Pericardial Window: Surgical Relief for Fluid Around the Heart
A comprehensive guide to pericardial window surgery, including indications, procedures, recovery, and frequently asked questions.
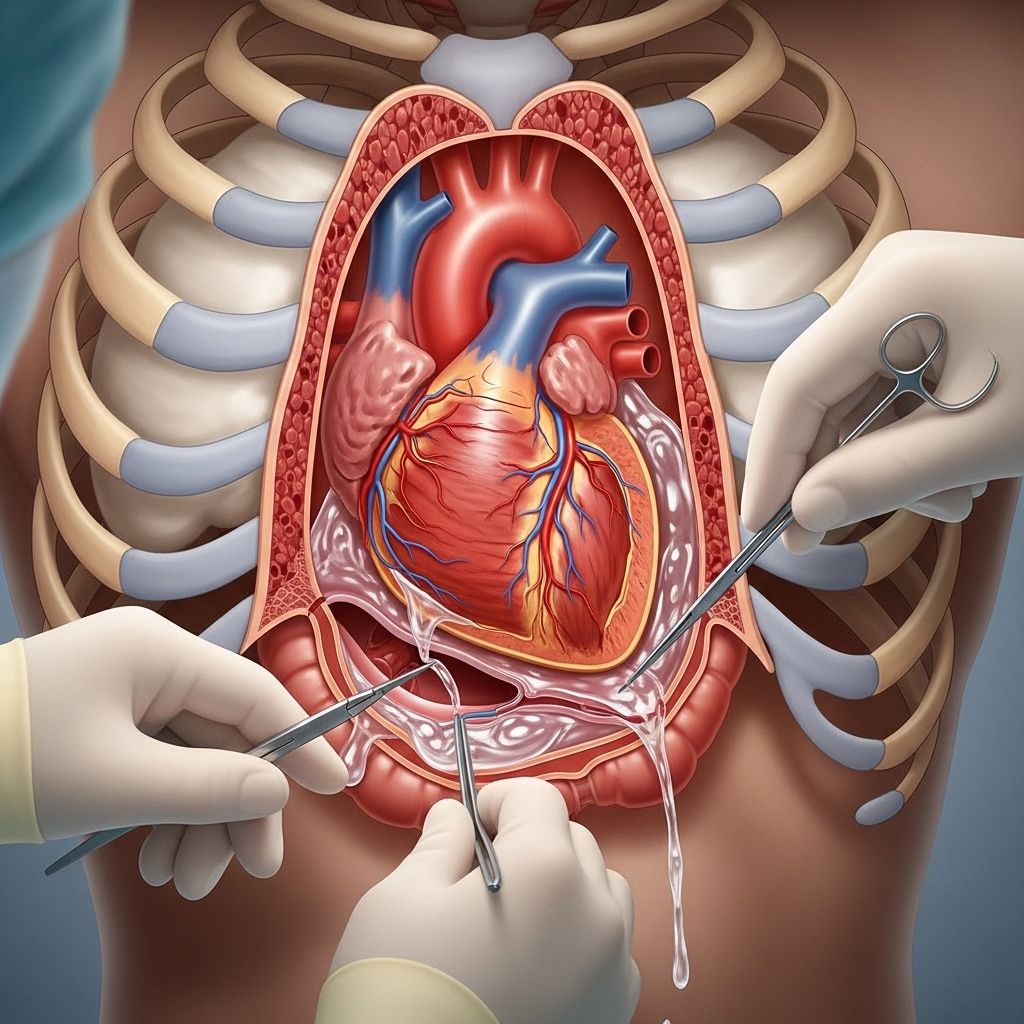
Pericardial Window Surgery Overview
A pericardial window is a surgical procedure designed to treat pericardial effusion — an abnormal accumulation of fluid around the heart. This procedure involves creating an opening in the pericardium (the protective sac surrounding the heart) to allow excess fluid to drain, relieving pressure and restoring proper cardiac function.
