Percutaneous Coronary Intervention: A Comprehensive Guide
An in-depth look at how PCI restores blood flow, reduces symptoms, and improves quality of life for those with coronary artery disease.
Percutaneous Coronary Intervention (PCI): A Comprehensive Guide
Percutaneous coronary intervention (PCI), also known as coronary angioplasty with stent placement, is a minimally invasive, non-surgical procedure that opens blocked or narrowed coronary arteries and restores essential blood flow to the heart muscle. By relieving obstructions caused by coronary artery disease, PCI can prevent heart attacks, reduce symptoms such as chest pain, and improve patient outcomes. This article provides an in-depth look at PCI, including indications, preparation, procedural steps, recovery, risks, and frequently asked questions.
What is Percutaneous Coronary Intervention?
Percutaneous coronary intervention (PCI) is a non-surgical procedure performed in a specialized environment known as a catheterization laboratory (cath lab). The main goal is to treat the narrowing (stenosis) or obstruction of the heart’s coronary arteries, conditions most often due to coronary artery disease (CAD). PCI remains an essential treatment for acute heart attacks (myocardial infarction), stable and unstable angina, and other indications where restoring blood flow reduces heart damage and symptoms.
- Minimally invasive: Performed through a small puncture in the wrist or groin instead of large surgical incisions
- Alternative to cardiac surgery: Less invasive than coronary artery bypass grafting (CABG)
- Main methods: Most commonly uses balloon angioplasty and may involve stent placement
Why Is PCI Performed?
PCI is used to treat and manage a range of heart conditions that involve insufficient blood flow to the heart muscle due to narrowed or blocked arteries.
- Angina pectoris: Both stable and unstable chest pain resulting from restricted blood supply to the heart
- Acute myocardial infarction (heart attack): Especially recommended for ST-segment elevation myocardial infarction (STEMI), as early PCI can quickly restore blood flow and minimize heart damage
- Myocardial ischemia: Reduced oxygen delivery to heart muscle causing symptoms or weakening heart function
- High-risk findings on stress testing: Severe blockages or symptoms persist despite medications
- Refractory angina: Symptoms that do not respond to medication alone
The procedure can be life-saving during a heart attack and significantly improves quality of life for individuals with angina or other forms of coronary artery disease.
Who Needs Percutaneous Coronary Intervention?
PCI is not suitable for everyone. Cardiologists recommend it only when other treatments (like medications) are insufficient, or when there is a direct threat to heart muscle health, such as during a heart attack. Common candidates include:
- Individuals with severe, persistent chest pain not controlled by medication
- Those with a high risk of heart attack, as determined by diagnostic tests (e.g., abnormal stress tests or imaging)
- Patients experiencing a heart attack (especially STEMI) who can be treated within 12 hours of symptom onset
- Those who failed or are not suitable candidates for coronary artery bypass surgery (CABG)
- Patients with unstable angina, non–ST-elevation acute coronary syndrome (NSTE-ACS), or worsening heart failure symptoms
How to Prepare for PCI
Preparation for percutaneous coronary intervention involves consultations, diagnostic imaging, and pre-procedure planning. Your health care provider will provide instructions tailored to your health and the specifics of your procedure. Typical preparation includes:
- Reviewing medical history: Including allergies (especially to contrast dyes or medications), bleeding risks, and medication lists
- Pre-procedure testing: Blood tests, electrocardiograms (ECG), chest X-rays, and kidney function assessment
- Fasting instructions: No eating or drinking for several hours before the procedure
- Medication adjustments: Some medications may be paused (e.g., blood thinners) or adjusted prior to PCI
- Arrangements for post-procedure care: Planning for transportation and assistance after the procedure
How the Procedure Works
The PCI procedure is completed using sophisticated imaging, precision instruments, and expert technique by an interventional cardiologist. The general steps are as follows:
- Access: A sheath (narrow tube) is inserted into a blood vessel in your wrist (radial artery) or groin (femoral artery). This area is cleaned, sterilized, and given local anesthesia to minimize discomfort.
- Catheter Insertion: A guiding catheter is threaded through the sheath and navigated through the blood vessels—under X-ray fluoroscopy—to the entrance of the coronary arteries.
- Contrast Dye: Contrast dye is injected via the catheter, making the arteries visible on live X-rays (angiography). This helps the cardiologist identify the location and extent of any blockages.
