Understanding Posterior Vitreous Detachment: Causes, Symptoms, and Care
Learn about posterior vitreous detachment, its symptoms, risks, and what to expect if you or a loved one experiences this common age-related eye change.
Posterior Vitreous Detachment (PVD): Overview
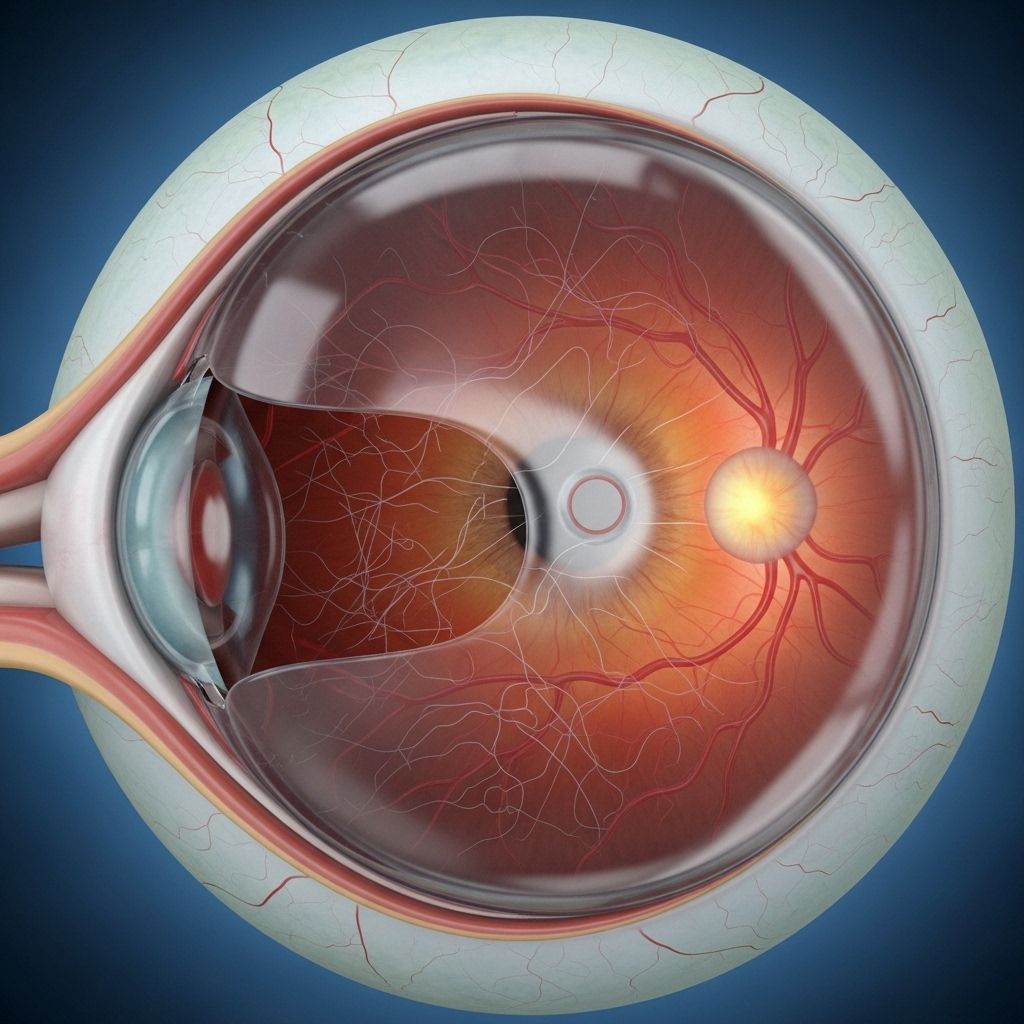
Posterior vitreous detachment (PVD) is a very common eye condition, mostly seen in adults over 50, where the gel-like substance inside your eye (the vitreous) separates from the retina at the back. This process is typically part of natural aging and most cases are benign, but there are important warning signs and rare complications to recognize, making timely assessment critical.
What Is Posterior Vitreous Detachment?
PVD occurs when the vitreous gel, which fills the middle portion of the eye and is attached to the retina, begins to shrink and pull away from the retina. The retina is the light-sensitive layer lining the inner back of your eye, responsible for transmitting visual information to your brain.
As the separation happens, some people experience symptoms, while others barely notice. Although PVD itself typically doesn’t cause vision loss, complications like retinal tears or detachments can threaten sight and require urgent attention.
