Plasma Cell Leukemia: Causes, Symptoms, and Treatment Options
Comprehensive guide on plasma cell leukemia, its causes, symptoms, diagnostic steps, treatment regimens, and what to expect for patients and caregivers.
Plasma Cell Leukemia: Causes, Symptoms, Diagnosis, and Treatments
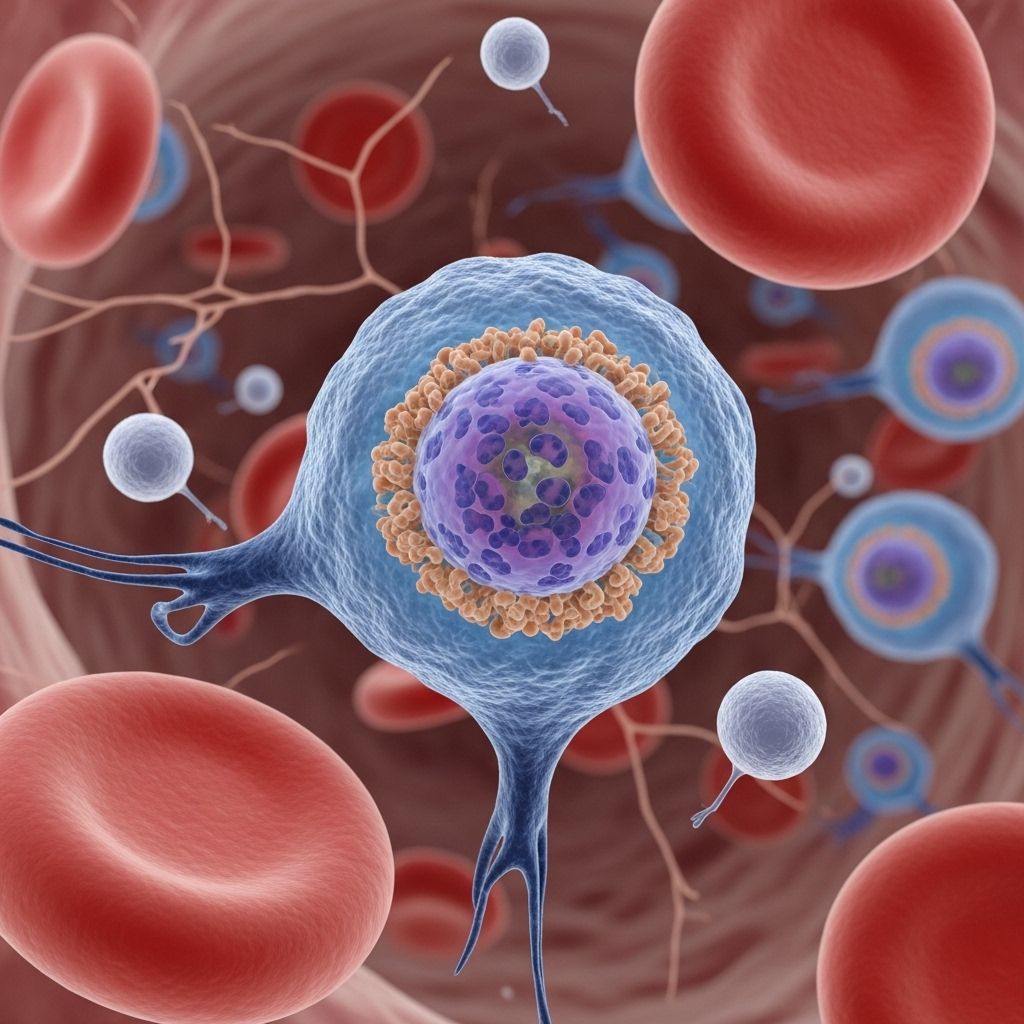
Plasma cell leukemia (PCL) is a rare and aggressive form of blood cancer that develops from abnormal plasma cells. These cells, which normally help the immune system by producing antibodies, become cancerous and multiply uncontrollably in PCL, circulating in the blood as well as residing in the bone marrow. Understanding PCL1s causes, symptoms, diagnosis, and treatment options is vital for patients and caregivers facing this serious condition.
