Percutaneous Coronary Intervention: Minimally Invasive Heart Treatment Explained
Learn how PCI restores blood flow in blocked heart arteries, improves symptom relief, and enables quick recovery.
Percutaneous Coronary Intervention (PCI): An In-Depth Guide
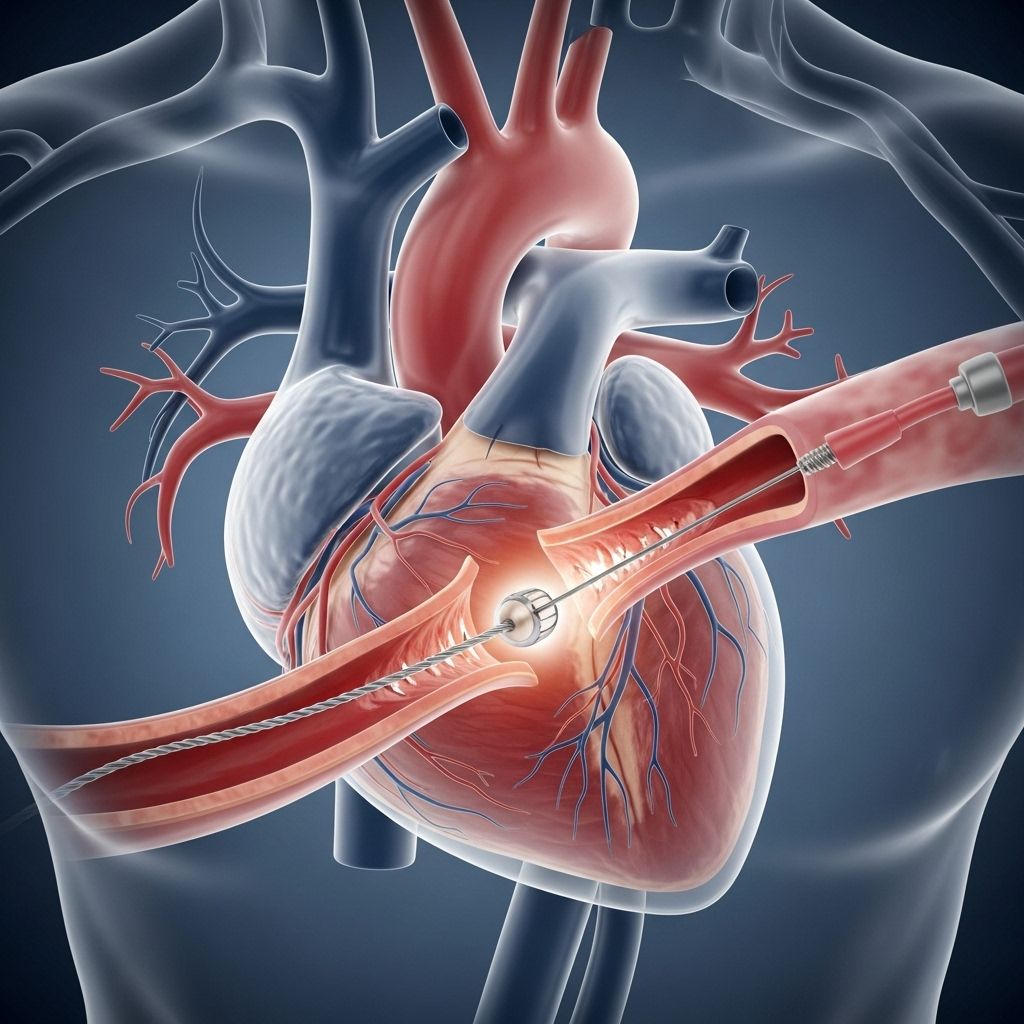
Percutaneous coronary intervention (PCI), commonly referred to as angioplasty with stent, is a minimally invasive, non-surgical procedure used to open blocked or narrowed coronary arteries. PCI is central to modern heart care, relieving symptoms, restoring blood flow, and reducing damage from heart attacks. This guide explores PCI in detail—including what it is, who needs it, how it’s performed, risks, benefits, and recovery.
What Is Percutaneous Coronary Intervention?
