Percutaneous Coronary Intervention (PCI): Essential Insights for Heart Attack Treatment
Learn how percutaneous coronary intervention (PCI) saves lives by treating blocked coronary arteries and improving heart attack outcomes.
Percutaneous Coronary Intervention (PCI): Key Facts and Overview
Percutaneous coronary intervention (PCI) is a minimally invasive procedure designed to open coronary arteries that have become narrowed or blocked due to the buildup of plaque. PCI plays a crucial role in managing coronary artery disease (CAD), especially during heart attacks, and is recognized for its ability to rapidly restore blood flow to the heart muscle, reduce damage, and improve patient outcomes.
- PCI is used to treat both acute and chronic forms of coronary artery disease.
- It is often performed in emergency settings but can also be planned for patients with significant blockages.
- Commonly performed alongside angioplasty, which uses a balloon to widen the artery.
Why Is PCI Performed?
The primary goal of PCI is to relieve blockages in coronary arteries and quickly restore blood flow to the heart. Most heart attacks are caused by sudden blockage from a ruptured plaque inside a coronary artery, so timely PCI can be lifesaving.
- Reduce damage to heart muscle during a heart attack.
- Relieve chest pain (angina) and related symptoms.
- Prevent further cardiac events by opening narrowed vessels.
When Is PCI Recommended?
Clinical guidelines recommend PCI for:
- People experiencing ST-segment elevation myocardial infarction (STEMI)—a severe form of heart attack.
- Some cases of non-ST-segment elevation myocardial infarction (NSTEMI) or unstable angina.
- Individuals with high-risk coronary plaques, even if symptoms aren’t severe, as research suggests pre-emptive PCI may reduce future cardiac events.
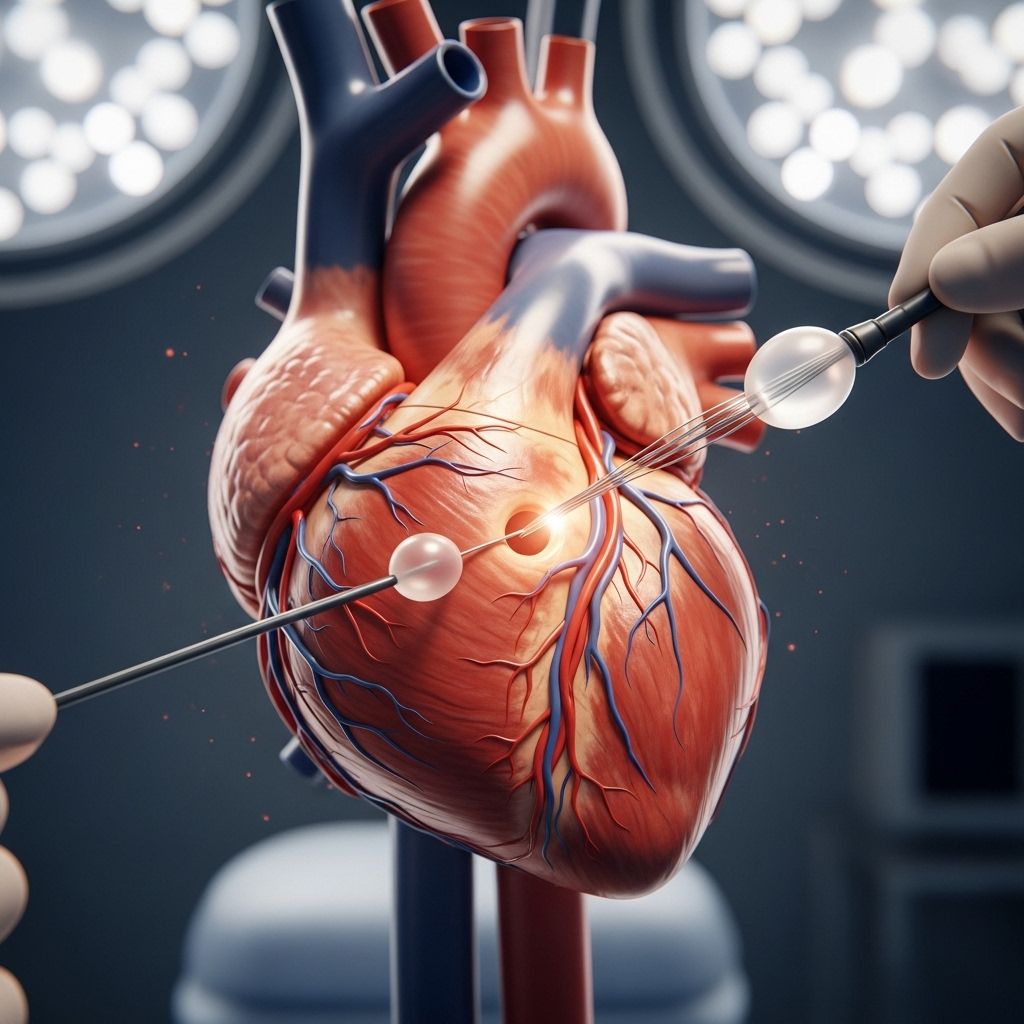
How Is PCI Performed?
