Platelet-Rich Plasma (PRP) Injections: Advancing Musculoskeletal Healing
Discover how platelet-rich plasma (PRP) injections are used to accelerate healing and treat musculoskeletal conditions, offering a minimally-invasive, personalized approach.
Platelet-Rich Plasma (PRP) Injections: Introduction
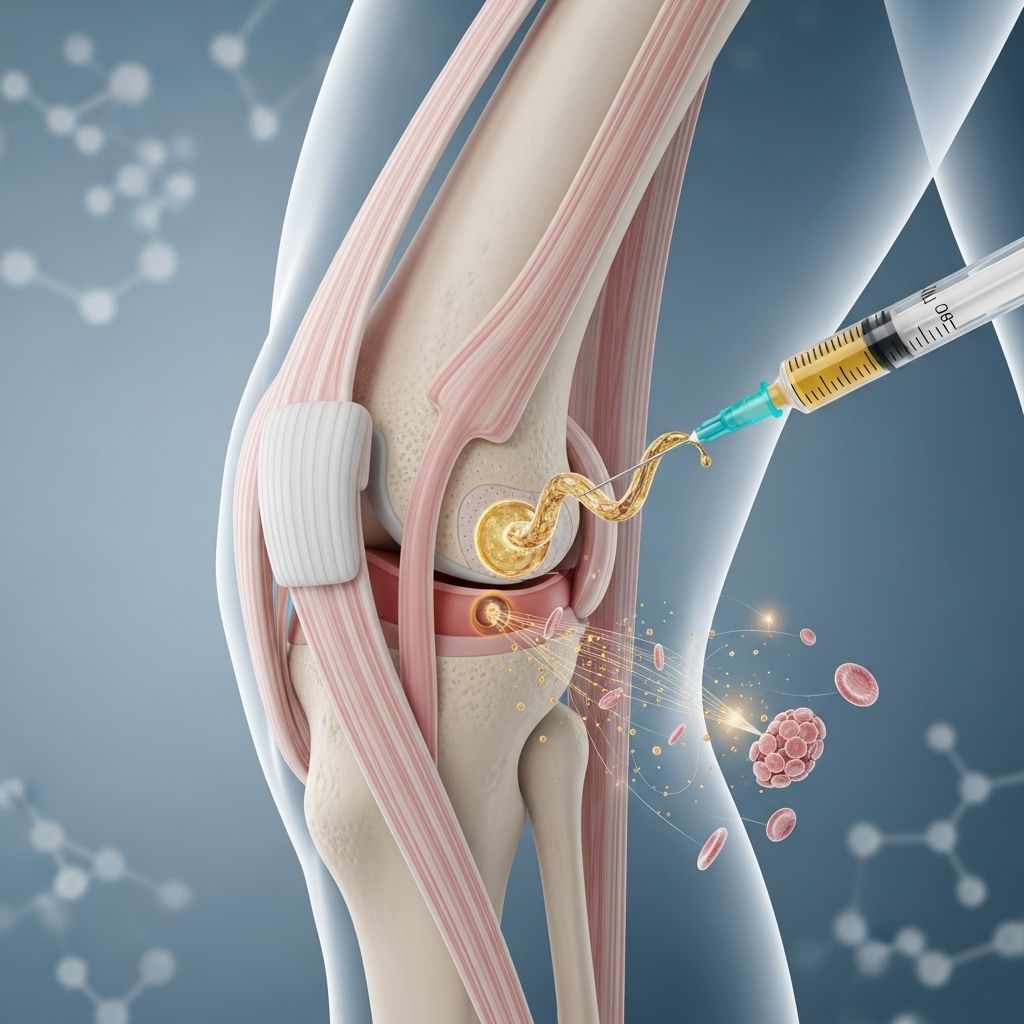
Platelet-rich plasma (PRP) injections represent a cutting-edge technique in regenerative medicine, designed to harness the body’s innate healing powers to treat musculoskeletal injuries, chronic pain, and degenerative conditions. Utilizing concentrated platelets from the patient’s own blood, PRP injections offer a personalized, safe, and minimally invasive therapy that can accelerate tissue repair and modulate inflammation.
This article explores the fundamentals of PRP therapy, its medical applications, procedure details, benefits, risks, and frequently asked questions. The content reflects the comprehensive approach and structure found in leading musculoskeletal centers.
What Is Platelet-Rich Plasma (PRP)?
Platelet-rich plasma is a derivative of human blood, concentrated to contain a higher-than-normal number of platelets and growth factors. Platelets are tiny blood cells that play an essential role in both blood clotting and tissue healing.
