Pericarditis and COVID-19: Understanding Heart Inflammation Associated With Coronavirus
Explore the connection between pericarditis and COVID-19—from symptoms and risks to diagnosis and treatment options.
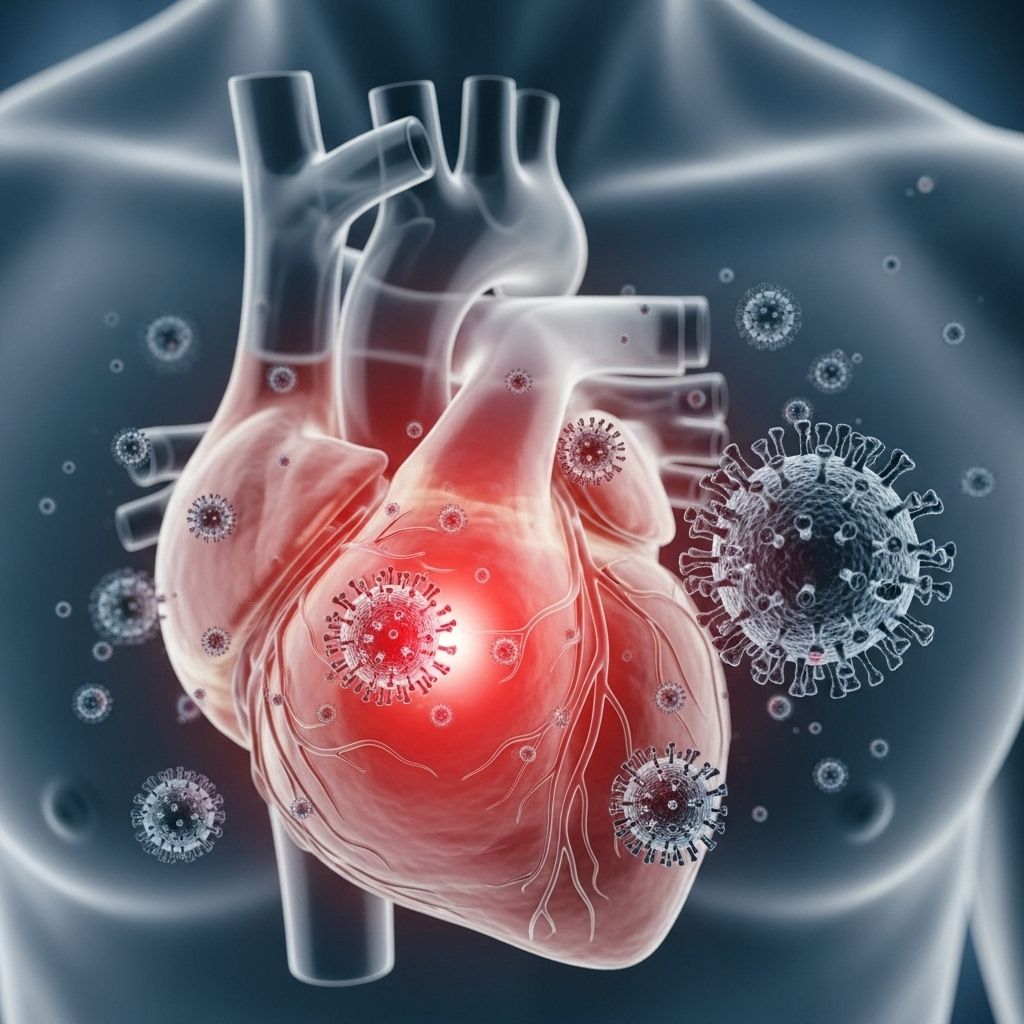
Pericarditis and COVID-19: Symptoms, Causes, and Treatment
COVID-19 has affected millions globally and revealed complex relationships between viral infections and cardiovascular health. Pericarditis, inflammation of the protective pericardial sac around the heart, can be triggered by COVID-19 in rare cases. This article explores the link between COVID-19 and pericarditis, potential symptoms, who is at risk, diagnostic criteria, management strategies, and how this condition fits into the broader picture of COVID-19’s cardiovascular impacts.
Table of Contents
- Is there a link between COVID-19 and pericarditis?
- Symptoms of COVID-19-Associated Pericarditis
- When Does COVID-19-Related Pericarditis Occur?
- Who Is at Risk?
- Diagnosis and Evaluation
- Treatment Options
- Pericarditis and Long COVID
- Potential Complications
- Prevention and Monitoring
- Frequently Asked Questions (FAQs)
Is There a Link Between COVID-19 and Pericarditis?
