Pneumoconiosis: Causes, Symptoms, Diagnosis, and Management
Learn about pneumoconiosis, a work-related lung disease caused by dust exposure, including types, signs, diagnosis, treatment, and prevention.
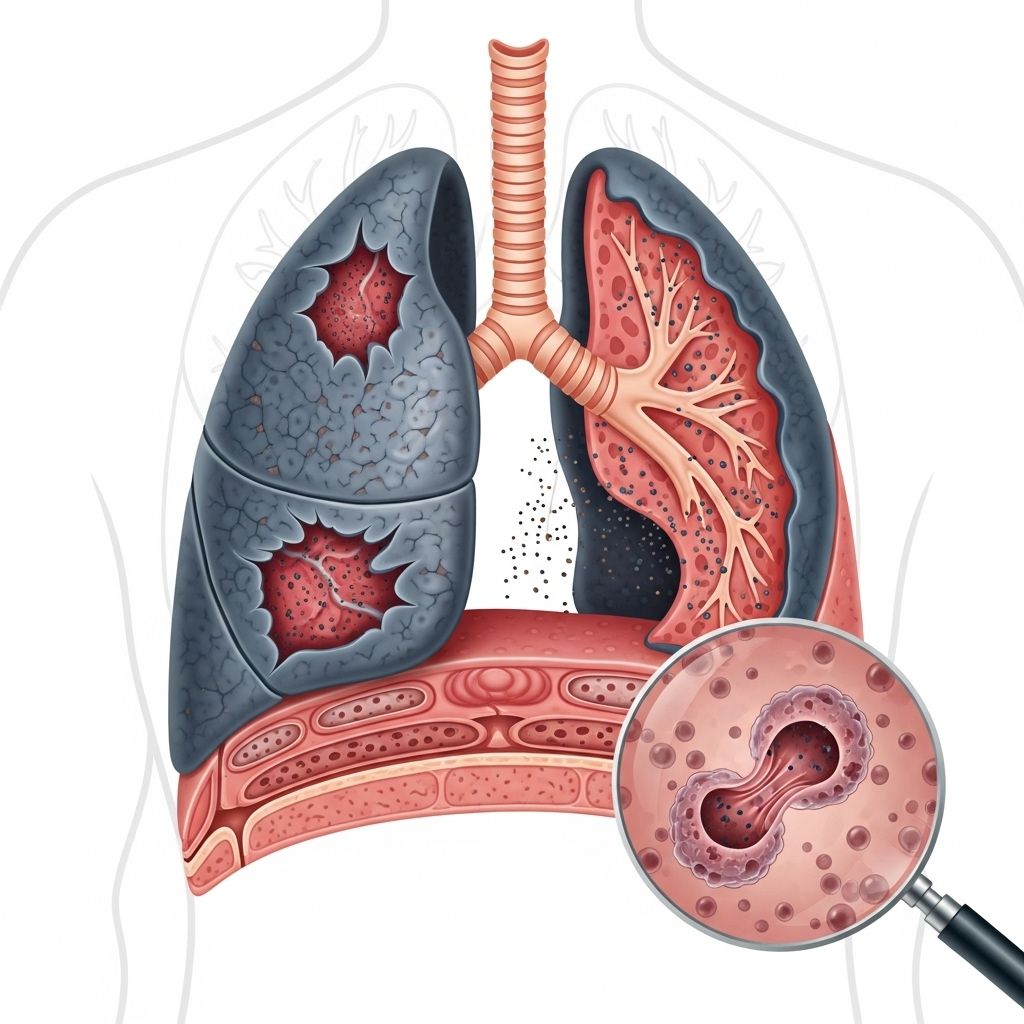
Pneumoconiosis is a group of lung diseases resulting from the inhalation of hazardous dust particles, most commonly in workplace settings. These particles settle deep within the lungs, triggering inflammation and, over time, scarring known as pulmonary fibrosis. Pneumoconiosis develops gradually and can lead to severe respiratory impairment.
Understanding Pneumoconiosis
Pneumoconiosis refers to a category of occupational lung diseases caused by breathing in mineral, chemical, or organic dusts over prolonged periods. The disease is primarily associated with certain job environments, such as mining, construction, quarrying, shipbuilding, and industries that generate fine dust. The scarring and tissue damage in the lungs makes it difficult for patients to breathe and can result in significant, lasting health problems.
- Coal worker’s pneumoconiosis (CWP): Also known as black lung disease, caused by inhaling coal dust.
- Silicosis: Caused by inhaling silica dust, often found in sandblasting, mining, and stone cutting.
- Asbestosis: Caused by inhaling asbestos fibers, common in shipbuilding, insulation work, and demolition.
- Byssinosis: Linked to inhalation of cotton, flax, or hemp dust; often called “brown lung” in textile workers.
- Other rarer types: Occur from exposure to aluminum, barium, graphite, iron, kaolin, mica, talc, and diacetyl (popcorn lung).
