Pleurisy: Causes, Symptoms, Diagnosis, and Treatment
Understand pleurisy, its underlying causes, signs, diagnostic techniques, effective management, and prevention strategies.
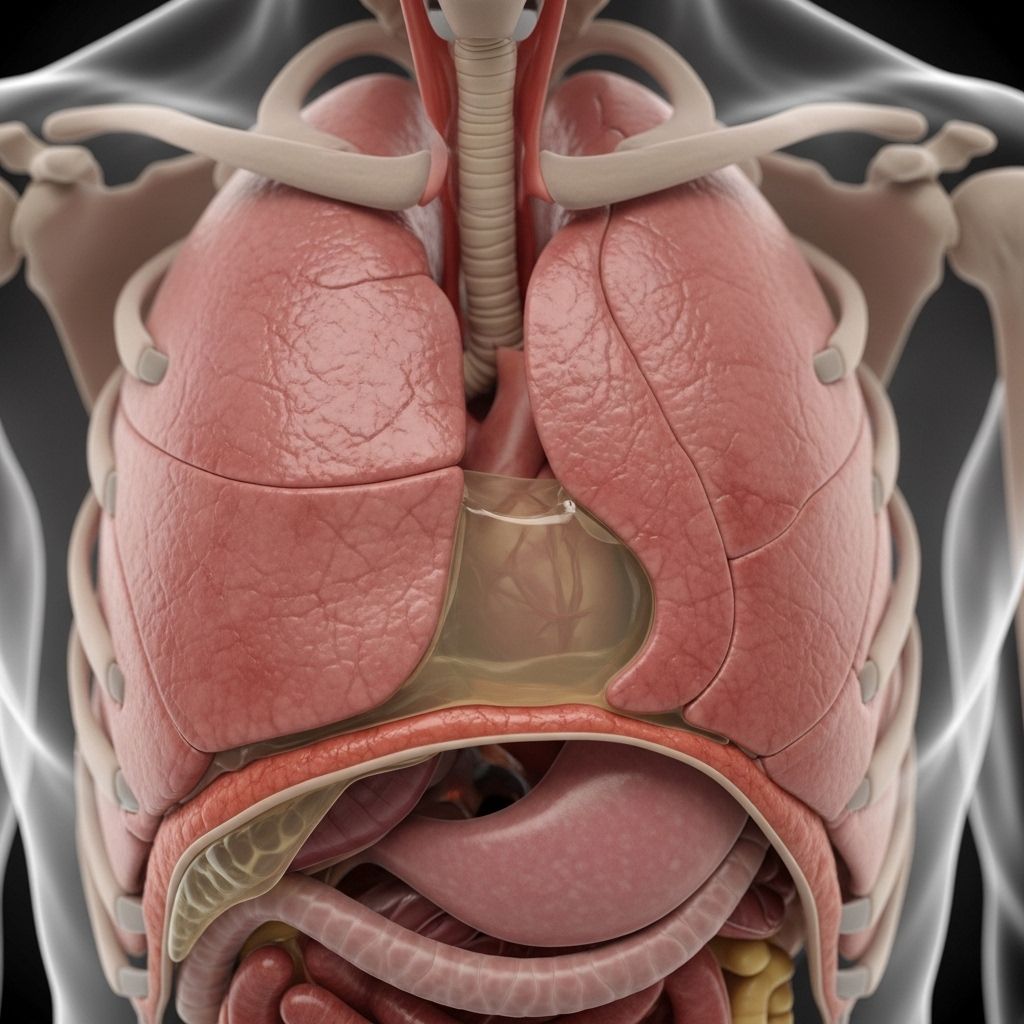
Pleurisy, sometimes referred to as pleuritis, is a condition in which the pleura—two thin layers of tissue surrounding the lungs—become inflamed. This inflammation can lead to sharp chest pain that worsens during breathing. Understanding pleurisy’s causes, signs, diagnostic methods, management, and preventive strategies can help patients and caregivers navigate this potentially serious but manageable condition.
What Is Pleurisy?
The pleura are two delicate, moist membranes that envelop each lung and line the inside of the chest cavity. The space between these layers, called the pleural space, normally contains a tiny amount of lubricating fluid to help the lungs move smoothly during breathing. When the pleura become inflamed or infected, they rub against each other, causing pleuritic pain—a hallmark symptom of pleurisy.
- Pleurisy refers specifically to inflammation of the pleura, resulting in sharp, stabbing chest pain, especially when inhaling deeply, coughing, or sneezing.