What Is Plasma Cell Leukemia?
Plasma cell leukemia is an unusual type of leukemia distinguished by the excessive proliferation of malignant plasma cells in the blood. While related to multiple myeloma, PCL is more aggressive, progresses faster, and often presents with more severe symptoms. There are two primary types:
- Primary PCL: Develops as a standalone condition without previous multiple myeloma.
- Secondary PCL: Occurs as a transformation from advanced or treated multiple myeloma, often indicating disease progression.
PCL comprises less than 5% of all plasma cell cancers. Its rapid progression makes prompt diagnosis and treatment essential for better outcomes.
Causes and Risk Factors
The precise causes of plasma cell leukemia remain unclear. However, genetic changes within plasma cells often play a vital role. Some relevant risk factors include:
- History of multiple myeloma (for secondary PCL)
- Older age (most cases occur in people over 60)
- Genetic predispositions or family history, though rare
- Possible links to chemical or radiation exposure, though not well-established
For many, no clear risk factors are identified, and the disease may arise unexpectedly.
Types of Plasma Cell Leukemia
| Type | Description |
|---|---|
| Primary PCL | Develops de novo, or without prior multiple myeloma diagnosis; generally presents more acutely. |
| Secondary PCL | Evolves from pre-existing or relapsed multiple myeloma; tends to appear in later stages of disease and has an even poorer prognosis. |
Common Symptoms and Complications
The symptoms of plasma cell leukemia usually develop rapidly and are typically more severe than those found in multiple myeloma. Common symptoms and complications include:
- Anemia, leading to fatigue and weakness
- Bone pain (often in the spine, hips, or ribs; related to bone lesions)
- Frequent infections, as the immune system becomes compromised
- Abnormal bleeding or bruising, due to low platelet counts
- Unintended weight loss and appetite loss
- Swollen lymph nodes, liver, or spleen
- Hypercalcemia: High calcium levels in blood causing nausea, vomiting, constipation, confusion, and weakness
- Renal (kidney) impairment
- Numbness or weakness in limbs (if spinal cord or nerves are affected)
The severity of each symptom can vary, but many people experience multiple complications at diagnosis.
How Is Plasma Cell Leukemia Diagnosed?
Diagnosis of PCL is often based on both clinical evaluation and laboratory findings. Typical diagnostic steps include:
- Complete Blood Count (CBC): Looks for abnormal levels of red/white blood cells and platelets.
- Peripheral Blood Smear: Microscopically identifies abnormal plasma cells circulating in the blood.
- Bone Marrow Biopsy: Determines the number and characteristics of plasma cells in bone marrow.
- Blood and Urine Protein Electrophoresis (SPEP/UPEP): Detects abnormal monoclonal proteins (M-proteins).
- Imaging (X-ray, MRI, CT): Checks for bone lesions, fractures, or soft tissue involvement.
Diagnostic criteria: PCL is confirmed if one or both of the following are found:
- Over 2,000 abnormal plasma cells per microliter (μL) of blood, or
- Abnormal plasma cells constitute >20% of total white blood cells in peripheral blood
How Is Plasma Cell Leukemia Treated?
The main goal in treating PCL is to rapidly reduce the number of plasma cells in the blood and bone marrow, aiming for remission and improved quality of life. Due to PCL’s aggressiveness, treatment typically begins immediately. Therapeutic strategies include:
1. Induction Therapy
- Targeted therapies: Drugs such as bortezomib (Velcade), lenalidomide (Revlimid), and thalidomide are commonly used as first-line agents.
- Chemotherapy: Combinations with drugs like cyclophosphamide, doxorubicin, or dexamethasone may be given.
- Proteasome inhibitors: Including bortezomib 1 help disrupt cancerous cell function.
2. Stem Cell Transplantation
- Autologous stem cell transplant: Uses patient1s own stem cells. It is suitable for younger, fitter patients and typically follows initial induction therapy.
- Allogeneic stem cell transplant: Uses stem cells from a donor, occasionally considered for suitable high-risk patients, but with higher risks.