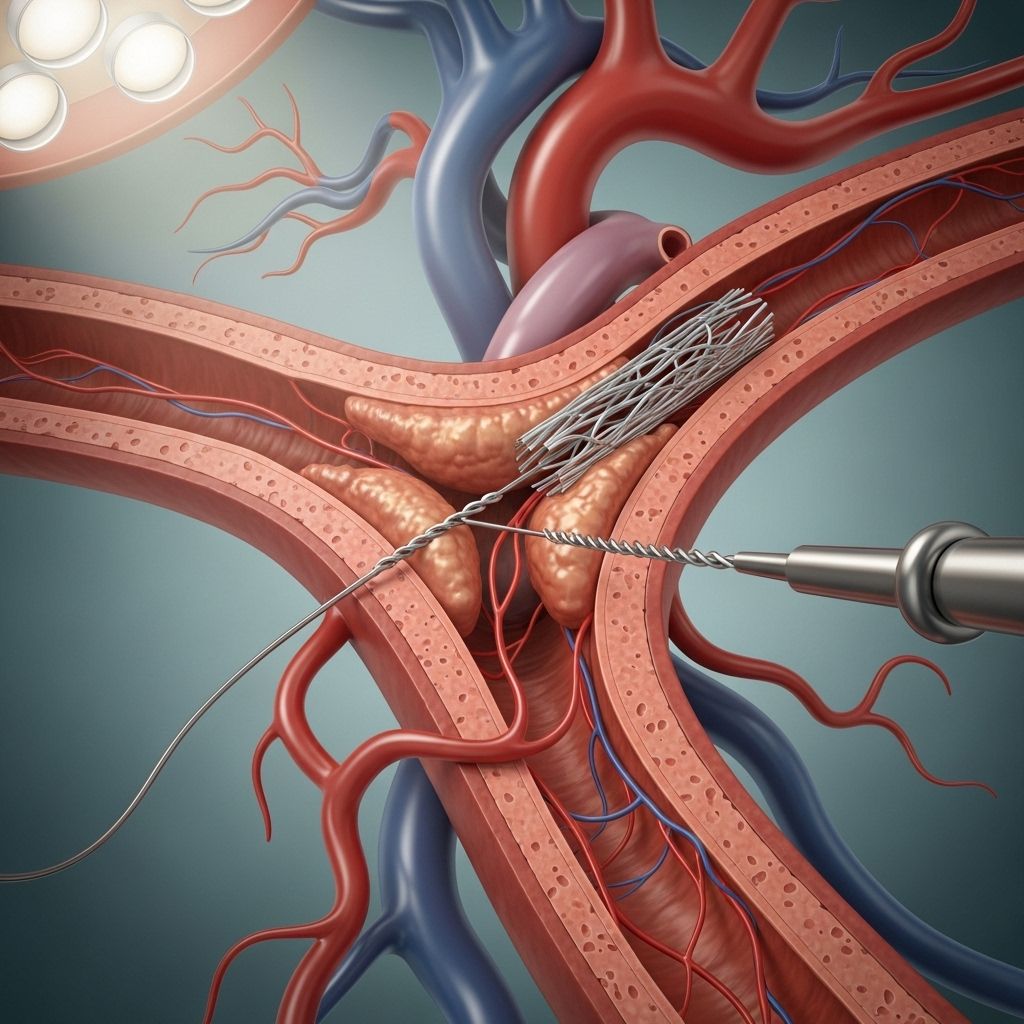
- Guidewire Placement: A thin wire is passed across the blockage as a track for other devices.
- Balloon Angioplasty: A balloon-tipped catheter is moved over the wire into the narrowed area. The balloon is inflated, compressing the plaque against the artery wall and widening the vessel.
- Stent Placement: In most cases, a wire-mesh stent (often drug-eluting to prevent re-narrowing) is delivered to the treated area. The balloon positions and deploys the stent, which holds the artery open permanently. The balloon is then deflated and removed, leaving the stent in place.
- Final Angiogram: Additional X-ray images are taken to confirm restoration of blood flow.
| Step | Description |
|---|---|
| Access | Sheath placed in wrist or groin blood vessel |
| Catheter Navigation | Guiding catheter threaded to coronary artery under X-ray |
| Angiography | Contrast dye outlines blockages |
| Balloon Angioplasty | Balloon inflates to open artery |
| Stent Placement | Wire mesh tube inserted to keep artery open |
| Confirmation | Final images check blood flow |
What to Expect During PCI
PCI typically lasts between 30 minutes and 2 hours, depending on the complexity and number of blockages. The patient is usually awake but sedated for comfort, with real-time communication possible between the patient and cardiac team throughout the process.