- The condition may be acute (of sudden onset and short duration) or, less commonly, chronic.
Causes of Pleurisy
A variety of conditions can cause pleurisy, most commonly infections. Addressing the underlying cause is essential for effective management.
- Viral Infections: The most common cause of pleurisy. Viruses such as influenza, Epstein-Barr, cytomegalovirus, and parainfluenza can spread to the pleural cavity and trigger inflammation.
- Bacterial Infections: Bacteria like Streptococcus pneumoniae, Staphylococcus aureus (including MRSA), and others can reach the pleura, often as a complication of pneumonia.
- Autoimmune Diseases: Conditions such as lupus and rheumatoid arthritis may cause the immune system to attack the pleura.
- Pulmonary Embolism: A blood clot in the lung can inflame the pleural layers, causing sudden pleuritic pain.
- Lung or Pleural Tumors: Malignancies such as lung cancer and mesothelioma may cause pleurisy, either directly or through associated effusions.
- Chest Trauma: Injury to the chest wall—such as rib fractures—can damage the pleura and initiate inflammation.
- Other Causes:
- Certain medications or drug-induced lupus
- Cancer treatments (chemotherapy, radiotherapy)
- HIV/AIDS or sickle cell anemia
- Inhalation of asbestos (asbestosis)
Symptoms of Pleurisy
Pleurisy characteristically causes chest pain, but associated symptoms can help identify the underlying cause.
- Sharp, stabbing chest pain that typically worsens with:
- Deep breathing
- Coughing
- Sneezing
- Movement of the chest or trunk
- Pain may be localized to one side of the chest but can radiate to the shoulder or back.
- Shortness of breath due to shallow breathing (to reduce pain).
- Occasionally, cough, fever, or chills if infection is present.
- Pleural effusion: Fluid buildup between the pleural layers may decrease pain but causes additional symptoms such as difficulty breathing and dry cough.
Who Is at Risk for Pleurisy?
Pleurisy can affect anyone, but certain factors may increase susceptibility:
- Individuals with recent respiratory infections (e.g., viral illnesses, pneumonia)
- People living with autoimmune diseases (e.g., lupus, rheumatoid arthritis)
- Those with a history of blood clots or pulmonary embolism
- Cancer patients, especially those with lung or pleural tumors
- People exposed to toxic substances (e.g., asbestos)
- Immunocompromised individuals
- Smokers
How Is Pleurisy Diagnosed?
Diagnosing pleurisy involves a combination of clinical evaluation, imaging studies, and laboratory tests to identify both the inflammation and its underlying cause.
Medical History and Physical Examination
- The healthcare provider will ask about symptoms, recent illnesses, and existing medical conditions.
- During examination, a distinctive ‘pleural rub’ may be heard with a stethoscope—a rough, grating sound during breathing caused by pleural layers rubbing together.
Diagnostic Tests
- Chest X-ray: Identifies lung infections, pleural effusion, or other abnormalities.
- CT Scan: Offers detailed images to reveal smaller or subtle pleural changes.
- Ultrasound: Detects pleural effusions and guides procedures to remove fluid.
- Blood Tests: Can identify infections, assess overall health, and check for autoimmune markers.
- Thoracentesis: If there is fluid buildup, a needle is used to extract pleural fluid for laboratory analysis. This can uncover infection, cancer cells, or other causes.
- Electrocardiogram (ECG): May be performed to rule out heart problems that mimic pleuritic symptoms.
Treatment of Pleurisy
The primary approach to treating pleurisy is addressing its root cause. Pain relief and supportive measures are also important to improve comfort and prevent complications.
Medications and Targeted Therapy
- Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen can reduce pain and inflammation. In severe cases, stronger analgesics may be prescribed.
- Antibiotics: If a bacterial infection (e.g., pneumonia) is present, appropriate antibiotics are required.
- Antiviral Medications: Used for severe or persistent viral infections causing pleurisy.
- Corticosteroids: For autoimmune-related pleurisy, steroids can decrease inflammation.
- Other Treatments: For specific causes, such as stopping the offending medication in drug-induced cases or cancer-directed therapy for tumor-associated pleurisy.
Pleural Effusion Management
- If pleurisy leads to significant fluid accumulation (pleural effusion), removal of fluid may be necessary to relieve symptoms and prevent complications.
- This can be achieved through thoracentesis or, for large or recurrent effusions, insertion of a chest tube.
