Posterior Subcapsular Cataract: Causes, Symptoms, Diagnosis, and Treatment
Get expert insights on posterior subcapsular cataracts—from symptoms and causes to latest treatment, prevention tips, and FAQs.
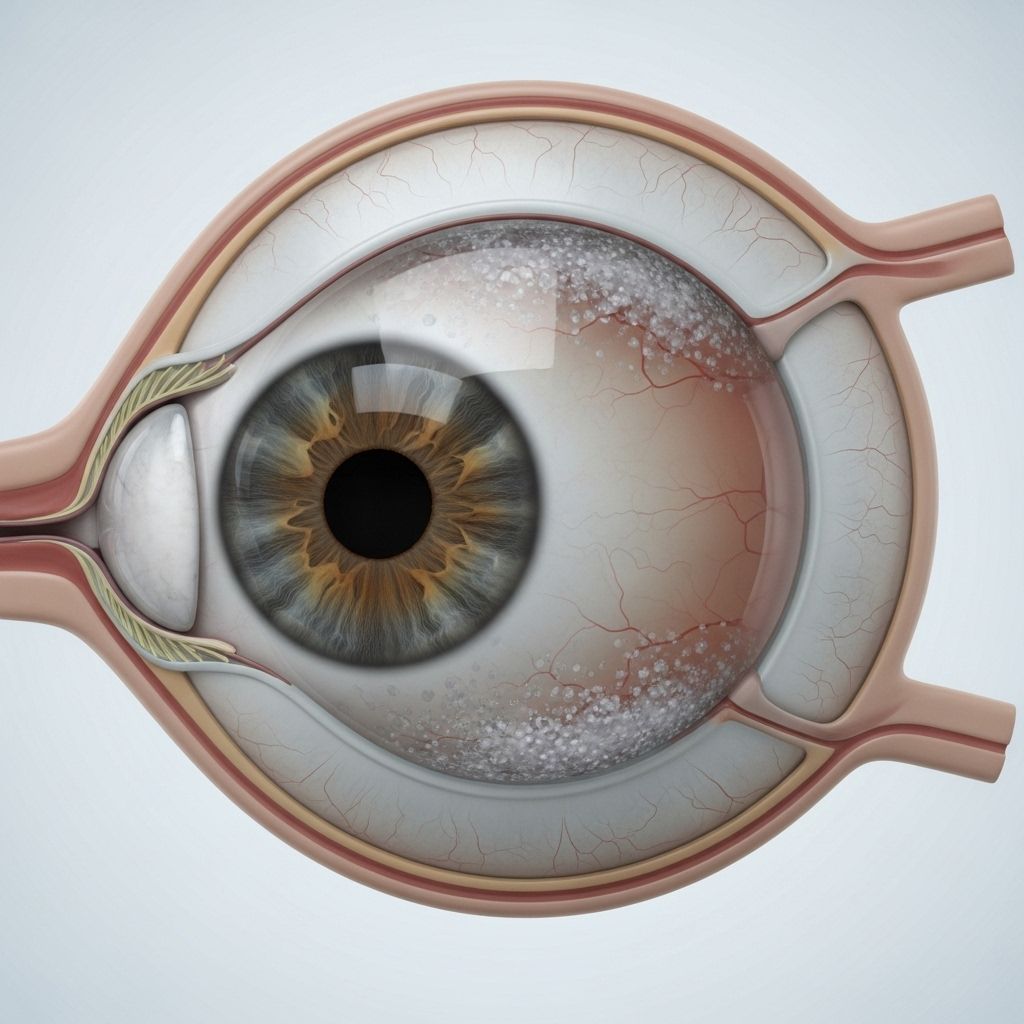
Posterior Subcapsular Cataract Overview
Posterior subcapsular cataract (PSC) is a specific type of cataract characterized by a cloudy or opaque area that develops on the back surface of the eye’s lens, just in front of the posterior lens capsule. Although less common than other forms of cataracts, PSC tends to progress more rapidly and may lead to significant vision problems. Understanding the symptoms, risk factors, diagnosis, and treatment of PSC is essential for effective management and maintaining eye health.
What Is a Posterior Subcapsular Cataract?
A posterior subcapsular cataract forms at the rear portion of the crystalline lens, specifically in the subcapsular space. Unlike other cataracts that develop mainly due to aging, PSC can also affect younger individuals, especially those with certain medical conditions or those exposed to specific risk factors.
