Pneumocystis Pneumonia (PCP): Causes, Symptoms, Diagnosis, and Treatment
A comprehensive overview of Pneumocystis pneumonia (PCP)—covering risk, causes, symptoms, diagnosis, treatment, prognosis, and FAQs.
Pneumocystis Pneumonia (PCP): What You Need to Know
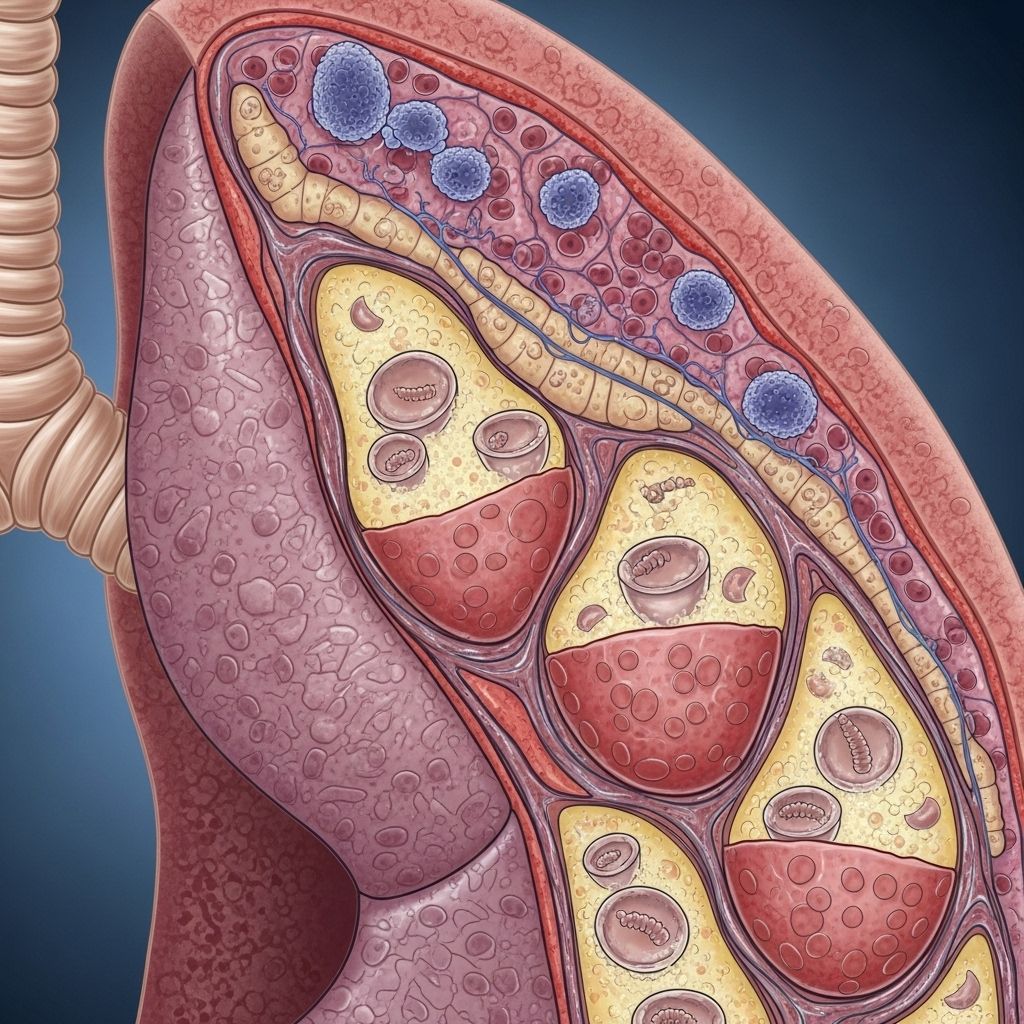
Pneumocystis pneumonia (PCP) is a dangerous lung infection caused by the fungus Pneumocystis jirovecii. It primarily targets individuals with weakened immune systems and can quickly become life-threatening without prompt diagnosis and treatment.
What is Pneumocystis Pneumonia?
Pneumocystis pneumonia (PCP)—formerly known as Pneumocystis carinii pneumonia—results from infection by the fungus Pneumocystis jirovecii. Unlike many other fungal respiratory infections, PCP almost exclusively affects those whose immune defenses are significantly compromised. Although this fungus is widespread in the environment, it rarely causes trouble in healthy people. However, when the body’s defenses are low, severe lung infection may occur, leading to dangerous complications if left untreated.
Who is at Risk for PCP?
PCP is most common in people with weakened immunity. Groups at risk include:
- People with HIV/AIDS, especially if their CD4 count is low
- Those undergoing chemotherapy for cancer
- Organ or bone marrow transplant recipients on immunosuppressants
- Individuals on long-term, high-dose corticosteroid therapy
- Patients with other medical conditions or treatments that reduce immune function
Before the development of effective HIV treatments and widespread use of preventive antibiotics, PCP was a leading cause of pneumonia among individuals with AIDS.