Lifestyle and Home Remedies
- Medication adherence: Always take prescribed medicine as directed to control pain and treat the underlying condition.
- Rest: Find a comfortable position that alleviates pain, and avoid overexerting yourself even after initial improvement.
- Smoking cessation: Smoking further irritates the lungs and pleura. Quitting is crucial for recovery and prevention of further lung damage.
- Hydration and nutrition: Maintaining good overall health supports recovery.
Complications of Pleurisy
Early and effective management usually leads to complete recovery, but severe or untreated cases can cause complications:
- Pleural Effusion: Excess fluid collects in the pleural cavity, potentially leading to respiratory distress and infection (empyema).
- Lung Compression (Atelectasis): Large effusions may compress the lung, reducing oxygenation.
- Fibrosis: Chronic inflammation may cause scarring and thickening of the pleura, resulting in persistent symptoms and reduced lung function.
Prevention of Pleurisy
While not all cases can be prevented, certain measures may reduce risk:
- Avoid exposure to individuals with contagious respiratory infections, especially if immunocompromised.
- Practice good hand hygiene to curb the spread of viruses and bacteria.
- Seek prompt medical attention for lung infections to prevent spread to the pleura.
- Quit smoking and avoid exposure to harmful substances like asbestos.
- Manage underlying health conditions (such as autoimmune diseases) as recommended by a healthcare provider.
Living with Pleurisy
Most people recover from pleurisy with proper medical care, but the course may vary depending on the underlying cause. During recovery, focus on pain management, rest, and follow-up with your healthcare provider.
- If symptoms persist, worsen, or are accompanied by severe shortness of breath, seek immediate medical attention.
Frequently Asked Questions (FAQs)
Q: Is pleurisy contagious?
A: Pleurisy itself is not contagious, but the infection that causes it (such as certain viruses or tuberculosis) may be transmissible. Usually, only pleurisy caused by a contagious agent can be spread to others.
Q: How long does pleurisy last?
A: The duration varies. Viral pleurisy often improves within days to two weeks, while pleurisy from bacterial infections or other underlying conditions may require longer treatment.
Q: Can pleurisy come back?
A: Recurrence is possible, particularly if the underlying condition persists or recurs. Management of chronic health problems and preventive strategies can lessen the risk of recurrence.
Q: When should I see a doctor?
A: Seek medical attention if you experience sudden, unexplained chest pain, especially with difficulty breathing or fever. Early evaluation ensures timely diagnosis and effective treatment.
Q: What are the home remedies for pleurisy pain?
A: Pain relief can be improved by resting in a comfortable position, taking medications as prescribed, and avoiding activities that trigger pain. However, always consult with your healthcare provider for initial assessment and to address the underlying cause.
Summary Table: Key Facts About Pleurisy
| Aspect | Details |
|---|---|
| Definition | Inflammation of the pleura, resulting in chest pain |
| Main Causes | Viral and bacterial infections, autoimmune diseases, pulmonary embolism, cancer, trauma |
| Symptoms | Sharp chest pain that worsens with breathing, coughing; shortness of breath |
| Diagnosis | History, physical exam, imaging (X-ray, CT), lab tests, thoracentesis |
| Treatment | Pain relief (NSAIDs), antibiotics/antivirals if infection, steroids for autoimmune, treat underlying cause |
| Complications | Pleural effusion, lung compression, fibrosis, respiratory failure |
| Prevention | Promptly treat infections, quit smoking, manage health conditions |
Further Resources
- Contact your healthcare provider for individual advice.
- For urgent symptoms such as severe chest pain or shortness of breath, seek emergency medical attention.
References
- https://www.youtube.com/watch?v=2w_iDVLTzHk
- https://www.uofmhealthsparrow.org/departments-conditions/conditions/pleurisy
- https://www.mayoclinic.org/diseases-conditions/pleurisy/diagnosis-treatment/drc-20351866
- https://www.aafp.org/pubs/afp/issues/2007/0501/p1357.html
- https://www.medicalnewstoday.com/articles/158813
- https://my.clevelandclinic.org/health/diseases/21172-pleurisy
- https://www.mayoclinic.org/diseases-conditions/pleurisy/symptoms-causes/syc-20351863
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/pleurisy
- https://www.adventhealth.com/blog/pleurisy-101-causes-symptoms-and-treatment-options
- https://www.nhs.uk/conditions/pleurisy/
Read full bio of medha deb












