PCOS and Diabetes: Understanding the Critical Connection
Explore the complex relationship between polycystic ovary syndrome (PCOS) and diabetes, including risk factors, symptoms, prevention, and treatment strategies.
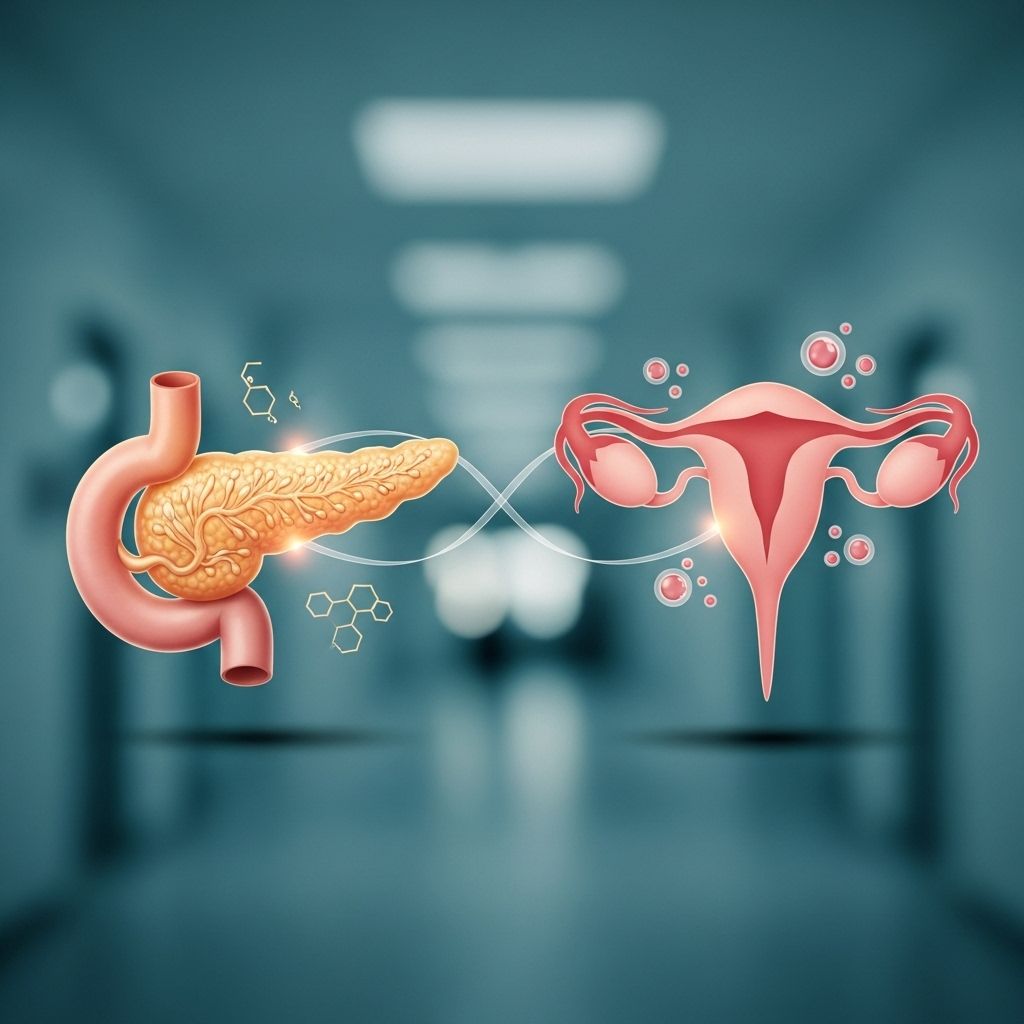
PCOS and Diabetes: Exploring the Important Link
Polycystic ovary syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age. Recent research has established significant connections between PCOS and type 2 diabetes, mainly through the shared mechanism of insulin resistance. Understanding this relationship is important for both prevention and management. This article will break down the science, risk factors, symptoms, and treatment strategies associated with these chronic conditions.
What Is PCOS?
Polycystic ovary syndrome (PCOS) is a complex hormonal disorder, affecting up to 2.2% to 26% of women globally. The wide variation in prevalence reflects differences in diagnostic criteria and population studied. PCOS commonly presents during the reproductive years and is one of the most prevalent endocrine disorders in women.
- Irregular or absent periods
- Excess androgen (testosterone and related hormones)
- Polycystic ovaries (enlarged ovaries with many small cysts)
Symptoms may also include acne, excess hair on the face or body, weight gain, infertility, and mood changes. PCOS increases the risk for several health conditions, including diabetes, heart disease, and metabolic syndrome.