COVID-19 can trigger pericarditis, though this outcome is uncommon. The pericardium is a thin, double-layered sac that surrounds the heart, acting as a protective barrier and minimizing friction from surrounding tissues. When infected by viruses—including SARS-CoV-2, the virus responsible for COVID-19—the pericardium may become inflamed, leading to pericarditis.
The link to COVID-19 stems from:
- Direct infection of heart tissue or pericardium by the coronavirus.
- An exaggerated immune response, in which the body’s defense mechanisms inadvertently attack its own tissues.
- In some cases, a combination of both viral invasion and immune reaction.
Pericarditis may develop independently, or occur alongside myocarditis—an inflammation of the heart muscle—resulting in the diagnosis of myopericarditis or perimyocarditis depending on the predominance of tissue involvement.
All documented variants of SARS-CoV-2 have been associated with cases of pericarditis and myocarditis, but detailed incidence data for pericarditis remain incomplete compared to myocarditis.
Symptoms of COVID-19-Associated Pericarditis
Research indicates that symptoms of pericarditis linked to COVID-19 mirror those of other viral pericarditis cases, primarily impacting the structures around the heart. Common symptoms include:
- Sudden-onset chest pain, often sharp and stabbing:
- Worse with deep breathing or lying down
- Improves when sitting up or leaning forward
- Rapid (tachycardic) heart rate
- Shortness of breath
- General weakness or fatigue
- Low-grade fever
- Cough
- Heart palpitations (fluttering or irregular heartbeat)
For some, symptoms may emerge while actively experiencing COVID-19; for others, pericarditis manifests after initial recovery.
When Does COVID-19-Related Pericarditis Occur?
Pericarditis may appear:
- During the acute phase of COVID-19 infection
- Anywhere from 5 to 56 days after recovery, based on case reports
- As a symptom of long COVID, months after apparent viral clearance
Long COVID refers to lingering symptoms and health concerns persisting weeks, months, or even years after a COVID-19 infection; pericarditis is now recognized within this spectrum in select cases.
Who Is at Risk of Pericarditis?
Certain groups may face elevated risk for developing COVID-19-related pericarditis:
- Young adults (though middle-aged individuals commonly affected)
- Males under age 50
- Individuals with rare genetic conditions
Risk factors do not guarantee development of pericarditis, but they indicate increased susceptibility compared to the general population.
Diagnosis and Evaluation
Diagnosing pericarditis relies on recognition of hallmark signs and multimodal assessment:
- Clinical symptoms: Chest pain, pericardial rub (distinctive sound on heart auscultation), shortness of breath
- Electrocardiogram (ECG/EKG): Characteristic alterations in heart rhythm
- Echocardiogram: Visualization of pericardial inflammation or fluid accumulation (effusion)
- Blood tests: Checking for markers of inflammation (e.g. C-reactive protein), cardiac injury (troponins), and immune activation
- Imaging: CT or MRI may provide additional detail, particularly in complex cases
Thorough evaluation is essential because pericarditis can mimic or coexist with other cardiac emergencies, such as myocardial infarction (heart attack) or myocarditis.
Treatment Options
Most cases of COVID-19-related pericarditis are managed with a combination of rest and anti-inflammatory medications. Treatment goals center on symptom relief, reduction of inflammation, and prevention of complications or recurrence. Typical strategies include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Ibuprofen, naproxen, or other OTC or prescription drugs to relieve pain and inflammation
- Aspirin: Often used due to additional cardiovascular benefits
- Colchicine: An anti-inflammatory used for both acute and recurrent pericarditis
If pericarditis recurs or does not resolve with standard therapies, additional medications may be considered:
- Interleukin-1 (IL-1) inhibitors: For recurrent cases, rilonacept (ARCALYST) is approved for management and reduction of future episodes in adults and pediatric patients (≥12 years)
Hospitalization may be necessary in severe cases, especially when symptoms suggest cardiac tamponade (dangerous compression of the heart) or major complications. In such situations, pericardial drainage or advanced therapies might be required.
Pericarditis and Long COVID
Post-COVID syndrome, or long COVID, describes persistent symptoms—including pericarditis—that extend beyond the typical recovery window. People experiencing chest pain, shortness of breath, or fatigue weeks after COVID-19 should consult with a healthcare provider for evaluation. Research suggests that heart inflammation can be a part of the evolving post-infection health landscape, necessitating vigilance and continued investigation.