The pericardial window is often recommended when other, less invasive methods of fluid removal, such as pericardiocentesis, are ineffective or when the condition recurs or is accompanied by diagnostic uncertainty.
What Is the Pericardium?
The pericardium is a double-layered fibrous sac covering the heart. It contains a small amount of lubricating fluid, which reduces friction during heartbeats. Excessive fluid build-up in the pericardium, known as pericardial effusion, can compress the heart and impair its function.
Pericardial effusion may result from various causes, and when this accumulation is significant, it can become a life-threatening emergency requiring intervention.
Indications: Why Is a Pericardial Window Needed?
Many conditions may require the creation of a pericardial window. These include:
- Infection of the heart or pericardial sac
- Cancer (especially metastatic cancer affecting the heart or pericardium)
- Inflammation due to myocardial infarction (heart attack) or other causes
- Trauma or injury to the chest
- Immune system disorders
- Medication reactions
- Radiation therapy effects
- Metabolic conditions (e.g., kidney failure with uremia)
- Idiopathic (unknown cause) fluid accumulation
Common symptoms suggestive of significant pericardial effusion include:
- Shortness of breath
- Chest pain or pressure
- Dizziness or lightheadedness
- Nausea
- Low blood pressure
- Rapid or irregular heartbeat
Comparison: Pericardial Window vs. Pericardiocentesis
| Procedure | Method | Indications | Advantages | Limitations |
|---|---|---|---|---|
| Pericardiocentesis | Needle aspiration with a catheter | Initial, mild to moderate effusions; urgent relief | Minimally invasive; quick recovery | Temporary relief; higher risk of recurrence |
| Pericardial Window | Surgical removal of pericardial tissue | Recurrent/large effusions; when catheter drainage fails or tissue diagnosis is needed | Permanent drainage; diagnostic tissue sample possible | More invasive; surgical risks |
Preparing for a Pericardial Window Surgery
The process leading to a pericardial window procedure typically involves thorough diagnostic assessment to confirm the effusion and identify its cause. Pre-operative evaluation may include:
- Chest X-rays
- Electrocardiogram (ECG/EKG)
- Blood tests
- Echocardiography (ECHO)
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Cardiac catheterization
Before surgery, patients are advised to:
- Share full medical history, including medications and allergies
- Follow fasting instructions as required by the anesthesiologist
- Arrange for post-operative transportation and care
- Discuss risks, benefits, and alternatives with the surgical team
How Pericardial Window Surgery Is Performed
Pericardial window surgery can be conducted through various approaches, depending on the patient’s anatomy, underlying condition, and surgeon’s expertise. All are designed to create a lasting outlet for fluid to escape from the pericardium into the chest or abdominal cavity, where it can be reabsorbed by the body.
Surgical Techniques
- Subxiphoid Approach: An incision made a few inches below the breastbone allows access to the pericardium; a small portion is removed to create the window.
- Thoracotomy Approach: The surgeon makes an incision between the ribs to reach the pericardium.
- Video-Assisted Thoracoscopic Surgery (VATS): Multiple small incisions are made in the side of the chest. A tiny camera and instruments allow the surgeon to view and remove pericardial tissue, creating the window without a large incision.
Most procedures are performed under general anesthesia, but in selected cases, local or regional anesthesia with sedation may be considered.
During the procedure:
- The surgical team monitors vital signs continuously.
- A breathing tube is inserted for airway control and respiration during general anesthesia.
- A small piece of the pericardium is excised (removed). This creates a “window” allowing fluid to drain into the pleural (chest) or peritoneal (abdominal) cavity.
- A chest tube or surgical drain may be placed to facilitate post-operative drainage.
- The incisions are sutured and dressed.
- Fluid samples may be sent to the laboratory for analysis to determine the cause of effusion.