PCP Transmission and Causes
The fungus Pneumocystis jirovecii is present in the environment, likely spreading through the air from person to person. Most people are exposed during childhood, but the infection remains dormant unless the immune system becomes compromised. PCP is not classified as a contagious disease in the same way as the flu or common cold, but outbreaks can occur in health care settings or among groups with shared exposures if many are immunosuppressed.
- PCP does not commonly affect people with healthy immune systems.
Symptoms of Pneumocystis Pneumonia
Symptoms of PCP can begin gradually and worsen over days or weeks. The severity may differ depending on the patient’s immune status. Common symptoms include:
- Fever
- Dry cough (often mild, but persistent)
- Shortness of breath—worse with exertion and gradually worsening
- Fatigue
- Chest pain or tightness
- Chills
In severe cases, symptoms can rapidly progress to respiratory failure. The hallmark sign is difficulty breathing, especially during activity. People with AIDS may have a slower onset of symptoms, while those with other causes of immune suppression may experience a more sudden and severe course.
Complications of PCP
- Respiratory failure
- Hypoxemia (very low oxygen levels in blood)
- Enlargement, or rupture, of air spaces (pneumothorax/air leak)
- Secondary bacterial pneumonia or other lung infections
- Potential spread to other organs (rare)
Because PCP can quickly become severe or fatal, early recognition and intervention are crucial.
How is PCP Diagnosed?
Early and accurate diagnosis is critical, as the condition can be life-threatening. Diagnosis usually involves a combination of the following:
- Physical examination and assessment of symptoms
- Imaging studies:
- Chest X-ray: May show characteristic diffuse, bilateral interstitial infiltrates—but imaging can vary
- CT scan: More sensitive for early changes
For those seeking information on respiratory problems and their implications, we recommend reading about whooping cough (pertussis) in adults: symptoms, risks, and prevention. This knowledge is essential for managing respiratory health, especially in vulnerable populations. - Laboratory tests:
- Blood tests: Low oxygen levels (hypoxemia), abnormal white blood cell counts
- Elevated lactate dehydrogenase (LDH)
- Definitive diagnosis by identifying the fungus in respiratory samples:
- Sputum analysis: Patient coughs up mucus sample
- Induced sputum: Saline mist inhaled to produce deeper mucus
- Bronchoalveolar lavage (BAL): Procedure using a thin tube (bronchoscope) to wash out cells/fluid from the lungs for analysis
- Biopsy: Occasionally, a tiny piece of lung tissue is taken if diagnosis is unclear
To grasp the complexities of related cardiovascular issues that may exacerbate pulmonary conditions, explore our Eisenmenger Syndrome guide: causes, symptoms, diagnosis, and modern treatments. This knowledge can aid in understanding the interplay between heart and lung health.
Molecular tests (PCR) and special stains help confirm Pneumocystis organisms in lab samples. Classic cultures are not used because the fungus does not grow in regular culture media.
PCP Treatment Options
The mainstay of PCP treatment is antibiotics. The primary (and most effective) choice is:
- Trimethoprim-sulfamethoxazole (TMP-SMX) (also known as co-trimoxazole or by brand names such as Bactrim, Septra, Cotrim): Given by mouth or intravenously for at least 21 days.
Other important aspects of treatment include:
- Hospitalization for moderate to severe cases
- Oxygen therapy for low blood oxygen
- Corticosteroids (such as prednisone) for moderate to severe PCP—the aim is to reduce lung inflammation, especially when oxygen levels are low
- Alternative antibiotics (for people who cannot tolerate TMP-SMX):
- Atovaquone
- Dapsone (often with another drug called trimethoprim)
- Clindamycin plus primaquine
- Pentamidine (usually given by intravenous infusion)
- Desensitization: For people with milder allergies to TMP-SMX, a gradual increase in dosage may be attempted under medical supervision
It’s critical to note: Pneumocystis pneumonia is treated with antibiotics—not antifungal medications. Even though the organism is a fungus, typical antifungal drugs do not work against PCP.
Monitoring and Supportive Care
- Patients may need breathing support through a ventilator in severe cases
- Monitoring for side effects (such as rash, fever, low blood counts) from antibiotics
- Hydration and supportive medical care throughout recovery
Prognosis and Recovery
When diagnosed and treated early, many people recover fully from PCP. However, the course can be severe, especially for those with other serious medical conditions. Factors affecting prognosis include:
- Underlying immune status (people with advanced HIV/AIDS or recent transplantation face higher risks)
- Severity at the time of diagnosis
- Timeliness and appropriateness of therapy
Complications related to severe hypoxemia or secondary infections can be life-threatening. Long-term follow-up care may be required to monitor for recurrence or chronic lung damage.