- Common Age-Related Change: Most people will develop PVD at some point, usually after age 50.
- Natural Process: The shrinking and separation of the vitreous gel is normal as we age.
- Potential Complications: Most cases are harmless, but some can lead to serious retinal disorders requiring prompt treatment.
Causes of Posterior Vitreous Detachment
PVD happens because the composition of the vitreous gel changes with age. The gel, formed mostly of water, collagen, and hyaluronic acid, loses its firmness over the decades.
- Aging: The main cause, as proteins (like collagen) break down, causing the gel to liquefy and shrink.
- Loss of Gel Volume: When the shrinking gel can’t fill the eye cavity fully, it pulls away from the retina.
- Breaking of Attachment: Tiny fibers attaching the vitreous gel to the retina weaken and snap, completing the detachment process.
- Other Risk Factors:
- Nearsightedness (myopia)
- Previous cataract surgery
- Eye trauma
- Certain retinal disorders
PVD generally occurs gently and gradually; however, strong or uneven forces, or abnormal adhesions (e.g. lattice degeneration), can cause troubling complications such as tearing of the retina or bleeding within the eye.
Symptoms of Posterior Vitreous Detachment
PVD symptoms often begin suddenly and can be alarming. However, these symptoms typically settle over several weeks or months, as your brain adapts. It’s vital to differentiate between harmless symptoms and warning signs of more significant retinal problems.
- Floaters: Tiny dark spots, strings, or clumps drifting in your vision, sometimes described as spider webs, circles, or dots.
- Flashes of Light: Brief flashes, arcs, or streaks of light in peripheral vision, especially in dimly-lit environments.
- Blurry Areas or Shadows: Less common, but may indicate a more serious issue if persistent or spreading.
- Arc of Light or Shadow: Sudden or persistent arc-shaped lights or shadows could accompany the onset.
Note: The symptoms of PVD may closely resemble those of a retinal detachment, which is a medical emergency. Immediate assessment by an eye care provider is necessary if you notice new floaters, flashes, or visual shadows.
How Is PVD Diagnosed?
Because PVD can mimic more dangerous conditions, eye doctors rely on thorough examination and specialized diagnostic tools:
- Comprehensive Eye Exam: Assessment by an ophthalmologist or optometrist, including discussion of symptoms and medical history.
- Dilated Retinal Exam: Eye drops widen your pupils, allowing a better view of the retina with special lenses and lights.
- Imaging: Sometimes, diagnostic imaging like optical coherence tomography (OCT) or ultrasound helps reveal the state of the vitreous and retina.
Patients with sudden new symptoms should seek eye care within 24 hours, especially if experiencing flashes, many floaters, or peripheral shadows. Prompt diagnosis helps rule out retinal tears and detachment.
Potential Complications of Posterior Vitreous Detachment
While most cases resolve safely, a minority develop problems that, if left untreated, threaten vision. These include:
- Retinal Tears: Occur in up to 10–15% of those with PVD. Tears can allow fluid to seep behind the retina, risking detachment.
- Retinal Detachment: The retina separates from underlying tissue; sight may be lost permanently if not repaired promptly.
- Macular Hole: A break in the central retina affecting fine, detailed vision.
- Vitreous Hemorrhage: Bleeding into the vitreous cavity, causing a sudden haze or loss of vision.
- Epiretinal Membrane Formation: Scar tissue forming on the retina’s surface, sometimes distorting vision.
Seek immediate care if you notice a sudden curtain or shadow crossing your vision, loss of central vision, or a sudden spike in floaters or flashes.
Treatment and Management of PVD
Most people with PVD do not require any treatment, especially if uncomplicated. Symptoms fade as the brain adapts and floaters settle. However, ongoing monitoring and specific interventions are sometimes necessary:
- No Treatment Needed: Typical cases are benign. Regular follow-up exams may be recommended during the symptomatic period.
- Surgical Treatment: Rarely, surgery called vitrectomy is performed if a dense vitreous hemorrhage is present, or to address retinal tears, holes, or detachments.
- Laser Treatment: If retinal tears are discovered, laser therapy may seal the tear and prevent detachment.
Vitrectomy: What to Expect
Vitrectomy is a procedure to remove the vitreous gel and hemorrhage, allowing the retina to be thoroughly examined and treated:
- Outpatient Surgery: Performed with local anesthesia, typically taking 15–25 minutes.
