Peripheral Vascular Disease: Causes, Symptoms, and Advances in Care
Understand the risks, symptoms, causes, diagnosis, and treatment advances for Peripheral Vascular Disease and related complications.
Peripheral Vascular Disease (PVD) affects millions globally and is among the leading causes of morbidity from vascular disorders outside the heart and brain. This guide comprehensively examines the origins, risk factors, warning signs, diagnostic approaches, and new treatment options for PVD.
What is Peripheral Vascular Disease?
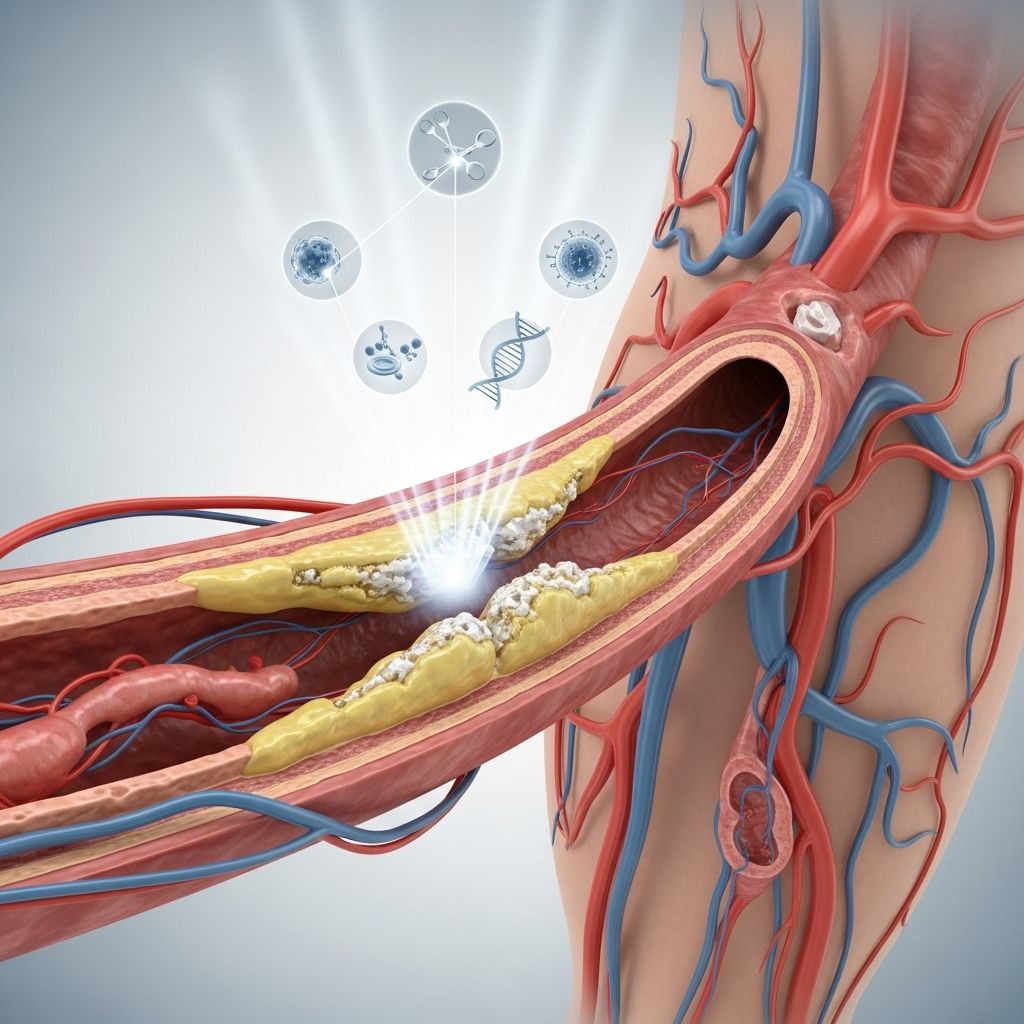
Peripheral Vascular Disease is a term for conditions which involve narrowing or blockage of blood vessels outside the heart and brain, typically in the legs and arms. Most commonly, it results from atherosclerosis—a buildup of fatty deposits within vessel walls that restricts blood flow to limbs and other peripheral areas.
PVD is often used interchangeably with Peripheral Artery Disease (PAD), though PVD technically encompasses both arterial and venous disease. However, in clinical use, PVD usually refers to arterial disease impacting the limbs.
Understanding the Blood Vessels Involved
- Arteries: Carry oxygen-rich blood from the heart to the body.
- Veins: Return oxygen-poor blood back to the heart.
