Phalloplasty for Gender Affirmation: Process, Techniques, and Recovery
A comprehensive guide to gender-affirming phalloplasty, including surgical techniques, preparation, risks, recovery, and frequently asked questions.
Phalloplasty for Gender Affirmation
Phalloplasty is a multi-stage gender-affirming surgical procedure designed to construct a penis for transgender men and non-binary individuals assigned female at birth. The operation aims to help individuals live authentically by aligning their physical anatomy with their gender identity, supporting improved psychological wellbeing and overall quality of life.
What Is Phalloplasty?
Phalloplasty reconstructs the penis using tissue harvested from donor sites such as the forearm, thigh, or abdomen. Key objectives include:
- Creation of an aesthetically proportioned phallus
- Ability to void urine while standing
- Construction of a functional scrotum
- Potential for penetrative intercourse
- Provision of tactile and erogenous sensation via nerve repair
The surgery is typically performed by a multidisciplinary team of plastic surgeons, urologists, and, when necessary, gynecologists. Phalloplasty is often accompanied by other procedures such as vaginectomy (removal of the vaginal cavity), scrotoplasty (scrotum creation), and placement of prosthetics for testicles and, optionally, the penis itself.
History and Evolution of Phalloplasty
The field of phalloplasty has evolved greatly over the past century:
- 1936: The first documented phalloplasty by Nikolaj Bogoraz, performed for traumatic amputation using abdominal tissue and rib cartilage grafts.
- 1946: Sir Harold Gilles completed the first gender-affirming phalloplasty for a transgender man, involving 13 operations over four years and abdominal skin for urethral reconstruction.
- 1984: Chang and Hwang introduced the radial forearm free flap (RFFF) ‘tube-within-a-tube’ technique.
- 1993: Gottlieb and Levine refined RFFF for improved vascularity and a more centralized urethra.
Advancements in microsurgical techniques have dramatically increased the safety and efficacy of phalloplasty, allowing more personalized care and increased patient satisfaction.
Surgical Techniques in Phalloplasty
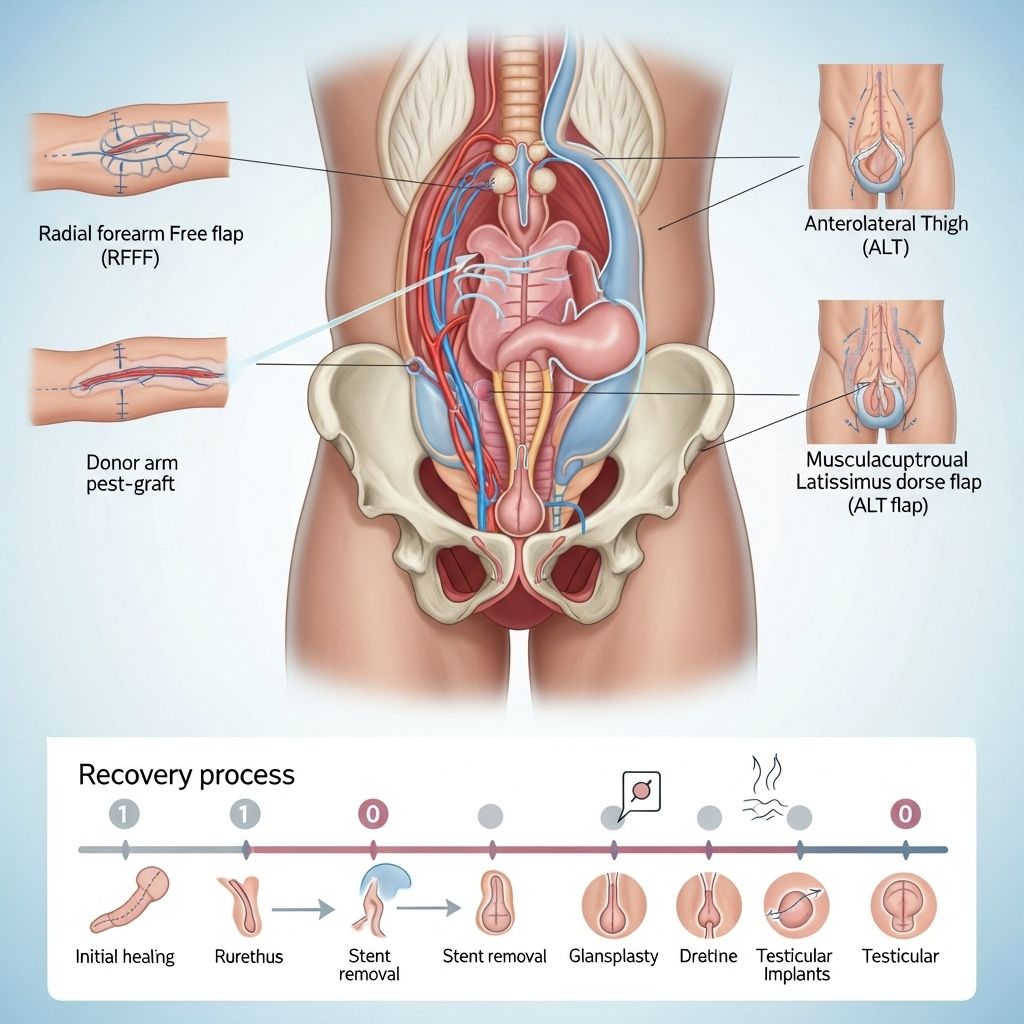
Phalloplasty is complex and highly individualized, with the choice of technique depending on patient anatomy, preferences, and surgeon expertise. Surgical options include:
- Free Flap Phalloplasty: Tissue, including skin, fat, and sometimes nerves, is fully detached and transplanted from a donor site (commonly the forearm) for penis construction.