How Pneumoconiosis Develops
When airborne dust particles are inhaled, they become lodged deep within the tiny air sacs (alveoli) of the lungs. The body’s immune system recognizes these foreign particles as threats and attempts to remove or destroy them, initiating an inflammatory response. Over the years, persistent inflammation leads to the formation of scar tissue (fibrosis) within the lungs. This scar tissue is stiff and thick, reducing the elasticity of the lungs and impairing oxygen exchange. The process is gradual and may remain asymptomatic or minimally symptomatic for a long period before severe respiratory symptoms emerge.
Simple vs. Complicated Pneumoconiosis
- Simple pneumoconiosis: Characterized by small, round spots of scar tissue known as nodules, often seen in X-rays. Most people do not experience major symptoms during the early stages.
- Complicated pneumoconiosis / Progressive Massive Fibrosis (PMF): Involves extensive scarring, resulting in large areas of fibrosis that cause significant respiratory symptoms and decreased lung function.
Major Causes of Pneumoconiosis
- Prolonged occupational exposure: The majority of cases arise from repeated, prolonged inhalation of hazardous dusts in workplaces such as coal mines, quarries, construction sites, textile mills, and factories handling asbestos or other minerals.
- Types of dusts linked to the disease:
- Coal dust
- Silica
- Asbestos
- Certain organic dusts (cotton fibers, for example)
- Less common: aluminum, barium, graphite, iron, kaolin, mica, talc, and diacetyl
It is rare for the disease to arise outside of occupational exposure. Household and environmental exposure levels are typically too low to cause pneumoconiosis.
Who is at Risk?
Pneumoconiosis predominantly affects workers exposed to respirable dusts for extended periods. The most vulnerable groups include:
- Coal miners (risk for CWP)
- Stone cutters, sandblasters, quarry workers (risk for silicosis)
- Insulators, demolition workers, shipyard workers (risk for asbestosis)
- Textile mill workers (risk for byssinosis)
- Individuals in industries handling specific metals or minerals
Additional factors that increase risk:
- High intensity of dust exposure
- Long duration of exposure (often years or decades)
- Smoking (increases lung vulnerability and worsens disease presentation)
Symptoms of Pneumoconiosis
The severity and presence of symptoms depend on the type and stage of the disease:
- Simple pneumoconiosis: Usually asymptomatic or only mild symptoms; sometimes detected incidentally by chest X-ray.
- Complicated pneumoconiosis / PMF:
- Chronic dry or productive cough (sometimes with dark or black sputum in CWP)
- Shortness of breath (dyspnea), especially upon exertion
- Increased production of phlegm
- Severe fatigue
- Fever (less common, may indicate infection or inflammation)
- Chest pain
Recognizing the symptoms and implications of lung nodules, especially for individuals at risk of pneumoconiosis, is vital for lung health management. Lung nodules can indicate various underlying issues, and timely evaluation is necessary. To gain insights into their causes, symptoms, diagnoses, and treatment options, check out our in-depth article on lung nodules.
Symptoms usually develop slowly, sometimes taking many years after first exposure. In advanced cases, even light physical activity can be difficult due to shortness of breath. People with some forms—such as asbestosis—may also experience pleural thickening or fluid buildup around the lungs.
Types of Pneumoconiosis
| Type of Pneumoconiosis | Main Cause | Primary Occupations Affected | Notable Features |
|---|---|---|---|
| Coal Worker’s Pneumoconiosis (CWP) | Coal dust | Coal miners | “Black lung”; cough with black phlegm |
| Silicosis | Silica dust | Miners, stone workers, sandblasters | Progresses rapidly with high exposure; risk for tuberculosis |
| Asbestosis | Asbestos fibers | Shipbuilders, insulators, demolition | Increases risk of lung cancer/mesothelioma |
| Byssinosis | Cotton, hemp, flax dust | Textile workers | Bouts of chest tightness and wheezing |
| Other rare types | Aluminum, iron, talc, diacetyl | Industry-specific workers | Type-dependent features, may mimic other lung diseases |
Diagnosis of Pneumoconiosis
Diagnosis is based on a combination of occupational history, clinical evaluation, imaging studies, and, occasionally, laboratory tests. Establishing the diagnosis involves:
- Detailed medical and work history: Key to identifying hazardous exposures.
- Chest X-rays: First step to identify characteristic patterns of lung scarring or nodules.
- High-resolution computed tomography (HRCT): Provides a detailed image of lung tissue and helps distinguish types and extent of lung damage.
- Pulmonary function tests: Assess lung function, detect restrictive or obstructive impairments, and help guide treatment.
- Laboratory tests: May be ordered to rule out infections or other interstitial lung diseases.
The International Labour Organization (ILO) has developed standards for radiological classification of pneumoconioses, crucial for diagnosis, severity grading, and surveillance. In the United States, specialized training—such as the B Reader Program operated by NIOSH—certifies physicians in chest X-ray interpretation for pneumoconiosis and related conditions.