- PVD mainly affects arteries, but can also involve veins, though less commonly.
Causes of Peripheral Vascular Disease
In the majority of cases, PVD is caused by atherosclerosis. Other underlying mechanisms or risk factors may also contribute:
- Diabetes: High blood sugar damages vessels and accelerates narrowing.
- Obstruction: Blood clots (thrombus) can suddenly block a vessel.
- Infection: Conditions like syphilis or salmonellosis can scar and narrow blood vessels.
- Arteritis: Inflammation of arteries, sometimes due to autoimmune disease.
- Congenital defects: Rarely, vessels may be abnormally narrow from birth.
- Vessel spasm: Raynaud’s disease and other disorders can cause narrowing in response to cold or stress.
Risk Factors
The likelihood of developing PVD increases with the presence of certain factors:
- Smoking: Tobacco greatly heightens risk—every additional 10 cigarettes increases odds for PVD by 1.4 times.
- Diabetes: Damages both small and large blood vessels.
- High blood pressure: Chronic hypertension stiffens and damages vessel walls.
- High cholesterol: Increases atherosclerotic plaque buildup.
- Obesity: Worsens cardiovascular strain and increases risk of hypertension and diabetes.
- Increasing Age: More common over age 50, especially over 65.
- Family History: Genetics influence susceptibility to vascular disease.
Who is Most at Risk?
- Individuals over 50 years old, especially those with a history of smoking or diabetes.
- Men are slightly more likely to develop PVD than women.
- People with a personal or family history of atherosclerosis, heart attack, or stroke.
- Patients with metabolic syndrome.
Common Symptoms of PVD
PVD symptoms often develop slowly. Early stages frequently go unnoticed or are mistaken for normal effects of aging or inactivity. The most common and distinctive symptoms include:
- Intermittent Claudication: Cramping, pain, fatigue, or heaviness in leg muscles during exercise, relieved by rest.
- Increased pain with activity and relief with rest.
- Coldness in affected body part—often feet or lower legs.
- Numbness or *pins and needles* sensation.
- Muscle weakness in the legs.
- Skin color changes: Blue, purple, or pale discoloration.
- Non-healing wounds or ulcers—especially on feet or toes.
- Gangrene: Blackened, decayed tissue, signifying severe and irreversible blood loss.
Many people with PVD are asymptomatic until the disease is advanced.
Complications of Peripheral Vascular Disease
If left untreated, PVD can lead to serious complications including:
- Critical Limb Ischemia: Long-term reduction in blood flow resulting in severe pain, ulcers, or gangrene. May require amputation.
- Increased risk of heart attack and stroke: Since PVD is a marker of systemic atherosclerosis.
- Infection and slow wound healing: Lack of blood supply impairs tissue recovery and defense against infection.
- Amputation: In severe cases, removal of the affected limb may be necessary.
Diagnosis of Peripheral Vascular Disease
Diagnosis is based on a combination of medical history, physical examination, and diagnostic tests:
- History: Focus on leg pain, activity level, and risk factors.
- Physical Exam: Key findings include diminished or absent pedal pulses, cool skin, abnormal coloration, ulcers, presence of bruits (whooshing sounds over arteries), and sometimes muscle atrophy or hair loss on legs.
Key Diagnostic Tests
- Ankle-Brachial Index (ABI): Compares blood pressure in ankle and arm using a blood pressure cuff and Doppler; ABI less than 0.9 is suggestive of PVD.
- Duplex Ultrasonography: Combines sound waves and Doppler to visualize blood flow and pinpoint blockages or narrowing.
- Magnetic Resonance Angiography (MRA): MRI technique using contrast dye to image arteries.
- Computed Tomography Angiography (CTA): Cross-sectional imaging for arterial assessment, particularly before surgical planning.
- Conventional Arteriography: X-ray with injected dye for detailed vascular mapping, reserved for pre-intervention planning.
- Lab Workup: CBC (complete blood count), fasting glucose/A1C, lipid profile, kidney function, urinalysis for protein or glucose.
Prevention of Peripheral Vascular Disease
The most effective approaches to lower the risk or delay progression of PVD involve lifestyle changes and management of existing health conditions:
- Stop smoking: Smoking cessation is the single most powerful measure to reduce risk.
- Exercise regularly: Physical activity (even walking programs) enhances circulation and increases walking distance before symptom onset.
- Control high blood pressure and cholesterol: Through medication and diet.
- Manage diabetes: Monitoring and maintaining target blood glucose levels.
- Healthy eating: Prioritize fruits, vegetables, fiber, and limited saturated fats and cholesterol.