PCI is considered a non-surgical procedure, carried out in a cardiac catheterization lab by an interventional cardiologist.
- A thin tube called a catheter is inserted through an artery in the groin or wrist.
- A balloon at the tip of the catheter may be inflated to widen the narrowed artery (balloon angioplasty).
- A small wire mesh tube called a stent is commonly placed to keep the artery open.
- Stents may be coated with medications (drug-eluting stents) to help prevent re-narrowing.
Most procedures take less than an hour. Patients are typically awake but sedated, and recovery times are faster than traditional surgery.
Step-by-Step Process of PCI
- Preparation with blood thinners and sedation.
- Catheter insertion and navigation to the blocked artery using x-ray guidance.
- Balloon inflation widens the vessel; stent placement ensures long-term patency.
- Removal of catheter and closure of access site.
Types of PCI Procedures
| Type | Description | Typical Use |
|---|---|---|
| Balloon Angioplasty | Balloon tipped catheter is inflated to compress plaque and widen artery. | Often first step before stent placement. |
| Stent Placement | Wire mesh tube inserted to keep artery open. May be drug-coated. | Most common; reduces risk of re-narrowing. |
| Preventive PCI | Proactive stenting of plaques at high risk of rupture, regardless of symptoms. | For patients with vulnerable plaques, emerging area per PREVENT trial. |
Who Should Get PCI?
PCI is widely recommended for individuals who:
- Are experiencing an acute heart attack (STEMI or unstable CAD).
- Have significant blockages not amenable to medical therapy alone.
- Show evidence of ischemia (lack of oxygen to heart tissue).
- May benefit from stabilizing high-risk plaques before symptoms arise.
The risk and potential benefit of PCI are evaluated based on individual patient factors, including anatomy of coronary disease, overall health, and timing from symptom onset.
Benefits of PCI for Heart Attack and CAD
PCI is lifesaving in heart attack settings. Clinical trials and meta-analyses show the following benefits:
- Increased survival rates in acute heart attack (especially STEMI).
- Reduced mortality, cardiac death, and recurrence of heart attack in unstable coronary artery disease.
- Decreases in persistent chest pain (angina).
- Rapid recovery compared to open heart surgery.
A meta-analysis of randomized trials found that PCI significantly decreased deaths in patients with unstable CAD, but did not change death or heart attack rates in patients with stable CAD.
PCI for Preventing Future Cardiac Events
- Recent studies (PREVENT trial) suggest that preventive stenting of high-risk plaques lowers the chance of severe cardiac events in asymptomatic but high-risk patients.
PCI vs. Medical Therapy Alone
Extensive research compares PCI to medical management:
- Unstable CAD (acute settings): PCI adds survival benefit over medical therapy.
- Stable CAD: Trials (COURAGE, ISCHEMIA, FAME-2) show no major difference in heart attack or death rates between PCI plus medication and medication alone.
