Phases of Acute Renal Failure: Stages, Symptoms, and Treatment
Comprehensive guide to acute renal failure types, stages, symptoms, diagnosis, and treatment for improved kidney health.
Acute renal failure (ARF), now commonly known as acute kidney injury (AKI), is a serious condition where the kidneys lose their ability to filter waste and maintain fluid, electrolyte, and acid-base balance—often very suddenly. This article explores the types, symptoms, diagnostic processes, stages, and evidence-based treatment strategies associated with acute renal failure, providing a thorough roadmap for patients, caregivers, and healthcare professionals navigating this potentially life-threatening disorder.
Understanding Acute Renal Failure
Acute renal failure is a rapid loss of kidney function, typically developing over hours to days. The kidneys, normally responsible for filtering blood and eliminating waste as urine, struggle to complete these vital tasks. Without prompt intervention, ARF can lead to accumulation of harmful wastes, disturbance in chemical balance, and in severe cases, organ dysfunction or death. ARF is most often reversible—especially when recognized early and managed appropriately—but it demands immediate medical attention.
The Three Types of Acute Renal Failure
The underlying causes of ARF are categorized into three types, each with distinct precipitating factors and clinical implications:
- Pre-renal ARF: Results from conditions that decrease blood flow to the kidneys.
- Intrinsic (Renal) ARF: Direct damage to the kidney tissue itself impairs function.
- Post-renal ARF: Occurs when injury is due to obstruction or blockage beyond the kidneys, inhibiting urine excretion.
1. Pre-renal ARF
Pre-renal ARF accounts for about 60% of ARF cases. In this form, the kidneys themselves are initially undamaged, but a reduction in overall blood flow prevents normal filtration, potentially leading to kidney injury if not promptly corrected.
Major causes include:
- Low blood volume (hypovolemia) due to severe bleeding, burns, or fluid loss from vomiting or diarrhea.
- Low blood pressure (hypotension) from heart attack, heart failure, liver failure, severe allergic reactions (anaphylaxis), septic shock, or certain medications (e.g., blood pressure drugs, NSAIDs, cyclosporine, anesthesia).
- Vascular problems such as a pulmonary embolism (blood clot in the lungs).
Timely correction of the underlying issue (restoring blood volume or pressure) is often sufficient to reverse pre-renal ARF if implemented before permanent kidney injury develops.
2. Intrinsic (Renal) ARF
Intrinsic ARF (also called renal or intrarenal ARF) stems from direct injury or disease affecting the kidney tissue itself. This injury disrupts the normal architecture of the kidney’s filtering units (glomeruli, tubules, interstitial tissue, or blood vessels).
Common causes include:
- Acute tubular necrosis (ATN): Often precipitated by ischemia (prolonged lack of blood flow), sepsis, toxins (drugs, heavy metals), or severe untreated pre-renal ARF.
- Glomerulonephritis: Inflammation of the glomeruli following infections or autoimmune diseases.
- Interstitial nephritis: Allergic reactions to medications (antibiotics, NSAIDs, etc.), infections.
- Vascular injury: Disorders affecting the small blood vessels of the kidney (vasculitis, malignant hypertension).
Intrinsic ARF often takes longer to resolve and may require more intensive intervention than pre-renal ARF.
3. Post-renal ARF
Post-renal ARF arises from obstruction or blockage beyond the kidneys, preventing urine from leaving the body. Backpressure damages nephrons and impairs filtration.
Typical causes:
- Obstructive uropathy: Kidney stones, enlarged prostate (BPH), ureteral strictures, tumors, or blood clots in the urinary tract.
Relieving the obstruction promptly can restore normal kidney function, especially if permanent damage has not occurred.
Symptoms of Acute Renal Failure
The presentation of acute renal failure depends on the underlying cause, the rapidity of onset, and the severity. Many patients show no symptoms in the earliest stages, while others may display several warning signs as kidney function declines.
- Decreased urine output (oliguria) or total absence of urine (anuria)
- Edema (swelling of legs, ankles, or face) due to fluid retention
- Fatigue, drowsiness, or weakness
- Nausea and vomiting
- Shortness of breath
- High blood pressure (hypertension)
- Irregular heartbeat (arrhythmia) or chest pain/pressure in severe cases
- Confusion or altered mental state
Symptoms may escalate rapidly, especially if ARF develops acutely. Patients should seek medical attention promptly if these warning signs occur, especially in high-risk individuals.