Type 2 Diabetes: The Basics
Type 2 diabetes is a metabolic disorder characterized by high blood glucose (sugar) levels due to insulin resistance and/or inadequate insulin production. Diabetes is a growing public health issue, with over 38 million Americans affected by some form of diabetes, according to CDC estimates.
Type 2 diabetes is often preventable or manageable through healthy lifestyle choices, but untreated or poorly managed diabetes increases the risk of serious complications, including cardiovascular disease, kidney failure, and nerve damage.
How Are PCOS and Diabetes Connected?
The connection between PCOS and type 2 diabetes is rooted in a shared problem: insulin resistance. Insulin is a hormone produced by the pancreas that helps cells absorb glucose from the bloodstream. When the body becomes resistant to insulin, blood sugar levels rise, and the pancreas tries to compensate by making more insulin.
- Insulin Resistance: Up to 70% of women with PCOS have some degree of insulin resistance.
- Insulin resistance is a central feature of PCOS and a major risk factor for type 2 diabetes.
- High insulin levels stimulate the ovaries to produce more androgens (male hormones), worsening PCOS symptoms.
- This hormonal imbalance can trigger or accelerate the path toward developing type 2 diabetes.
Studies indicate that women with PCOS are about four times more likely to develop type 2 diabetes than women without PCOS and are diagnosed with diabetes, on average, four years earlier.
The Science Behind the Link
Although the exact mechanisms remain under investigation, researchers believe genetics, obesity, and environmental factors all influence the development of PCOS and diabetes. Some key factors include:
- Genetic predisposition: Family history of either PCOS or type 2 diabetes increases risk for both conditions.
- Obesity: Higher body mass index (BMI) strongly predicts both PCOS and type 2 diabetes.
- Insulin resistance: Present in both conditions and appears to be the common denominator linking PCOS and diabetes.
About half of women with PCOS develop type 2 diabetes by age 40.
Table: Comparing PCOS and Type 2 Diabetes
| Feature | PCOS | Type 2 Diabetes |
|---|---|---|
| Hormonal Imbalance | Yes (especially androgens) | No, unless associated with other endocrine disorders |
| Insulin Resistance | Common, often present from a young age | Primary cause and consequence |
| Main Risk Factors | Genetics, obesity, insulin resistance | Obesity, genetics, inactivity, poor diet, insulin resistance |
| Typical Age of Onset | Teens to 20s (reproductive age) | Usually after age 40, but earlier with risk factors |
| Major Symptoms | Irregular periods, hirsutism, acne, infertility | Increased thirst, frequent urination, fatigue, blurred vision |
Key Symptoms of PCOS and Diabetes
PCOS Symptoms
- Irregular or absent periods
- Excess facial or body hair (hirsutism)
- Acne, especially on the face and back
- Weight gain or difficulty losing weight
- Thinning hair on the scalp
- Infertility or difficulty ovulating
- Darkening of skin, especially around neck creases and armpits
Type 2 Diabetes Symptoms
- Increased thirst and hunger
- Frequent urination
- Fatigue
- Blurred vision
- Slow-healing sores or frequent infections
- Tingling or numbness in hands or feet
Who Is at Higher Risk?
Several risk factors increase the likelihood of developing both PCOS and type 2 diabetes:
- Family history: Having a close relative with PCOS or diabetes heightens your risk.
- Obesity: Extra body weight, especially around the belly, is linked to higher rates of both conditions.
- Ethnicity: Studies show higher rates of both PCOS and type 2 diabetes in Hispanic, African American, Native American, and South Asian populations.
- Personal history: History of gestational diabetes, metabolic syndrome, or irregular periods increases risk.
- Insulin resistance: If you are already insulin resistant, your chances are further increased.
Other Types of Diabetes and PCOS
While the relationship with type 2 diabetes is well established, PCOS can affect the risk of other diabetes types:
- Type 1 diabetes: There is some evidence that women with type 1 diabetes may have a higher risk of developing PCOS, with about 1 in 4 affected at some point.
- Gestational diabetes: Women with PCOS are more likely to develop diabetes during pregnancy. This not only increases pregnancy risks for mother and baby but can also raise the risk of developing type 2 diabetes later for both.