- Angina relief: PCI offers faster and greater reduction in chest pain than medication alone.
Risks and Potential Complications of PCI
Though PCI is generally safe, there are some risks:
- Bleeding at the catheter insertion site.
- Allergic reactions to contrast dye used during imaging.
- Damage to the artery or the heart itself.
- Rarely, heart attack, stroke, or death can occur during the procedure.
- Blood clots forming in or around the stent after placement (requires blood thinners).
After PCI: Recovery and What to Expect
Recovery after PCI is usually quick:
- Most patients leave the hospital within 1–2 days of the procedure.
- Return to regular activities within a week, unless complications arise.
- Careful monitoring for chest pain, bleeding, or signs of infection at the catheter site.
- Prescription medications to prevent clotting and promote vessel healing (such as aspirin, clopidogrel).
Long-term lifestyle changes—including healthy diet, exercise, and smoking cessation—are recommended to maintain heart health after PCI.
Recent Research and Clinical Trials
Key studies and trials shaping current PCI guidelines and practice include:
- COURAGE Trial: Found no significant difference in heart attack or death rates between PCI with medical therapy and medical therapy alone in stable CAD.
- ISCHEMIA and FAME-2 Trials: Noted greater angina relief for PCI, but no difference in major outcomes for stable CAD.
- PREVENT Trial: Largest study on preventive PCI in high-risk plaques, showing an 89% reduction in major cardiac events over two years compared to medication alone.
These findings emphasize the value of PCI in unstable or acute settings, and ongoing exploration for preventive approaches in select high-risk patients.
Frequently Asked Questions (FAQs) About PCI
What is PCI and when is it used for heart attacks?
PCI is a minimally invasive procedure to open blocked coronary arteries and restore blood flow during a heart attack or severe angina attack.
Is PCI always needed for heart attacks?
No. PCI is especially crucial in acute heart attack settings (STEMI). In stable CAD or mild symptoms, medical therapy may suffice and PCI might not improve survival.
What are the main risks of PCI?
Most common risks include bleeding, allergic reactions to contrast dye, vessel damage, and possibly clotting at the stent site. Life-threatening complications are rare.
How long is recovery after PCI?
Most people recover rapidly, resuming normal activities within a week. Careful monitoring and medication adherence are vital for stent success and heart health.
Does PCI cure coronary artery disease?
PCI treats the immediate blockage but does not cure the underlying disease. Ongoing lifestyle adjustments and medication are needed to manage cardiovascular risk.
Key Takeaways
- PCI is lifesaving for heart attack and unstable coronary artery disease, notably for those with acute symptoms or high-risk plaques.
- For stable CAD, PCI is primarily used to relieve symptoms (angina), not to improve survival.
- Pre-emptive PCI targeting vulnerable plaques is an emerging strategy with positive early research results.
- Risks are low but present; individualized decision-making based on clinical guidelines and patient health is essential.
- Recovery from PCI is generally fast, but long-term heart health requires ongoing medical and lifestyle care.
Further Resources
- American Heart Association – Guidelines on PCI and heart attack care
- Latest clinical trials and meta-analyses – For insights into stable and unstable CAD treatment outcomes
- Patient support communities – For education on recovery and living with CAD
References
- https://www.healthline.com/health/heart-attack/pci-for-heart-attack
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10547354/
- https://www.acc.org/About-ACC/Press-Releases/2024/04/08/14/42/preventive-percutaneous-coronary-intervention-for-high-risk-coronary-plaques-reduces-cardiac-events
- https://www.ahajournals.org/doi/10.1161/CIRCOUTCOMES.119.006363
- https://www.healthline.com/health/heart/percutaneous-coronary-intervention
- https://www.medicalnewstoday.com/articles/pci-coronary-artery-disease
- https://www.ncbi.nlm.nih.gov/books/NBK556123/
- https://www.medicalnewstoday.com/articles/184130
- https://www.heartandstroke.ca/heart-disease/treatments/surgery-and-other-procedures/percutaneous-coronary-intervention
Read full bio of Sneha Tete