How Acute Renal Failure is Diagnosed
Swift, accurate diagnosis is essential to initiate therapy and improve outcomes in ARF. Evaluation generally involves a combination of the following:
- Medical History & Physical Exam: Assessment for underlying diseases, recent events (bleeding, dehydration, infections), symptoms, and medications.
- Laboratory Tests: Measurement of serum creatinine (indicator of kidney filtration), blood urea nitrogen (BUN), electrolyte levels, and complete blood count.
- Urinalysis: Checks for protein, blood, casts, and other abnormal findings in the urine.
- Imaging Studies: Ultrasound or CT scan can identify structural abnormalities, blockages, kidney size, and more.
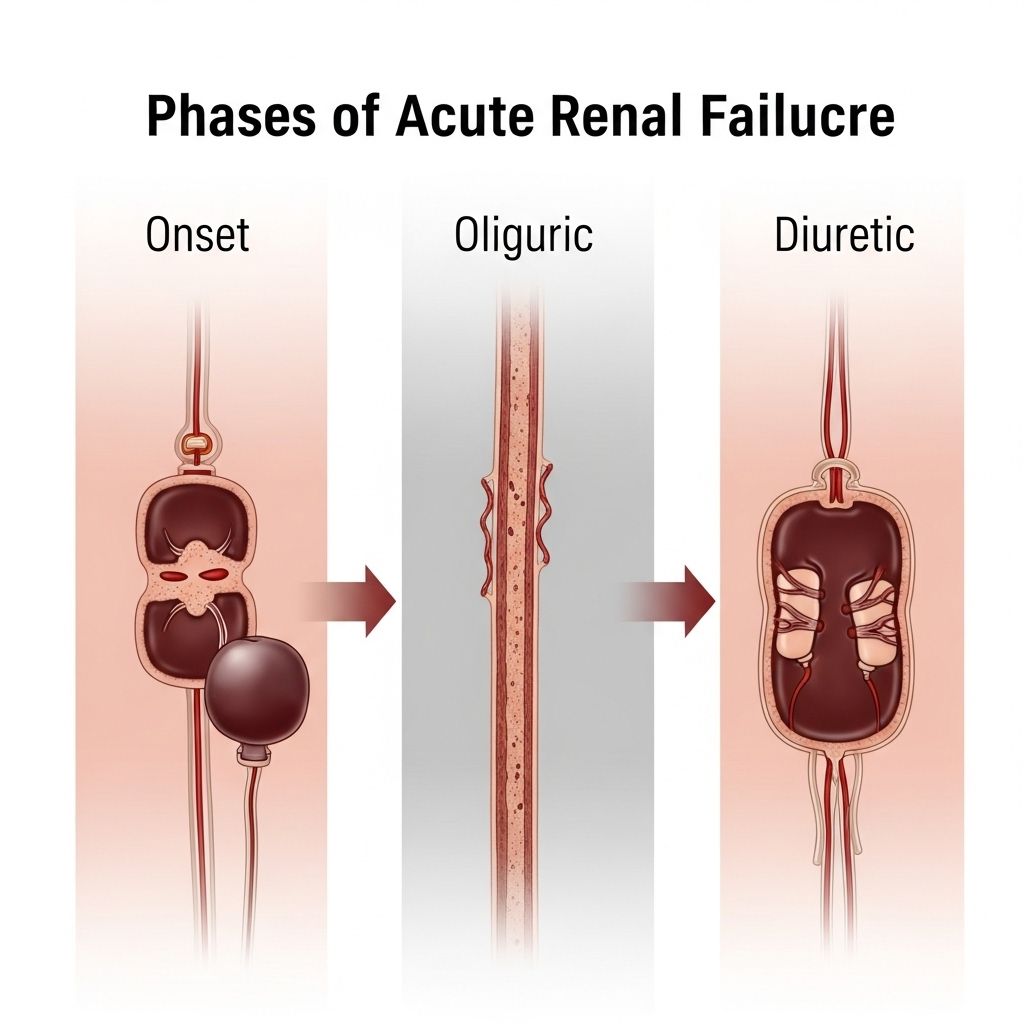
Stages of Acute Renal Failure
Doctors use well-established criteria to stage the severity of ARF. The KDIGO (Kidney Disease: Improving Global Outcomes) and AKIN (Acute Kidney Injury Network) staging systems are commonly used, based on serum creatinine increases and urine output declines. Staging helps guide treatment and predict prognosis.
| Stage | Serum Creatinine | Urine Output |
|---|---|---|
| Stage 1 | Increase by ≥0.3 mg/dL within 48h OR 1.5–1.9 × baseline | <0.5 mL/kg/h for 6–12 h |
| Stage 2 | 2.0–2.9 × baseline | <0.5 mL/kg/h for ≥12 h |
| Stage 3 | 3.0 × baseline OR ≥4.0 mg/dL OR dialysis required | <0.3 mL/kg/h for ≥24 h OR anuria for ≥12 h |
Stage Details
- Stage 1: Early kidney injury, often with minimal symptoms. May be detected through routine labs.