- Pedicled Flap Phalloplasty: Tissue is moved from a nearby site (such as the thigh, groin, or abdomen) and continues to receive blood supply from its original location until vascular integration is complete.
The most common donor sites are:
- Radial forearm (RFFF)
- Anterolateral thigh
- Latissimus dorsi (from the back)
Each donor site has implications for cosmetic outcomes, sensation, and potential complications at both the donor and recipient sites. The specific flap is selected based on individualized factors, including the degree of available tissue and healing potential.
| Donor Site | Benefits | Considerations |
|---|---|---|
| Radial Forearm | High sensation potential, reliable blood supply | Visible arm scar, need for hair removal, risk of functional impact |
| Anterolateral Thigh | Larger tissue bulk, less visible scar | Less sensation, possibly less natural appearance |
| Latissimus Dorsi | Good tissue volume, suitable for larger phallus | Back scar, complex nerve connection for sensation |
Step-by-Step Overview
- Tissue Harvest: Flaps are raised from the chosen donor site (often the forearm), with vessels and nerves carefully isolated for reconnection.
- Shaping and Construction: Tissue is sculpted into a neopenis using techniques like ‘tube-within-a-tube’ for shaft and urethra creation.
- Urethral Lengthening: Tissue from the vaginal wall and labia minora can be used to extend the urethra, enabling voiding from the tip.
- Scrotoplasty: Labia majora are repositioned and joined to create a scrotum, often with silicone testicular implants inserted during one of the stages.
- Sensation Restoration: Microsurgical nerve connections provide tactile and sometimes erogenous sensation.
Additional procedures such as glansplasty (the creation of the glans penis) and vaginectomy (closure or removal of the vaginal cavity) may be conducted in parallel or as staged operations.
Preparation for Phalloplasty Surgery
Thorough preparation is crucial for optimal outcomes. Key preoperative steps include:
- Medical Evaluation: Comprehensive health assessment and review of medical history to identify surgical risks and suitability.
- Hormone Therapy: Testosterone therapy to promote clitoral growth, supporting metoidioplasty or urethral construction.
- Blood Tests: Conducted at least three months prior to surgery to ensure overall health readiness.
- Nutrition and Hygiene: Maintaining a balanced diet and good intestinal health pre-surgery.
- Forearm Hair Removal: Laser hair reduction (if forearm flap is chosen) minimizes post-surgical hair growth within the neourethra.
- Mental Health Support: Counseling and support to address psychological needs and manage expectations.
Patients are encouraged to discuss goals, expectations, and potential outcomes in detail with their surgical team. Informed consent and shared decision-making are fundamental for patient-centered care.
Associated Procedures and Stages in Phalloplasty
Phalloplasty commonly involves a series of procedures over several months or years, tailored to each patient:
- Metoidioplasty: A masculinizing genital procedure using clitoral growth from testosterone therapy to create a small penis, often coupled with urethral lengthening and scrotoplasty.
- Vaginectomy: Closure or removal of the vaginal cavity, sometimes performed before or during phalloplasty.
- Testicular Prosthesis Placement: Silicone or saline testicles are placed in the newly constructed scrotum, staged as needed.
- Penile Prosthesis: Inflatable or rigid penile implants may be considered after healing, allowing for penetrative sexual activity.