3. Supportive Treatments
- Pain management, including analgesics for bone pain
- Blood transfusions for severe anemia or thrombocytopenia
- Antibiotics to prevent or manage infections
- Bisphosphonates for bone strengthening
- Dialysis or other management for kidney failure when needed
4. Emerging and Targeted Therapies
- Newer treatments under research include monoclonal antibodies, CAR T-cell therapies, immunotherapies and drugs targeting specific plasma cell mutations.
The choice of therapy depends on disease severity, prior treatments (if secondary PCL), patient age, and overall health.
What Is the Prognosis for Plasma Cell Leukemia?
PCL has a poorer outlook compared to most other blood cancers due to its rapid progression and resistance to standard treatments. Key points on prognosis:
- Median survival for primary PCL ranges between 7 to 11 months, even with therapy.
- Survival may drop to 2 to 7 months in cases of secondary PCL.
- Early and aggressive treatment improves outcomes, though cures are very rare.
- Newer therapies and transplants may extend survival for some patients.
Living with Plasma Cell Leukemia
Dealing with a PCL diagnosis can be overwhelming. Patients and families are encouraged to:
- Seek multidisciplinary care: Hematologists, oncologists, kidney and pain specialists, social workers, and nurses may all be involved in your team.
- Monitor for infections and symptoms: Promptly report new fevers, pain, or unusual symptoms to your care team.
- Consider clinical trials: Participation may provide access to novel treatments and closer monitoring.
- Utilize support resources: Patient advocacy groups and counseling can help manage the emotional impacts of living with cancer.
Frequently Asked Questions (FAQs)
What is the difference between plasma cell leukemia and multiple myeloma?
Both diseases involve malignant plasma cells but PCL is more aggressive, features a higher proportion of abnormal plasma cells in the blood, and progresses more quickly. PCL can occur on its own (primary) or evolve from myeloma (secondary).
Is plasma cell leukemia curable?
Cure is currently not possible for most people with PCL, but aggressive treatment and, when possible, stem cell transplantation may lead to remission and extend survival.
Who is most at risk for plasma cell leukemia?
PCL is very rare and typically affects adults over the age of 60. Secondary PCL develops in people with known multiple myeloma.
What supportive care options exist?
Pain management, antibiotics, blood transfusions, kidney support, and emotional support all play essential roles alongside antileukemic treatment.
Are there experimental therapies available?
Yes, clinical trials are exploring new immunotherapies, monoclonal antibodies, and other precision medicine approaches. Discuss options with your healthcare team.
When to See a Doctor
See a doctor right away if you experience persistent or worsening fatigue, unexplained bruising or bleeding, frequent infections, severe bone pain, mental confusion, or other symptoms listed above1especially if there is a personal or family history of blood cancers.
Resources and Support
- Hematology/Oncology clinics: For specialized care
- Patient advocacy and support groups: Offer information and emotional support (such as the Leukemia & Lymphoma Society, Myeloma UK, International Myeloma Foundation)
- Counseling and mental health support: Can help patients and families cope with anxiety and depression during treatment
Staying informed and accessing comprehensive medical and psychosocial support can help improve quality of life for people living with plasma cell leukemia.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3907188/
- https://www.myeloma.org.uk/understanding-myeloma/related-conditions/plasma-cell-leukaemia/
- https://www.oncologyradiotherapy.com/articles/plasma-cell-leukemia-clinical-manifestations-and-management.pdf
- https://www.patientpower.info/leukemia/plasma-cell-leukemia
- https://www.healthline.com/health/leukemia/plasma-cell-leukemia
- https://my.clevelandclinic.org/health/diseases/plasma-cell-leukemia
- https://www.mayoclinic.org/diseases-conditions/multiple-myeloma/symptoms-causes/syc-20353378
- https://www.cancer.gov/types/myeloma/patient/myeloma-treatment-pdq
- https://www.myeloma.org/resource-library/primary-plasma-cell-leukemia-consensus-definition-international-myeloma-working
Read full bio of medha deb