- Location: Occurs at the back of the lens capsule.
- Quick Progression: PSC often develops faster than other types of cataracts.
- Prevalence: Accounts for about 3% of cataracts based on population studies.
Understanding the Eye’s Lens and Cataract Formation
The lens inside the eye is made up of highly organized fibers and water, which allow light to pass through and focus on the retina. Over time or when exposed to certain risk factors, proteins within these fibers can clump and form opacities, interfering with vision. PSC differs from other types of cataracts due to its position and the speed with which it impairs vision.
Symptoms of Posterior Subcapsular Cataract
PSC is notorious for causing more rapid and severe visual symptoms compared to other cataracts. Recognizing these symptoms early can lead to timely intervention and treatment.
- Blurring of vision: Especially pronounced when performing tasks that require focus, such as reading.
- Glare and halos: Difficulty seeing because of bothersome glare from sources of bright light like headlights or sunlight, often accompanied by halos around lights.
- Sensitivity to light: Increased discomfort or pain in bright environments.
- Defective near vision: Problems with activities such as reading, which require clear near vision.
- Reduction in contrast sensitivity: Difficulty distinguishing objects in low-contrast situations.
- Diplopia or polyopia (in some cases): Seeing multiple images or double vision.
As the cataract progresses, these symptoms can worsen rapidly, resulting in marked difficulty with daily activities that require clear vision.
Causes and Risk Factors for PSC
Multiple factors contribute to the development of posterior subcapsular cataracts. Many are related to general health and environmental exposures, while some are genetic or idiopathic.
- Aging: Natural aging processes promote the buildup and clumping of lens protein fibers.
- Long-term corticosteroid use: Extended exposure to corticosteroid medications significantly increases the risk of PSC.
- Medical conditions: Diabetes mellitus is a principal risk factor, as is retinitis pigmentosa and chronic intraocular inflammation (like uveitis).
- Radiation exposure: History of radiation therapy or excessive UV exposure can damage lens proteins and increase risk.
- Eye trauma: Previous blunt trauma to the eye may precipitate PSC formation.
- Genetic predispositions: Conditions such as atopic dermatitis and other skin disorders may be associated with PSC.
- High myopia (extreme nearsightedness): Patients with high refractive errors are more susceptible.
- Underlying systemic diseases: Other autoimmune or inflammatory diseases can contribute to risk.
- Lifestyle factors: Smoking, excessive alcohol consumption, obesity, and poor diet may further raise risk.
How PSC Develops: Pathophysiology
Posterior subcapsular cataracts develop when the orderly arrangement of lens fibers is disrupted, particularly in the subcapsular region. The following steps outline this process:
- With aging or risk factor exposure, lens fibers become overactive, sometimes triggered by new growth beneath the lens capsule.
- Protein fibers clump and scatter, creating an opaque cluster within the subcapsular region.
- This opacity interferes with light transmission, especially in the central area of focus, leading to rapid visual deterioration.
Diagnostic Methods for Posterior Subcapsular Cataract
Diagnosis starts with a comprehensive eye examination by an ophthalmologist, including direct observation and imaging techniques.
- Slit-lamp examination: Allows the clinician to visualize the lens and detect subcapsular opacities.
- Reduced visual acuity testing: Confirms decreased vision and assesses how cataract is affecting daily functioning.
- Contrast sensitivity testing: Evaluates the ability to perceive objects against a background.
- Additional diagnostic tests: May include fundus examination or imaging if other ocular pathology is suspected.
Classification of PSC by Size
| PSC Stage | Size (mm) | Description |
|---|---|---|
| PSC 1+ | 1–2 mm | Early stage, mild visual symptoms |
| PSC 2+ | 2–3 mm | Moderate progression, vision increasingly affected |
| PSC 3+ | >3 mm | Advanced stage, significant functional impairment |
Posterior Subcapsular Cataract vs. Other Types of Cataract
| Type | Location | Prevalence (%) | Rate of Progression |
|---|---|---|---|
| Posterior Subcapsular Cataract (PSC) | Back of lens capsule | 3 | Rapid |
| Cortical Cataract | Lens cortex (outer layer) | 8 | Moderate |
| Nuclear Cataract | Central portion of lens | 13 | Slow |
Prevention Strategies
While not all cases of PSC can be prevented, several steps may reduce your risk:
- Limit corticosteroid use: Use only when medically necessary under guidance from a healthcare provider.