Plasma is the liquid component of blood, providing a medium for all blood cells, nutrients, hormones, and proteins. In PRP formulations, the platelets are suspended within plasma to promote a potent healing effect when re-injected into the body.
The preparation process removes most red and white blood cells, leaving a platelets-rich solution that can target damaged or diseased tissues for accelerated repair.
How Are PRP Injections Prepared and Administered?
The PRP injection procedure involves several key steps:
- Blood Draw: The patient undergoes a standard blood draw, typically 10–60 milliliters depending on the target area and volume needed.
- Centrifugation: The blood sample is processed in a centrifuge, which rapidly spins to separate components by density. Platelets are isolated from red blood cells, white blood cells, and plasma.
- Preparation of PRP: Platelets are concentrated to 2–8 times their usual level, suspended in a small volume of plasma. The specific formulation may vary, such as leukocyte-rich (containing white blood cells) or leukocyte-poor PRP, each offering different inflammatory profiles.
Specialized PRP methods may further concentrate anti-inflammatory growth factors like IL-1ra (interleukin-1 receptor antagonist) or a2M (alpha-2-Macroglobulin), enhancing the injection’s healing focus.
- Precise Injection: The PRP solution is injected directly into the targeted joint, tendon, ligament, or muscle using sterile technique. Ultrasound guidance is often used to improve accuracy and ensure delivery into affected tissue.
Mechanism of Action: How PRP Works
PRP’s therapeutic benefits stem from its high concentration of growth factors and bioactive proteins that activate cellular repair pathways. Key mechanisms include:
- Stimulation of Cellular Regeneration: Released growth factors promote recruitment and activation of reparative cells, stimulating tissue renewal and matrix formation.
- Modulation of Inflammation: By altering inflammatory signaling, PRP can decrease pain and swelling or, in certain formulations, increase inflammation for chronic conditions to boost healing response.
- Promotion of Angiogenesis: Growth factors encourage new blood vessel formation, enhancing oxygen and nutrient supply essential for tissue recovery.
- Reduction of Scar Formation: PRP may limit development of excess scar tissue, supporting more functional healing in musculoskeletal injuries.
Medical Uses of PRP Therapy
PRP injections have gained acceptance for treating a spectrum of conditions, notably within musculoskeletal medicine:
- Tendon Injuries: Commonly used for chronic tendon disorders (tendinopathies) such as tennis elbow, jumper’s knee, and Achilles tendonitis, PRP accelerates soft tissue healing and function restoration.
- Ligament and Muscle Injuries: PRP may enhance healing in ligamentous strains, partial tears, and muscle injuries, contributing to improved outcomes and recovery time.
- Osteoarthritis: Intra-articular PRP injections for knee, hip, and other joints can decrease pain and inflammation associated with arthritis, promote cartilage health, and support functional improvement.
- Postoperative Recovery: PRP therapy is used adjunctively to promote faster healing and decrease pain after orthopedic surgery.
- Other Applications: Emerging evidence supports PRP in treating skin conditions, stimulating hair growth (alopecia), and cosmetic enhancement, though musculoskeletal indications remain most established.
Key Benefits of Platelet-Rich Plasma Injections
PRP therapy offers several important advantages:
- Enhanced Tissue Healing: PRP stimulates and sustains robust tissue regeneration for faster and more complete recovery compared to conventional methods.
- Reduced Inflammation: Certain PRP formulations can limit inflammatory signaling, alleviating swelling and discomfort, especially in arthritis and tendinopathies.
- Minimally-Invasive Procedure: Using the patient’s own blood greatly limits allergenic risk or tissue rejection, and PRP injections are performed as outpatient procedures under local anesthesia.
- Opioid-sparing Effect: PRP may lower dependence on pain medications, including opioids and oral anti-inflammatories. Patients are typically advised to stop NSAID use before and after PRP injections for maximal benefit.
- Regenerative Rather Than Symptomatic: Unlike many interventions, PRP targets the root cause by enhancing biological repair, rather than simply masking symptoms.
Conditions Treated with PRP Injections
PRP is applied across a variety of musculoskeletal and other medical problems. Common indications include:
| Condition | Benefit of PRP Injection |
|---|---|
| Tendon Injuries (e.g., tennis elbow) | Accelerated healing, reduced pain and improved function |
| Ligament Damage | Regeneration and strengthening of ligament tissue |
| Osteoarthritis (knee, hip, shoulder) | Alleviates pain, slows cartilage deterioration, improves mobility |
| Muscle Injuries | Promotes muscle regeneration, restores strength |
| Chronic Inflammatory Conditions | Limits harmful inflammation, supports long-term joint health |
| Skin and Hair Loss | Stimulates repair and growth, improves cosmetic appearance |
Treatment Steps: What Patients Can Expect
- Consultation and Assessment: Healthcare providers evaluate the patient’s medical history, current condition, previous treatments, and eligibility for PRP.