Treatment Options for Peripheral Vascular Disease
Treatment aims to relieve symptoms, halt progression, improve quality of life, and reduce cardiovascular risk.
Lifestyle Modifications
- Smoking cessation: Access to programs for quitting.
- Supervised exercise therapy: Structured walking programs are proven to boost pain-free walking time and distance—sometimes by as much as 150% (over six additional minutes walking time).
- Nutrition counseling: Especially for cholesterol and hypertension control.
- Diabetes management: Achieving optimal glycemic control.
Medications
- Statins: Lower “bad” cholesterol (LDL), reduce plaque buildup, and lower heart attack/stroke risk.
- Antiplatelets: Aspirin or clopidogrel to prevent blood clots and reduce vascular events.
- Blood pressure medications: ACE inhibitors, beta blockers, or others for optimal blood pressure control.
- Agents for leg pain: Cilostazol can improve walking in people with claudication, although not suitable for all, especially with heart failure.
- Diabetes medications: For those requiring improved glucose control.
Minimally Invasive and Surgical Interventions
- Balloon Angioplasty: A catheter is used to open narrowed arteries, sometimes with advanced methods like intravascular lithotripsy for heavily calcified arteries.
- Stenting: A mesh-like tube is placed to keep arteries open after angioplasty.
- Atherectomy: Technique to remove atherosclerotic plaque from vessel walls in select cases.
- Bypass Surgery: Creating a new pathway for blood to flow around blockage using a vessel graft.
- Amputation: In extreme cases, for irreversible gangrene or infection.
Supportive Care and Monitoring
- Wound care for non-healing ulcers.
- Limb preservation services for advanced cases.
- Periodic surveillance (follow-ups) with vascular specialists.
Living with Peripheral Vascular Disease
Ongoing care for PVD involves a multidisciplinary approach and patient engagement in healthy living. Key points for management:
- Track symptoms: Note any worsening of leg pain, numbness, color changes, or wounds.
- Regular medical checkups to monitor blood pressure, cholesterol, and blood sugar.
- Promptly report any new symptoms or infections, especially ulcers or redness in feet and legs.
- Adhere to prescribed medications and exercise regimens.
Peripheral Vascular Disease and Associated Conditions
PVD often coexists with other vascular disorders. Awareness and management of additional health issues—coronary artery disease, carotid artery disease, and chronic kidney disease—are crucial for overall outcomes.
Frequently Asked Questions (FAQs)
What is the difference between peripheral artery disease and peripheral vascular disease?
Peripheral artery disease (PAD) specifically refers to narrowing or blockage of arteries—most often in the legs—whereas peripheral vascular disease (PVD) is a broader term that can also include blood vessel disorders of veins and lymphatics.
If I don’t have leg pain, could I still have PVD?
Yes, PVD may be asymptomatic or produce only subtle symptoms in early stages; many people are diagnosed only after the disease is advanced or complications develop.
Can PVD be cured?
There is no cure for PVD, but most cases can be managed and progression slowed with lifestyle changes, medication, and—in some cases—surgical intervention.
What are the warning signs of complications I should watch for?
Seek immediate care if you notice severe pain, non-healing wounds, blackened areas on your toes or feet, or sudden coolness/paleness in a limb.
Key Points to Remember
- PVD is a common and often underdiagnosed circulatory disorder.
- Most cases are related to atherosclerosis but can also be caused by clots, infections, or other conditions.
- Symptoms range from mild discomfort to severe limb-threatening gangrene.
- Diagnosis is based on symptoms, physical exam, and vascular imaging.
- Lifestyle changes are fundamental to prevention and management.
- Advanced cases may need minimally invasive or surgical procedures.
- Prompt and ongoing care can prevent progression and improve quality of life.
If you have symptoms or risk factors for PVD, speak to your healthcare provider promptly for screening and guidance on managing your vascular health.
References
- https://www.aafp.org/pubs/afp/issues/2006/0601/p1971.html/1000
- https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/peripheral-vascular-disease
- https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/diagnosis-treatment/drc-20350563
- https://www.rush.edu/conditions/peripheral-vascular-disease-pvd
- https://www.yalemedicine.org/conditions/peripheral-vascular-disease
- https://www.mayoclinic.org/diseases-conditions/peripheral-artery-disease/symptoms-causes/syc-20350557
- https://my.clevelandclinic.org/health/diseases/17357-peripheral-artery-disease-pad
- https://www.nhs.uk/conditions/peripheral-arterial-disease-pad/treatment/
Read full bio of Sneha Tete