- Manage systemic diseases: Control diabetes and inflammatory conditions with regular medical care.
- Protect eyes from UV radiation: Wear sunglasses that block ultraviolet light when outdoors.
- Maintain overall health: Follow a balanced diet, avoid smoking, and limit alcohol intake.
- Add regular eye exams: Routine examinations allow early detection and intervention.
Treatment Options for PSC
Once PSC starts to impact daily life or vision significantly, surgery is the primary and most effective treatment. Currently, no medications can reverse or halt PSC progression; only surgical removal restores vision.
- Cataract surgery: The diseased lens is removed and replaced by an artificial intraocular lens (IOL). The most common technique is phacoemulsification—a minimally invasive procedure performed under local anesthesia.
- Day surgery: Most surgeries are outpatient, typically completed within 15–30 minutes.
- Recovery: Patients usually go home the same day, with full recovery expected in 6–8 weeks.
- Post-operative care: Eye drops and limiting activities are required to prevent infection and ensure successful healing.
- Vision correction: Some patients may require glasses after surgery depending on the type of IOL implanted.
Advanced Surgical Techniques
PSC cataracts are commonly treated with phacoemulsification:
- Ultrasound probe breaks up the cloudy lens (phaco probe).
- Lens fragments are removed, and an intraocular lens is placed for clear vision.
- Surgical success rate is virtually 100%, with most patients experiencing significant vision improvement.
Living With Posterior Subcapsular Cataract
Rapid progression and impact on near vision can make PSC particularly challenging. Proper adaptation and preparation for surgery are essential. Key recommendations include:
- Seek prompt consultation with an ophthalmologist if symptoms develop.
- Maintain eye protection and healthy habits.
- Discuss individual risk factors and medication history with your doctor.
- Follow up regularly for early detection and management of PSC or other ocular problems.
Frequently Asked Questions (FAQs)
What differentiates posterior subcapsular cataracts from other cataracts?
PSC develops at the back of the lens and tends to progress faster, often impacting near vision and causing more noticeable glare and halos than cortical or nuclear cataracts.
Who is most at risk for PSC?
Individuals with diabetes, those who use corticosteroids long-term, people with skin conditions (e.g., atopic dermatitis), and those exposed to radiation or trauma are at greater risk.
Can PSC be reversed without surgery?
No current medication or therapy can reverse PSC; surgery is required when vision is impaired.
Is cataract surgery for PSC safe?
Yes, modern cataract surgery (most commonly phacoemulsification) is a safe, outpatient procedure with very high success rates and rapid recovery.
What are signs I need cataract surgery?
If PSC causes difficulty with reading, driving, or other daily activities, and vision is not adequately corrected with glasses, surgery is usually recommended.
Key Takeaways
- PSC is a rapidly progressing cataract found at the back of the lens, often resulting in glare, halos, and defective near vision.
- Risk factors include aging, steroids, diabetes, radiation, trauma, and genetic conditions.
- Surgery is the only definitive treatment, carried out through safe, effective outpatient techniques.
- Early detection and preventive care can minimize risk and ensure best outcomes for eye health.
References and Further Reading
- All About Vision: Overview and Causes of PSC
- Dr. Agarwal’s Eye Hospital: Symptoms and Treatments
- West Boca Eye Center: Surgical Approach and Staging
- NeoRetina: Causes, Risk Factors, and Pathophysiology
References
- https://www.allaboutvision.com/conditions/cataracts/posterior-subcapsular/
- https://www.dragarwal.com/diseases-conditions/cataract/posterior-subcapsular-cataract/
- https://www.neoretina.com/blog/how-to-outpace-posterior-subcapsular-cataracts/
- https://www.westbocaeyecenter.com/post/what-is-a-posterior-subcapsular-cataract
- https://www.drsimonskalicky.com.au/blog/posterior-subcapsular-cataracts-how-they-are-caused-and-possible-treatment/
- https://www.mayoclinic.org/diseases-conditions/cataracts/symptoms-causes/syc-20353790
- https://my.clevelandclinic.org/health/diseases/8589-cataracts-age-related
- https://my.clevelandclinic.org/health/diseases/24737-posterior-capsular-opacification
Read full bio of Sneha Tete