Can PCP be Prevented?
No vaccine exists to prevent Pneumocystis pneumonia at this time. However, powerful measures help reduce the risk in at-risk individuals:
- Prophylactic antibiotics:
- People at high risk (for example, those with HIV/AIDS and low CD4 counts, transplant recipients, and those on high-dose corticosteroids) may be prescribed TMP-SMX or other antibiotics on a preventive basis
- Alternative medications are available for those allergic to TMP-SMX
- Timely antiretroviral therapy in HIV/AIDS to strengthen the immune system
- Careful monitoring and tailored medical care in other immunosuppressed patients
Prophylactic medicines have drastically reduced the incidence of PCP in many high-risk groups.
When to Seek Medical Attention
Early intervention is essential. You should seek emergency medical attention if you have a weakened immune system and experience:
- Shortness of breath not explained by routine activity
- Severe or worsening cough
- Chest pain, especially with breathing
- High fever or chills
- Extreme fatigue
If you fall into a high-risk group (HIV/AIDS, cancer therapy, organ transplant, etc.), discuss any new respiratory symptoms promptly with your healthcare provider.
Frequently Asked Questions (FAQs) about PCP
Q: Is PCP contagious?
A: PCP is caused by a fungus that is present in the general environment. While it is not considered highly contagious, rare outbreaks can occur among healthcare settings or immunosuppressed populations. Healthy people are unlikely to contract PCP even after exposure.
Q: How is PCP different from other types of pneumonia?
A: Unlike bacterial or viral pneumonia, PCP almost exclusively affects people with severely weakened immunity. The infection is slow and progressive, with little or no mucus. In addition, the primary treatment is antibiotics designed for bacteria, not the standard antifungal drugs for other fungal infections.
Q: Who should get PCP prophylaxis?
A: PCP prevention is recommended for people with HIV/AIDS and low CD4 counts, transplant patients, those receiving certain cancer treatments, and others on high-dose immunosuppressive medications. Your healthcare provider will determine if you need preventive medication based on your risk factors.
Q: What are the risks of untreated PCP?
A: Untreated PCP can quickly progress to severe respiratory distress and potentially death. The risk is greatest in people whose immune systems are already compromised. Early diagnosis and therapy are critical for survival.
Q: Can you recover from PCP?
A: Yes. With prompt and appropriate treatment, many people recover fully from PCP. However, the risk of complications—especially in those with significantly weakened immunity—makes fast medical intervention vital.
Q: What is the outlook for people with PCP?
A: The prognosis has improved dramatically thanks to advances in treatment and prevention. Most people with early, appropriately managed PCP survive and recover.
Table: Comparison of PCP with Other Pneumonias
| Feature | Pneumocystis Pneumonia (PCP) | Bacterial Pneumonia | Viral Pneumonia |
|---|---|---|---|
| Main cause | Pneumocystis jirovecii fungus | Bacteria (e.g., Streptococcus pneumoniae) | Viruses (e.g., influenza, SARS-CoV-2) |
| Common in | Immunocompromised individuals | All age groups, especially elderly or those with underlying disease | All age groups, varies by virus |
| Symptoms onset | Gradual (days to weeks) | Acute (hours to days) | Acute or gradual |
| Classic symptoms | Fever, dry cough, progressive breathlessness, hypoxemia | Fever, productive cough, chest pain, chills | Fever, cough, muscle aches, shortness of breath |
| Main treatment | Antibiotics (TMP-SMX) | Antibiotics | Supportive care, antivirals (limited role) |
| Prevention | Prophylactic antibiotics for high-risk | Vaccination (for some pathogens), hygiene | Vaccination (for influenza, COVID-19), hygiene |
Key Takeaways
- PCP is a serious fungal lung infection affecting mainly immunocompromised people
- Prompt treatment with TMP-SMX antibiotics is usually effective
- Preventive antibiotics greatly reduce risk in high-risk groups—no vaccine is available
- Recognizing symptoms early is crucial for survival and recovery
References
- https://medlineplus.gov/pneumocystisinfections.html
- https://www.mountsinai.org/health-library/diseases-conditions/pneumocystis-jiroveci-pneumonia
- https://my.clevelandclinic.org/health/diseases/pneumocystis-pneumonia
- https://rarediseases.org/rare-diseases/pneumocystis-pneumonia/
- https://www.ncbi.nlm.nih.gov/books/NBK482370/
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/p/pneumocystis-pneumonia-or-pcp.html
- https://www.aafp.org/pubs/afp/issues/1999/1015/p1699.html
Read full bio of Sneha Tete