Risks and Potential Complications
- Infection at the incision or within the chest cavity
- Bleeding due to tissue or vessel injury
- Damage to the heart or surrounding organs
- Arrhythmias (abnormal heart rhythms)
- Pneumothorax (collapsed lung)
- Persistent or recurrent effusion
- Heart failure
- Rarely, death
Most complications are uncommon, but the surgical team will discuss specific risk factors with each patient before the procedure.
Recovery After a Pericardial Window Procedure
Patients typically spend several days in the hospital after surgery. Recovery includes:
- Close monitoring of heart and lung function
- Pain management with medications
- Continued drainage until fluid is minimized
- Ultrasound or imaging follow-up to assess effusion
- Gradual resumption of activity based on doctor’s guidance
Most people can return to daily activities within a few weeks, depending on their overall health and the underlying cause of the effusion.
Follow-Up Care
- Regular check-ups to monitor for recurrence
- Analysis of fluid/tissue samples, if taken, for diagnosis and treatment planning
- Adjustment of medications based on findings
- Supportive care for underlying causes (e.g., infection, cancer, kidney disease)
Frequently Asked Questions (FAQs)
What is a pericardial window?
A pericardial window is a surgical procedure in which a small portion of the pericardium (the membrane surrounding the heart) is removed to allow excess fluid to drain into an adjacent body cavity, relieving pressure on the heart.
Why is a pericardial window performed?
It is performed to treat large or recurrent pericardial effusions that can’t be managed by less invasive procedures, or when tissue analysis is necessary for diagnosis.
How long does recovery take?
Recovery varies depending on the patient’s condition but generally takes a few weeks. Most patients are hospitalized for several days post-surgery for close monitoring.
What risks are associated with pericardial window surgery?
Risks include infection, bleeding, heart damage, abnormal rhythms, pneumothorax, recurrence of fluid, heart failure, and rarely, death.
Will I have any physical restrictions after surgery?
Patients may need to limit strenuous activities for several weeks and follow specific physician instructions to ensure proper healing.
Does a pericardial window provide a permanent solution?
The procedure offers a lasting outlet for fluid drainage and can be curative. However, the recurrence depends on the underlying cause of effusion and ongoing disease management.
Can fluid build-up recur after the procedure?
While less common than after pericardiocentesis, fluid may recur especially if the underlying disease progresses. Routine follow-up is vital.
Key Takeaways
- The pericardial window is a critical surgical intervention for symptomatic or recurrent fluid around the heart.
- It addresses underlying causes and helps relief symptoms, improves heart function, and can aid diagnosis.
- Multiple surgical approaches are available, each tailored to the individual patient and underlying disease.
- Comprehensive pre- and post-operative care minimises risks and promotes recovery.
Additional Resources
- Consult with your healthcare provider for personalized evaluation and decision-making.
- American Heart Association: Cardiac Procedures and Surgeries
- National Institutes of Health: Heart, Lung, and Blood Institute
- Cancer Care Organizations for cancer-related effusions
References
- Hopkins Medicine: Treatment – Pericardial Window
- MyLungCancerTeam: Pericardial Window for Lung Cancer
- University of Rochester Medical Center: Pericardial Window
- RWJBarnabas Health: Tests & Procedures – Pericardial Window
References
- https://www.mylungcancerteam.com/treatments/pericardial-window
- https://www.urmc.rochester.edu/encyclopedia/content?contenttypeid=135&contentid=359
- https://www.rwjbh.org/treatment-care/heart-and-vascular-care/tests-procedures/pericardial-window/
- https://pubmed.ncbi.nlm.nih.gov/36029363/
- https://pure.johnshopkins.edu/en/publications/pericardial-effusion-and-tamponade-evaluation-imaging-modalities–4
- https://pubmed.ncbi.nlm.nih.gov/18414173/
- https://pure.johnshopkins.edu/en/publications/poor-outcomes-associated-with-drainage-of-pericardial-effusions-i-3
Read full bio of Sneha Tete