- Sensation: Some pressure at the insertion site, occasional chest discomfort during balloon inflation, but little pain overall
- Monitoring: Continuous heart rate, rhythm, blood pressure, and oxygen level monitoring
- Team: The procedure is performed by skilled interventional cardiologists with support staff
- Post-procedure recovery: Short observation in a recovery area; some patients may go home the same day, others may stay overnight based on their clinical status
Recovery After PCI
Recovery is typically faster and less painful than open-heart surgery:
- Observation: Most patients are monitored for several hours, and in uncomplicated cases, may be discharged within 24 hours
- Site care: Instructions are given on how to care for the catheter insertion site; avoid vigorous movement or heavy lifting for a specified period
- Activity: Light walking is encouraged, but patients should avoid strenuous exercise until cleared by their physician
- Medications: Antiplatelet drugs (e.g., aspirin, clopidogrel) may be prescribed to prevent stent clotting
- Follow-up: Regular follow-up visits are necessary to monitor recovery and manage cardiac risk factors
Potential Risks and Complications
While PCI is generally considered safe and effective, all invasive procedures carry some risks. Serious complications are rare but can include:
- Bleeding: Especially at the catheter insertion site
- Blood vessel injury: Damage to the artery used for access
- Allergic reactions: To contrast dye or medications
- Heart attack: Although rare, it can occur during or after PCI
- Stroke: Due to dislodged clots during catheter manipulation
- Restenosis: Re-narrowing of the artery, especially if a bare-metal stent (rather than a drug-eluting stent) is used
- Stent thrombosis: Blood clot formation in the stent—a medical emergency
- Kidney damage: From contrast dye, especially in patients with preexisting kidney disease
Your care team will discuss these risks and steps taken to minimize them.
Results, Outlook, and Follow-up
Most people who undergo PCI experience a significant reduction in symptoms, improved heart function, and a lower risk of future heart attacks if they adhere to medication regimens and lifestyle recommendations:
- Relief of chest pain (angina): PCI quickly decreases or eliminates angina in most patients
- Improved physical capabilities: Many resume normal activities within days
- Long-term outcomes: Success depends on the extent of coronary disease, type of stent, and management of risk factors such as hypertension, diabetes, high cholesterol, and smoking cessation
- Dual antiplatelet therapy: Essential for a period after stent placement to prevent stent thrombosis
- Lifestyle modifications: Dietary changes, regular activity, and cardiac rehabilitation help maximize long-term benefits
Alternatives to Percutaneous Coronary Intervention
Not all coronary artery disease requires PCI. Alternatives include:
- Medication alone: For less severe cases or when risk of intervention outweighs benefits
- Coronary artery bypass grafting (CABG): Open-heart surgery for extensive or complex disease
- Managing risk factors: Aggressive control of blood pressure, cholesterol, diabetes, and promoting tobacco cessation
Frequently Asked Questions (FAQs)
Q: How long does the PCI procedure take?
A: PCI typically takes 30 minutes to 2 hours, depending on the complexity and number of blockages being treated.
Q: Will I be awake during the procedure?
A: Yes. Most patients are awake but sedated for comfort. General anesthesia is not usually required.
Q: How soon can I go home after PCI?
A: Many people leave the hospital the same day or within 24 hours if there are no complications.
Q: What are the signs of trouble after PCI?
A: Notify your doctor or seek emergency help if you notice chest pain, heavy bleeding, swelling at the insertion site, fever, or shortness of breath.
Q: Will I need to take medications after PCI?
A: Yes. You will likely need to take antiplatelet medications (such as aspirin and clopidogrel) for a period of time to prevent clots within the stent.
Q: Is it possible for arteries to re-narrow after PCI?
A: Yes, called restenosis. Drug-eluting stents significantly reduce this risk compared to bare-metal stents.
Q: Can I return to normal activities?
A: Most people resume normal activities and work within a week, but your cardiologist will give you guidance based on your circumstances.
Q: Are there alternatives to PCI?
A: Yes. Depending on the case, medications and lifestyle changes, or coronary artery bypass grafting surgery, may be recommended. Your doctor will discuss the best option for you.
Summary
Percutaneous coronary intervention is a cornerstone of modern cardiology, successfully treating many types of coronary artery disease with minimal invasiveness and rapid recovery. By reopening blocked arteries, PCI helps restore heart function, relieve symptoms, and reduce the risk of severe cardiovascular complications. If you or a loved one is facing PCI, understanding the procedure, its risks, recovery process, and benefits will help guide decision-making and promote the best possible outcome.
References
- https://www.yalemedicine.org/conditions/percutaneous-coronary-intervention-pci
- https://www.merckmanuals.com/professional/cardiovascular-disorders/coronary-artery-disease/percutaneous-coronary-interventions-pci
- https://www.ncbi.nlm.nih.gov/books/NBK556123/
- https://en.wikipedia.org/wiki/Percutaneous_coronary_intervention
- https://www.ucsfhealth.org/treatments/percutaneous-coronary-intervention
- https://www.youtube.com/watch?v=HOwyDph3b2c
- https://www.heartandstroke.ca/heart-disease/treatments/surgery-and-other-procedures/percutaneous-coronary-intervention
- https://www.va.gov/COMMUNITYCARE/docs/providers/CDI/IVC-CDI-00038.pdf
- https://www.abiomed.com/en-us/patients-and-caregivers/blog/pci-vs-protected-pci-what-is-the-difference-and-which-one-is-right-for-me
Read full bio of Sneha Tete












