although not routinely used, radiation may be recommended if leukemia has spread to the brain or spinal cord, or to shrink large tumors.
Stem Cell Transplant (Bone Marrow Transplant)
Used primarily for high-risk or relapsed cases, this procedure replaces diseased bone marrow with healthy stem cells, often from a matched donor.
Supportive Care
- Blood transfusions to address anemia or low platelets
- Antibiotics, antifungals, and antivirals to prevent or treat infections
- Pain control and management of side effects
- Close monitoring for complications such as tumor lysis syndrome
Prognosis and Outlook
Outcomes for Pre-B-ALL have improved considerably in recent decades, especially among children. Factors influencing prognosis include:
- Age at diagnosis (children fare better than adults)
- White blood cell count at presentation
- Response to initial therapy
- Genetic and molecular characteristics of leukemia cells
Five-year survival rates for children can exceed 85%, while for adults, the rate is lower but continues to improve with newer therapies. Early diagnosis and adherence to the treatment plan are vital to the best outcomes.
Living With Pre-B-ALL
A diagnosis of Pre-B-ALL brings emotional, physical, and logistical challenges. Patients, families, and caregivers can access support in a variety of ways:
- Pediatric and adult oncology teams guide treatment and provide holistic care.
- Support groups offer shared experiences, coping strategies, and encouragement.
- Nutritional, psychological, and social services help manage the effects of disease and treatment.
- Long-term follow-up is important for monitoring remission, managing late effects, and improving quality of life.
Frequently Asked Questions (FAQs)
What is the difference between Pre-B-ALL and other types of ALL?
Pre-B-ALL arises from immature B lymphocytes in the bone marrow, while other types, like T-cell ALL, originate from immature T cells. Pre-B-ALL is more common, especially in children.
Why do children have a better prognosis than adults with Pre-B-ALL?
Children typically tolerate chemotherapy better, and their Pre-B-ALL is often biologically more responsive to treatment, leading to higher remission and cure rates.
Is Pre-B-ALL hereditary?
Most Pre-B-ALL cases are not inherited. However, genetic syndromes like Down syndrome raise the risk, and a family history may slightly increase susceptibility.
What are the early warning signs of Pre-B-ALL?
Early signs include unexplained fatigue, frequent infections, easy bruising, recurring fever, swollen lymph nodes, or bleeding. Any persistent or concerning symptoms should be evaluated by a doctor.
How is Pre-B-ALL treated if it relapses?
Relapsed Pre-B-ALL may require more intensive chemotherapy, targeted therapies, immunotherapies, or stem cell transplantation. Newer approaches like CAR T-cell therapy offer hope for difficult cases.
References
- https://www.healthline.com/health/leukemia/pre-b-acute-lymphoblastic-leukemia
- https://www.cancer.org/cancer/types/acute-lymphocytic-leukemia/detection-diagnosis-staging/signs-symptoms.html
- https://www.leukaemia.org.au/blood-cancer/types-of-blood-cancer/leukaemia/acute-lymphoblastic-leukaemia/
- https://www.ncbi.nlm.nih.gov/books/NBK459149/
- https://www.cancer.gov/types/leukemia/patient/child-all-treatment-pdq
- https://www.mayoclinic.org/diseases-conditions/acute-lymphocytic-leukemia/symptoms-causes/syc-20369077
- https://my.clevelandclinic.org/health/diseases/21564-acute-lymphocytic-leukemia
- https://cancer.osu.edu/for-patients-and-caregivers/learn-about-cancers-and-treatments/cancers-conditions-and-treatment/cancer-types/blood-cancers/leukemia/b-cell-acute-lymphoblastic-leukemia
Read full bio of Sneha Tete