Potential Complications
While most cases of pericarditis following COVID-19 are mild and responsive to treatment, complications can occur:
- Pericardial effusion: Excess fluid buildup leading to pressure on the heart
- Cardiac tamponade: Life-threatening compression requiring emergency intervention
- Recurrent or chronic pericarditis: Continued inflammation despite initial therapy
- Associated cardiac complications: Increased risk of heart failure, arrhythmias, and other severe manifestations, especially in hospitalized individuals
Close monitoring and follow-up are crucial for early detection and management of these complications.
Prevention and Monitoring
- Prompt management of COVID-19 per national and international guidelines helps reduce complication risks.
- Early recognition of chest pain and other new cardiovascular symptoms is key.
- Individuals who have recovered from COVID-19 but develop persistent symptoms should seek medical advice and may benefit from heart health screening.
- COVID-19 vaccination provides protection against severe disease, but in rare instances can also be associated with pericarditis or myocarditis. These cases, however, are infrequent and generally milder than those associated with the infection itself.
Frequently Asked Questions (FAQs)
Q: What causes pericarditis in people with COVID-19?
A: Pericarditis can result from direct viral infection of the pericardium or the body’s immune response to SARS-CoV-2. The inflammatory reaction, sometimes disproportionately strong, damages pericardial tissues and produces the classic symptoms of pericarditis.
Q: How common is pericarditis in COVID-19 patients?
A: Pericarditis is relatively rare compared to myocarditis in COVID-19 cases. Estimates for myocarditis are more robust (e.g., ~150 cases per 100,000 people with COVID-19), whereas pericarditis’s precise frequency is less well-defined but generally lower.
Q: What are the most serious risks associated with COVID-19-related pericarditis?
A: While most cases resolve, the most serious risks include cardiac tamponade and chronic or recurrent inflammation that can lead to structural damage to the heart. Hospitalized patients may face higher risks for complications like heart failure and arrhythmias.
Q: Are there effective therapies for COVID-19-induced pericarditis?
A: Yes. Most recover with NSAIDs, aspirin, and colchicine. Recurrent cases may require biologics such as IL-1 inhibitors (e.g., rilonacept). In severe cases, interventional therapies may be needed.
Q: Can COVID-19 vaccination cause pericarditis?
A: Rarely, pericarditis and myocarditis have occurred after vaccination. These cases are infrequent, usually mild, and should be weighed against the severe risks associated with COVID-19 infection itself.
Summary Table: Key Facts About Pericarditis and COVID-19
| Aspect | Description |
|---|---|
| Cause | Direct viral infection; immune response; rarely after vaccination |
| Symptoms | Sharp chest pain, rapid heart rate, fatigue, fever, palpitations |
| Timing | During COVID-19, 5–56 days post-diagnosis, or as long COVID |
| Risk Groups | Young adults, males (under 50), rare genetic conditions |
| Treatment | NSAIDs, aspirin, colchicine, IL-1 inhibitors (for recurrent cases) |
| Complications | Effusion, tamponade, heart failure, arrhythmia, recurrent pericarditis |
Additional Resources
- National Heart, Lung, and Blood Institute: Heart inflammation information and patient guidance.
- Centers for Disease Control and Prevention (CDC): COVID-19 risk factors and heart health updates.
- American Heart Association: COVID-19’s cardiovascular impact overview.
Takeaway
While COVID-19-associated pericarditis remains rare, it is a clinically significant manifestation of heart inflammation that demands prompt recognition and tailored management. Persistent or recurrent symptoms—especially chest pain—after COVID-19 should be medically evaluated to ensure early intervention and optimal recovery. Ongoing research will continue to reveal new insights into the short- and long-term impacts of SARS-CoV-2 infection on cardiovascular health.
References
- https://ada.com/covid/pericarditis-and-covid-19/
- https://www.healthline.com/health/heart-health/pericarditis-and-covid
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8173318/
- https://www.ahajournals.org/doi/10.1161/JAHA.123.031338
- https://www.healthline.com/health/heart-disease/covid-heart-disease
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7826081/
- https://openrespiratorymedicinejournal.com/VOLUME/16/ELOCATOR/e187430642210190/FULLTEXT/
- https://www.cureus.com/articles/101512-a-systematic-review-of-covid-19-and-pericarditis
- https://www.acc.org/Latest-in-Cardiology/Articles/2021/02/05/19/37/COVID-19-as-a-Possible-Cause-of-Myocarditis-and-Pericarditis
- https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.123.321878
Read full bio of medha deb