The approach, number of stages, and timing of additional interventions depend on individual anatomy, healing rates, and patient desires.
Risks and Potential Complications
While phalloplasty is generally safe and associated with high patient satisfaction, risks and complications may arise:
- Flap-Related Issues: Healing compromise, infection, or necrosis at the donor or recipient site.
- Urethral Complications: Stricture (narrowing) or fistula (abnormal connection) leading to urinary problems.
- Scarring and Sensation Changes: Decreased sensation and prominent scarring at donor or recipient sites.
- Delayed Healing: Prolonged recovery or need for revision surgeries.
- Prosthesis Migration or Failure: Displacement or malfunction of implanted devices.
Management of complications often involves additional surgical interventions and multidisciplinary follow-up.
Recovery and Postoperative Care
Recovery from phalloplasty is a gradual process requiring careful monitoring and support:
- Hospital Stay: Patients typically stay in the hospital for several days to monitor healing, pain control, and wound care.
- Follow-Up Visits: Regular check-ups with surgeons, urologists, and allied health professionals to assess tissue healing and manage complications.
- Physical Activity Restrictions: Rest and avoidance of strenuous activity are required for initial weeks.
- Long-Term Rehabilitation: May include pelvic floor exercises, physiotherapy, and ongoing psychological support.
Most patients report improved self-esteem and quality of life after surgery, although recovery times vary and revision procedures may be necessary.
Expected Outcomes and Patient Satisfaction
Phalloplasty offers tangible benefits for many transgender men and non-binary individuals:
- Improved Gender Congruence
- Increased confidence in daily life
- Ability to void while standing
- Potential for sexual function
Patient satisfaction rates are generally high. Most individuals experience significant improvement in gender congruity, psychological wellbeing, and social confidence. However, it is important to recognize the need for continued support due to occasional complications or unmet expectations.
Frequently Asked Questions (FAQs)
Q: Who is a candidate for phalloplasty?
A: Candidates are trans men and non-binary individuals seeking gender-affirming genital surgery after detailed medical and psychological assessment. Typically, readiness involves hormonal therapy, confirmed diagnosis of gender dysphoria, ability to provide informed consent, and overall good health.
Q: Are there different options besides phalloplasty?
A: Metoidioplasty is an alternative, using clitoral tissue grown via testosterone for a smaller phallus with urethral extension. Surgical approach depends on goals and anatomy.
Q: How many surgeries are involved in phalloplasty?
A: Phalloplasty is usually staged, with multiple procedures over several months or years. The number depends on the chosen technique and patient-specific factors.
Q: What is the healing time after phalloplasty?
A: Initial recovery involves a hospital stay of several days; full recovery may take several months with staged surgeries and rehabilitation.
Q: Are there risks with genital prosthetics?
A: Risks include device migration, infection, or malfunction. These are generally managed with additional surgery or device replacement.
Q: Will sensation be restored?
A: Surgeons perform nerve coaptation to maximize tactile and erogenous sensation. Results vary, but many patients regain some degree of feeling.
Q: Why is laser hair removal needed on the forearm?
A: Laser hair reduction minimizes risk of unwanted hair growth inside the new urethra, improving hygiene and comfort.
Key Takeaways
- Phalloplasty is a complex, multi-stage gender-affirming surgery that aligns anatomical features with gender identity.
- Options range from free flap (forearm, thigh, back) to pedicled flap techniques, plus adjunct procedures for optimal aesthetics and function.
- Preparation and recovery require multidisciplinary care, with attention to physical, psychological, and social wellbeing.
- High patient satisfaction rates testify to the procedure’s life-changing impact, but risks and the possibility of revision remain.
Additional Resources
- International centers specializing in gender-affirming surgery
- Transgender patient advocacy organizations
- Mental health counseling and support groups
- Peer-reviewed clinical guidance documents (WPATH, Endocrine Society)
References
- https://www.uclahealth.org/medical-services/gender-health/programs-services/genital-reconstructive-services-bottom-surgery
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11477944/
- https://atm.amegroups.org/article/view/58864/html
- https://imgender.com/en/phalloplasty-surgery/
- https://transcare.ucsf.edu/guidelines/phalloplasty
- https://my.clevelandclinic.org/health/procedures/21585-phalloplasty
- https://www.dartmouth-hitchcock.org/transgender-health-program/phalloplasty
- https://www.mayoclinic.org/tests-procedures/masculinizing-surgery/about/pac-20385105
Read full bio of Sneha Tete