Treatment and Management
There is no cure for pneumoconiosis, as the lung scarring is irreversible. However, several strategies are available to manage symptoms, slow disease progression, and improve quality of life:
- Avoidance of further dust exposure: Essential to prevent progression; may require a change in occupation or job duties.
- Smoking cessation: Smoking can worsen respiratory impairment and should be stopped immediately.
- Medications: Bronchodilators can help open airways. In some cases, corticosteroids may be used to reduce inflammation.
- Oxygen therapy: Prescribed for individuals with low blood oxygen levels to relieve breathlessness and improve daily function.
- Vaccinations: Influenza and pneumonia vaccines are recommended to reduce the risk of respiratory infections.
- Pulmonary rehabilitation: Exercise training, education, and support may benefit individuals with reduced lung function.
- Treatment of complications: Such as infections, heart problems, or additional lung diseases (e.g., tuberculosis).
Regular medical follow-up is important. In severe cases, advanced treatments like lung transplantation may be considered, though this is rarely an option due to the complexity of underlying health and eligibility factors.
Prevention Strategies
As pneumoconiosis is primarily occupational, prevention focuses on minimizing dust exposure in the workplace:
- Engineering controls: Adequate ventilation, dust suppression systems, and use of wet processes when cutting or grinding materials.
- Personal protective equipment (PPE): Approved respirators or masks must be worn when exposure cannot be eliminated.
- Workplace regulations: Adherence to Occupational Safety and Health Administration (OSHA) and Mine Safety and Health Administration (MSHA) standards for dust limits and safety protocols.
- Health surveillance: Regular lung function testing and chest imaging for at-risk workers to detect early disease.
- Training and education: Workers and employers should be educated about the risks, symptoms, and preventive measures related to hazardous dust exposures.
Enforcing safe workplace practices and promptly addressing hazardous exposures are the most effective ways to prevent new cases of pneumoconiosis.
Prognosis
The outlook for individuals with pneumoconiosis depends on the type, duration, and intensity of exposure, the stage of the disease at diagnosis, and the promptness of intervention. Simple forms may cause little or no disability, while progressive massive fibrosis or advanced silicosis/asbestosis can lead to severe, disabling respiratory failure and increased mortality. Early diagnosis, cessation of exposure, and proper management offer the best chance for a stable or slowed disease course.
Frequently Asked Questions (FAQs)
Q: What is the difference between pneumoconiosis and other lung diseases?
A: Pneumoconiosis specifically refers to lung conditions caused by sustained inhalation of inorganic dusts (like coal, silica, asbestos) at work. Other lung diseases, such as asthma or COPD, have different causes and mechanisms.
Q: Is pneumoconiosis contagious?
A: No, pneumoconiosis is not infectious or contagious. It arises solely from environmental or occupational dust exposure and will not spread from person to person.
Q: Can pneumoconiosis be reversed?
A: The lung scarring and tissue damage from pneumoconiosis cannot be reversed. Management focuses on relieving symptoms and preventing further exposure to harmful dust.
Q: Who should be screened for pneumoconiosis?
A: Workers in high-risk industries (mining, construction, shipbuilding, textile production, and manufacturing with hazardous dusts) should have regular health screenings, chest imaging, and lung function tests.
Q: Are there government programs to support affected workers?
A: Yes. In the US, governmental programs provide workplace safety standards and may offer compensation or support to workers who develop occupational diseases such as pneumoconiosis. Specific programs include the Black Lung Benefits Program for coal miners and the NIOSH B Reader Program for expert radiograph review.
Key Takeaways
- Pneumoconiosis is a preventable occupational lung disease caused by inhaling harmful dusts over long periods.
- The condition is most common among workers exposed to coal, silica, asbestos, or organic textile dusts.
- Symptoms typically develop only after years of exposure, with chronic cough and shortness of breath being most common.
- Treatment focuses on symptom relief and preventing further exposure; there is no cure for scarring once established.
- Prevention through workplace controls, PPE, education, and regular health monitoring is critical to protect workers.
References
- https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=134&ContentID=162
- https://www.webmd.com/lung/what-is-pneumoconiosis
- https://www.cdc.gov/niosh/pneumoconioses/about/index.html
- https://www.pulmonaryfibrosis.org/understanding-pff/types-of-pulmonary-fibrosis/occupationalpf
- https://www.cedars-sinai.org/health-library/diseases-and-conditions/p/pneumoconiosis.html
- https://www.lung.org/lung-health-diseases/lung-disease-lookup/black-lung/symptoms-diagnosis
- https://my.clevelandclinic.org/health/diseases/25135-black-lung-disease
- https://www.pulmonologyadvisor.com/ddi/pneumoconiosis/
Read full bio of Sneha Tete