- Blood Collection: A sterile blood draw is performed in-office.
- Processing: The sample is centrifuged to isolate and concentrate platelets.
- Injection: PRP is delivered to the targeted site, often under ultrasound guidance; treatment is usually completed in under an hour.
- Post-Injection Instructions: Patients may be advised to rest the treated area briefly and avoid anti-inflammatory medications; typical post-procedure discomfort is mild to moderate and transient.
- Follow-Up: Periodic evaluation is performed to assess response, and repeat injections may be scheduled if indicated.
Safety, Risks, and Recovery
PRP injections are considered highly safe, utilizing autologous (your own) blood elements. Common minor side effects may include:
- Localized pain or soreness at the injection site (usually resolves in hours to days)
- Mild swelling or bruising
- Risk of infection (rare due to sterile technique)
- Temporary increase in discomfort reflecting a healing response
Serious complications are rare. Because PRP leverages the body’s own blood, risks of allergic reaction or immune rejection are virtually eliminated.
Patients are typically able to resume light activities within 24–48 hours and gradually return to full function, often with a “rest and gradual rehab” protocol post-injection. Recovery time varies based on the injury and individual response. Full effects may be seen within several weeks, with improvements in pain and function continuing for months.
PRP vs. Traditional Treatments
| Aspect | PRP Injections | Traditional Therapies |
|---|---|---|
| Source | Autologous blood product | Medications, surgery, physical therapy |
| Healing Approach | Regenerative, biological stimulation | Symptomatic, mechanical or pharmaceutical |
| Risks | Low – personalized and biocompatible | Variable – may include systemic side effects |
| Procedure | Minimally invasive injection | May require surgery or prolonged medication |
| Effectiveness | Accelerates healing; may reduce pain and inflammation | Depends on treatment, may not address underlying tissue regeneration |
Frequently Asked Questions (FAQs)
What types of conditions are best treated with PRP?
PRP is most effective for chronic tendon injuries, mild to moderate osteoarthritis, ligament sprains, and muscle tears. Certain skin and cosmetic indications are also emerging.
Is PRP safe?
Yes. PRP is safe and associated with a very low risk of infection or allergic reaction, as it uses the patient’s own blood. Standard protocol reduces complications. Mild pain or swelling is expected temporarily.
How many PRP injections will I need?
The number of injections varies by condition and individual response. Some injuries require one session, while others may benefit from a series spaced weeks apart.
Can I take painkillers with PRP treatments?
Patients are typically asked to avoid anti-inflammatory medications (NSAIDs) before and after PRP to support optimal healing. Non-NSAID pain relief and ice may be allowed by your medical team.
How quickly does PRP work?
Some patients report improvement within a few days; most see increased healing, decreased pain, and improved function after several weeks, with ongoing benefit continuing for months.
Are PRP injections covered by insurance?
Coverage varies by provider and region. Many insurers consider PRP investigational for some uses, so patients should check with their medical and insurance teams.
How does PRP differ from cortisone injections?
Cortisone injections primarily reduce inflammation and pain temporarily, while PRP aims to regenerate and heal tissues for long-term improvement. PRP has no risk of tissue atrophy associated with repeated cortisone use.
Conclusion
Platelet-rich plasma (PRP) injections are an advanced, evidence-based therapy at the forefront of musculoskeletal medicine. By utilizing the body’s own biological factors, PRP promotes healing, reduces pain, and restores function with minimal risk. As research advances, PRP is increasingly applied in diverse areas, offering hope to those with persistent injuries or degenerative conditions.
Consult with a musculoskeletal specialist to determine whether PRP therapy fits your individualized treatment plan, and take a step toward natural, regenerative healing.
References
- https://www.uchealth.org/treatments-procedures/platelet-rich-plasma-prp-therapy/
- https://www.hss.edu/health-library/conditions-and-treatments/list/prp-injections
- https://my.clevelandclinic.org/health/treatments/platelet-rich-plasma-prp-injection
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6030616/
- https://www.bswhealth.com/treatments-and-procedures/platelet-rich-plasma-therapy
- https://www.painmedicineconsultants.com/blog/the-10-benefits-of-platelet-rich-plasma-prp-therapy
- https://www.nyp.org/orthopedics/prp-injections
Read full bio of Sneha Tete