PCI is a procedure to treat narrowed or blocked sections of the coronary arteries, allowing improved blood flow to the heart muscle. Unlike heart surgery, PCI is performed by accessing the arteries through small punctures, mainly in the wrist (radial artery) or groin (femoral artery), and does not require opening the chest cavity.
PCI primarily involves two steps:
- Balloon angioplasty: Inflation of a small balloon within the blocked artery to widen it.
- Stent placement: Insertion of a wire-mesh tube (stent) to keep the artery open. Most stents are coated with drugs to prevent future blockage.
PCI procedures are conducted in specialized hospital labs called catheterization laboratories (cath labs) by interventional cardiologists, aided by imaging technology for real-time visualization.
Why Is PCI Needed?
PCI is principally used to treat coronary artery disease (CAD)—the buildup of plaque within arteries supplying the heart. The procedure is often recommended if medical management does not relieve symptoms or in the setting of heart attack.
Main Indications for PCI:
- Stable or unstable angina pectoris (chest pain due to reduced blood flow).
- Myocardial ischemia (reduced oxygen delivery to the heart tissue).
- Acute myocardial infarction (heart attack), especially within 90 minutes of pain onset.
- Critical narrowing of arteries not suited for open surgery (coronary artery bypass grafting, or CABG).
- Significant symptoms due to blocked arteries that are poorly controlled with medication.
In emergency settings, PCI can be life-saving by restoring circulation and preserving heart muscle.
How Is PCI Performed?
The PCI procedure generally follows these steps:
- Preparation: The patient receives intravenous medications to relax but is usually awake. Access is obtained through a blood vessel—commonly the wrist or groin.
- Catheter Insertion: A sheath is placed in the chosen artery. Through this, a thin catheter is guided to the heart using real-time X-ray imaging (fluoroscopy).
- Contrast Injection: Contrast dye is injected via the catheter to visualize the coronary arteries and identify blockages.
- Guidewire Placement: A thin wire is passed across the narrowed section of the artery.
- Balloon Angioplasty (PTCA): A balloon-tipped catheter is advanced over the guidewire to the blockage. The balloon is inflated to compress plaque and widen the artery.
- Stent Deployment: Often, a stent mounted on a balloon is delivered. The balloon inflation expands the stent, which remains in place once the balloon is deflated and withdrawn.
- Final Assessment: Repeat angiography (X-rays) is done to confirm improved blood flow. The catheters and sheath are removed, and pressure is applied to the entry site.
Types of Stents Used in PCI
| Stent Type | Description | Uses/Benefits |
|---|---|---|
| Bare-metal stent | Simple wire mesh, no drug coating. | Lower cost, but higher risk of restenosis (re-narrowing). |
| Drug-eluting stent (DES) | Wire mesh coated with medication that slowly releases. | Reduces risk of restenosis; most commonly used today. |
Benefits of Percutaneous Coronary Intervention
- Minimally invasive: No need for large chest incisions; access from wrist or groin.
- Quick symptom relief: Rapid alleviation of angina and chest pain in most cases.
- Reduced risk of heart failure and heart attack progression: Restores blood flow early during heart attack.
- Shorter recovery times: Most patients return home within 1–2 days and resume daily activities faster than with surgery.
- Lower overall risk compared to open surgery (CABG), though not suitable for all situations.
Risks and Potential Complications of PCI
While PCI is widely considered safe, risks remain, especially in older adults and those with multiple health conditions.
- Bleeding or bruising at the catheter entry site.
- Allergic reaction to contrast dye.
- Blood vessel injury or damage (rare).
- Restenosis (re-narrowing of the artery), more common with bare-metal stents.
- Formation of blood clots within the stent (stent thrombosis).
- Heart rhythm disturbances or arrhythmias.
- Heart attack, stroke, or death—rare, but severe complications may occur.
Reducing Complications
Modern techniques—such as using the radial artery for access—help minimize discomfort and complications, including bleeding and longer immobility.
Who Should Not Have PCI?
PCI may not be the best treatment in certain cases, such as:
- Extensive blockages in several arteries (often requiring coronary artery bypass surgery).
- Complex coronary anatomy or failure of previous PCI attempts.
- Severe underlying illness increasing procedure risk.