- Small Ports: Three tiny openings allow entry of instruments including infusion cannula, light pipe, and vitrectomy cutter.
- Gel Removal: Balance salt solution replaces removed gel, and the surgeon locates and treats retinal breaks, tears, or detachment.
- Intravitreal Gas Bubble: Sometimes used to hold the retina in place while healing occurs following laser therapy.
- Post-Operative Care: No sutures are typically needed, and a patch is worn overnight.
Living with PVD: What to Monitor
For most patients, life quickly returns to normal after the initial symptoms subside. Nevertheless, continual vigilance for new or worsening symptoms is key to preventing sight-threatening complications.
- Floaters and flashes often diminish over weeks or months.
- 85% of cases do not develop further complications.
- Regular checkups may be recommended for a few months after PVD symptoms begin.
- Any sudden change in vision deserves immediate evaluation.
Prevention and Risk Reduction
While aging is unavoidable and the main driver of PVD, you can still minimize risk and respond quickly to problems with these steps:
- Protect Your Eyes: Wear protective eyewear during sports or risky activities to avoid trauma.
- Manage Underlying Conditions: Keep diabetes, blood pressure, and cholesterol under control.
- Monitor Vision: Be aware of visual changes; have regular eye exams especially if you are over 50, nearsighted, or have had previous eye surgery.
- Quick Response: Seek prompt medical attention for any new flashes, floaters, or vision loss.
Frequently Asked Questions (FAQs) About Posterior Vitreous Detachment
Q: Is PVD painful? Can it cause blindness?
A: PVD itself is painless and does not cause vision loss directly. However, complications like retinal tears or detachment can threaten sight and require immediate treatment.
Q: Do floaters and flashes ever go away?
A: Most patients find floaters and flashes improve or disappear over 1–3 months as the brain adapts and the vitreous settles. Persistent, worsening, or new symptoms must be checked by a doctor.
Q: Can PVD be prevented?
A: Since aging is the primary cause, PVD can’t be fully prevented, but risk of serious complications can be reduced through regular eye exams and protective measures.
Q: What should I do if I experience new floaters or flashes?
A: Visit an eye care professional within 24 hours for a comprehensive dilated retinal exam. Quick assessment is crucial to rule out retinal tears or detachment.
Q: What if I have had cataract surgery – am I at higher risk?
A: Yes, previous eye surgeries and eye trauma can increase the risk of PVD and related complications. Discuss your risk with your eye doctor and attend regular follow-up visits.
Quick Reference Table: PVD vs. Retinal Detachment
| Feature | Posterior Vitreous Detachment (PVD) | Retinal Detachment |
|---|---|---|
| Symptoms | Floaters, flashes, rarely mild shadow | Curtain or veil over vision, severe vision loss |
| Pain | Painless | Painless |
| Vision Loss | Usually absent | Often severe and urgent |
| Urgency of Treatment | Rule out retinal tear promptly | Requires immediate treatment |
| Outcome | Symptoms usually settle; good prognosis | Can result in permanent sight loss if untreated |
Key Takeaways
- PVD is a natural age-related change inside the eye, occurring commonly after age 50.
- Most cases don’t need treatment and settle with time, but a minority develop sight-threatening complications such as retinal tears or detachment.
- Classic symptoms include floaters and flashes; immediate evaluation is essential for new, changing, or severe symptoms.
- Regular eye examination and awareness of warning signs help prevent permanent vision loss.
- Contact an eye care professional promptly if you experience sudden changes in vision.
References
- https://www.retinacenternj.com/diseases-treatment/posterior-vitreous-detachment-pvd
- https://www.asrs.org/patients/retinal-diseases/9/posterior-vitreous-detachment
- https://www.webmd.com/eye-health/posterior-vitreous-detachment-facts
- https://www.rnib.org.uk/your-eyes/eye-conditions-az/posterior-vitreous-detachment/
- https://my.clevelandclinic.org/health/diseases/14413-posterior-vitreous-detachment
- https://www.mdfoundation.com.au/about-macular-disease/other-macular-conditions/pvd-and-floaters/
- https://www.retinamn.com/retinal-conditions/posterior-vitreous-detachment
- https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/vitreous-detachment
- https://www.mayoclinic.org/diseases-conditions/retinal-detachment/symptoms-causes/syc-20351344
Read full bio of medha deb