- Stage 2: Moderate injury with more pronounced decrease in kidney function and urine output.
- Stage 3: Severe kidney failure, possibly requiring dialysis or resulting in dangerously low or absent urine output.
Treatment Options for Acute Renal Failure
Underlying cause, stage, and overall health dictate appropriate management strategies. Key treatment goals include:
- Restoring normal blood volume and pressure
- Correcting electrolyte, acid-base, and fluid imbalances
- Treating the underlying disease or injury (such as removing a blockage or stopping harmful medications)
- Providing supportive care, including nutritional support and monitoring for complications
Common Approaches
- Medications: Adjust or discontinue nephrotoxic drugs; treat infections promptly with appropriate antibiotics; use diuretics judiciously if needed to manage fluid status.
- Fluid Management: Administer IV fluids in cases of dehydration; restrict fluids if fluid overload is present.
- Correction of Electrolytes: Severe potassium or acid-base disturbances may require urgent therapy (such as Kayexalate for hyperkalemia, bicarbonate for acidosis).
- Dialysis: Initiated when critical markers indicate life-threatening derangements or if kidney function does not recover rapidly. Dialysis acts as an artificial filter to remove toxins and excess fluid.
- Treating Obstructions: Procedures such as catheterization, stent placement, or surgical intervention may be needed for post-renal ARF.
Long-Term Outlook
Many people recover full or partial kidney function when ARF is identified and managed early. In others, especially those with pre-existing kidney disease or severe underlying illness, ARF can progress to chronic kidney disease (CKD) or end-stage renal disease (ESRD), and require ongoing dialysis.
- Mortality rates are substantially higher in those with severe or prolonged ARF, older age, or significant comorbidities.
- Early and aggressive management significantly improves the chances of recovery and survival.
Frequently Asked Questions (FAQs)
What are the warning signs of acute renal failure?
Look for decreased urine output, marked swelling, fatigue, nausea, confusion, and, in severe cases, chest discomfort or shortness of breath. Many cases present with subtle or no early symptoms—especially in hospitalized or critically ill patients.
How is ARF different from chronic kidney disease?
ARF or AKI develops suddenly, usually within days, and may be reversible if treated early. Chronic kidney disease evolves over months or years and is generally permanent and progressive.
What increases the risk for ARF?
Major risk factors include advanced age, recent illness or surgery, severe infections, use of certain medications (like NSAIDs, ACE inhibitors, contrast dyes), heart or liver failure, dehydration, and pre-existing kidney disease.
Can acute renal failure be prevented?
While not all cases are preventable, addressing dehydration promptly, avoiding unnecessary nephrotoxic medications, managing chronic health conditions, and treating infections early can all help reduce the risk.
What is the prognosis for someone with ARF?
With timely intervention, many individuals recover fully. However, the risk of complications or progression to chronic kidney disease is higher in those with more severe or prolonged ARF, older adults, and those with other serious illnesses.
Key Takeaways
- Acute renal failure is a serious but potentially reversible loss of kidney function, requiring prompt diagnosis and intervention.
- The three main types—pre-renal, intrinsic, and post-renal ARF—differ in their causes and management strategies.
- Symptoms can be subtle, underscoring the importance of routine monitoring for kidney function in high-risk settings.
- Accurate staging using the KDIGO or AKIN criteria guides treatment and helps predict outcomes.
- Early, aggressive support maximizes recovery, minimizes complications, and improves overall outcomes.
References
- https://www.healthline.com/health/kidney-disease/phases-of-acute-renal-failure
- https://www.medicalnewstoday.com/articles/types-of-renal-failure
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3134724/
- https://www.healthline.com/health/kidney-disease/oliguric-phase-of-acute-renal-failure
- https://www.healthline.com/health/video/ckd-stages
- https://www.medicalnewstoday.com/articles/327300
- https://www.ncbi.nlm.nih.gov/books/NBK441896/
- https://my.clevelandclinic.org/health/diseases/17689-kidney-failure
- https://www.kidney.org/kidney-topics/acute-kidney-injury-aki
- https://www.aafp.org/pubs/afp/issues/2019/1201/p687.html
Read full bio of medha deb