Recovery After PCI
Most patients recover quickly after PCI. Typical recovery steps include:
- Monitoring in the hospital for a few hours to overnight, depending on the case and any underlying conditions.
- Limited activity for 1–2 days, especially when the leg is used for catheter access.
- Gradual return to normal physical activity after discharge.
- Instructions for site care, medications to prevent blood clots, and lifestyle changes to support heart health.
Medications Post-PCI
Many patients will need to take “dual antiplatelet therapy”—usually aspirin and another medicine—to prevent clotting within the stent for several months.
PCI Versus Other Heart Treatments
| Treatment | Description | Main Uses | Key advantages | Key limitations |
|---|---|---|---|---|
| PCI | Minimally invasive, balloon and stent placement. | Single or limited blockages, emergency heart attack treatment. | Quick recovery, good symptom relief. | Not suitable for multiple/complex blockages. |
| Coronary artery bypass grafting (CABG) | Open heart surgery, arteries bypassed with vessels from leg/chest. | Multiple or complex blockages. | Best for extensive disease, long-term durability. | Longer recovery, higher risk surgery. |
| Medication therapy | Drugs to reduce risk and manage symptoms. | Mild/moderate symptoms, prevention. | No procedure needed, lower cost. | May not relieve significant blockages. |
Preparing for Percutaneous Coronary Intervention
- Assessment: Doctors perform blood tests, electrocardiogram (ECG), and imaging (coronary angiography) to determine the need for PCI.
- Medication review: Guidance is provided on which medicines to stop or continue before the procedure.
- Fasting: Patients typically fast for several hours before PCI.
- Consent: Information is given and written consent obtained prior to the procedure.
Living With a Stent After PCI
Having a stent usually does not restrict physical activity after recovery. Patients are advised to:
- Follow all recommended medications—especially antiplatelet drugs.
- Attend regular follow-ups for heart health monitoring.
- Adopt heart-healthy lifestyle changes: balanced diet, regular exercise, avoiding tobacco, and managing cholesterol and diabetes.
Frequently Asked Questions (FAQs)
Q: Who performs PCI?
A: PCI procedures are performed by specialized doctors called interventional cardiologists in hospital catheterization labs.
Q: Is PCI painful?
A: PCI is minimally invasive and performed under local anesthesia with relaxation medicines; most patients experience only mild discomfort, mainly at the entry site.
Q: How long does PCI take?
A: The procedure usually lasts from 30 minutes to 2 hours, depending on the number of blockages treated.
Q: What is the long-term outlook after PCI?
A: Most patients experience significant symptom relief and improved heart function. Ongoing care is essential to reduce the risk of future heart events.
Q: Can arteries re-narrow after PCI?
A: Yes, re-narrowing (restenosis) can occur, but drug-eluting stents have significantly reduced this risk. Regular monitoring and adherence to medication help minimize complications.
Q: What if I am allergic to contrast dye?
A: Let your healthcare team know before PCI. Alternative dyes or medications can be used to reduce allergic reactions.
Key Takeaways About Percutaneous Coronary Intervention
- PCI is a nonsurgical heart procedure to treat blocked arteries quickly and effectively.
- Most PCI patients recover fast and enjoy prompt symptom relief.
- The procedure is safe but carries some risks, especially in emergency settings or complex disease.
- Long-term lifestyle management and medication adherence are crucial post-PCI.
References
- https://www.yalemedicine.org/conditions/percutaneous-coronary-intervention-pci
- https://www.merckmanuals.com/professional/cardiovascular-disorders/coronary-artery-disease/percutaneous-coronary-interventions-pci
- https://www.ncbi.nlm.nih.gov/books/NBK556123/
- https://en.wikipedia.org/wiki/Percutaneous_coronary_intervention
- https://www.uabmedicine.org/specialties/percutaneous-coronary-intervention/
- https://www.youtube.com/watch?v=HOwyDph3b2c
- https://www.heartandstroke.ca/heart-disease/treatments/surgery-and-other-procedures/percutaneous-coronary-intervention
- https://www.ucsfhealth.org/treatments/percutaneous-coronary-intervention
- https://www.va.gov/COMMUNITYCARE/docs/providers/CDI/IVC-CDI-00038.pdf
Read full bio of medha deb