Testing and Diagnosis
Screening is essential for early detection and intervention. If you have PCOS, your healthcare provider should routinely check for signs of insulin resistance and diabetes:
- Fasting blood sugar
- Hemoglobin A1C (average blood sugar over 2–3 months)
- Oral glucose tolerance test if higher risk
- Regular monitoring of weight, cholesterol, and blood pressure
Prompt diagnosis enables earlier lifestyle and treatment interventions, reducing the risk for long-term complications.
Lifestyle Changes to Lower Your Risk
One of the most powerful ways to reduce your risk of diabetes if you have PCOS is through lifestyle management. Evidence shows that even small changes can produce significant results.
- Weight loss: Losing even 5% of your body weight can improve insulin sensitivity and help regulate menstrual cycles.
- Physical activity: Regular exercise, including both aerobic and strength training, helps your body use insulin more effectively.
- Healthy diet: Choose high-fiber foods, lean proteins, healthy fats, and reduce added sugars and processed foods.
- Sleep: Aim for adequate, good-quality sleep each night.
- Managing stress: Chronic stress can increase blood sugar and worsen hormones; practices like yoga, meditation, or deep breathing may help.
Medical Treatment Options
In some cases, lifestyle changes alone may not be enough. Medical therapy can target both PCOS symptoms and diabetes risk factors.
- Metformin: Originally developed for type 2 diabetes, metformin is often prescribed to women with PCOS. It improves insulin sensitivity, lowers blood sugar, and can help restore regular ovulation.
- Hormonal contraceptives: Birth control pills may be used to regulate menstrual cycles and reduce androgen levels.
- Anti-androgen medications: Sometimes used for excess hair growth or acne.
- Fertility treatments: For women struggling with infertility, ovulation-inducing medications may be considered.
Talk to your healthcare provider about which treatments may be most effective for your situation.
Living With PCOS and Diabetes Risk
Being diagnosed with PCOS can feel overwhelming, especially given the increased risk for diabetes and other serious health concerns. However, comprehensive management—combining self-monitoring, lifestyle changes, and medical intervention—can greatly improve health outcomes.
If you’re living with PCOS, prioritize open communication with your healthcare team and learn about all the available tools for prevention and treatment.
Frequently Asked Questions (FAQs)
Q: Does having PCOS mean I will definitely get diabetes?
A: Not necessarily. Although your risk is higher, especially if you have other risk factors (like obesity or family history), healthy lifestyle choices and regular screening can help prevent or delay the onset of diabetes.
Q: Should women with PCOS get tested for diabetes regularly?
A: Yes, most experts recommend regular diabetes screening for women with PCOS. Monitoring should include blood sugar testing and assessments of other metabolic risk factors.
Q: Can weight loss actually reverse symptoms?
A: For many women, even modest weight loss (as little as 5%) can significantly improve insulin sensitivity, restore ovulation, and lower the risk of developing diabetes and heart disease.
Q: Is the risk the same for all ages?
A: The risk for type 2 diabetes is highest in young adulthood for those with PCOS. Over time, if you maintain a healthy lifestyle, your risk for diabetes will become similar to that of other women your age.
Q: What can I do to protect myself if I have PCOS?
A: Focus on regular physical activity, balanced nutrition, stress reduction, and maintaining a healthy weight. Work with your healthcare provider for ongoing screening and personalized advice.
Summary: Taking Control of Your Health
The interplay between PCOS and type 2 diabetes highlights the need for awareness, proactive management, and continuous research into the underlying mechanisms driving both. By understanding risk factors, recognizing early symptoms, making healthy lifestyle choices, and pursuing appropriate medical treatment, women with PCOS can significantly lower their risk and improve quality of life.
Don’t hesitate to consult with your healthcare team about concerns or questions regarding PCOS and diabetes risk—and remember, you have the power to influence your health outcomes.
References
- https://www.healthline.com/health/diabetes/are-pcos-and-diabetes-connected
- https://www.endocrine.org/news-and-advocacy/news-room/2017/researchers-reveal-link-between-pcos-type-2-diabetes
- https://www.webmd.com/diabetes/pcos-and-diabetes
- https://www.universityhealth.com/blog/connection-between-pcos-diabetes
- https://www.cdc.gov/diabetes/risk-factors/pcos-polycystic-ovary-syndrome.html
- https://www.cedars-sinai.org/blog/pcos-diabetes-heart-disease-stroke.html
- https://www.niddk.nih.gov/health-information/professionals/diabetes-discoveries-practice/links-pcos-diabetes
- https://www.youtube.com/watch?v=B8hMIPgPBeY
Read full bio of Sneha Tete












