Parasitic Infections of the Skin: Causes, Symptoms, and Treatments
Explore the causes, symptoms, risk factors, and treatments for common parasitic skin infections and learn how to protect yourself and your community.
Parasitic Infections of the Skin: Causes, Symptoms, Diagnosis, and Treatment
Parasitic skin infections are a group of conditions caused by parasites—organisms that live on or within another organism, often causing harm to their host. Although parasitic skin diseases are most common in tropical climates and resource-limited settings, they can affect anyone, anywhere in the world. Understanding the types, symptoms, diagnosis, and treatment of these infections is crucial for effective management and prevention.
What Are Parasitic Skin Infections?
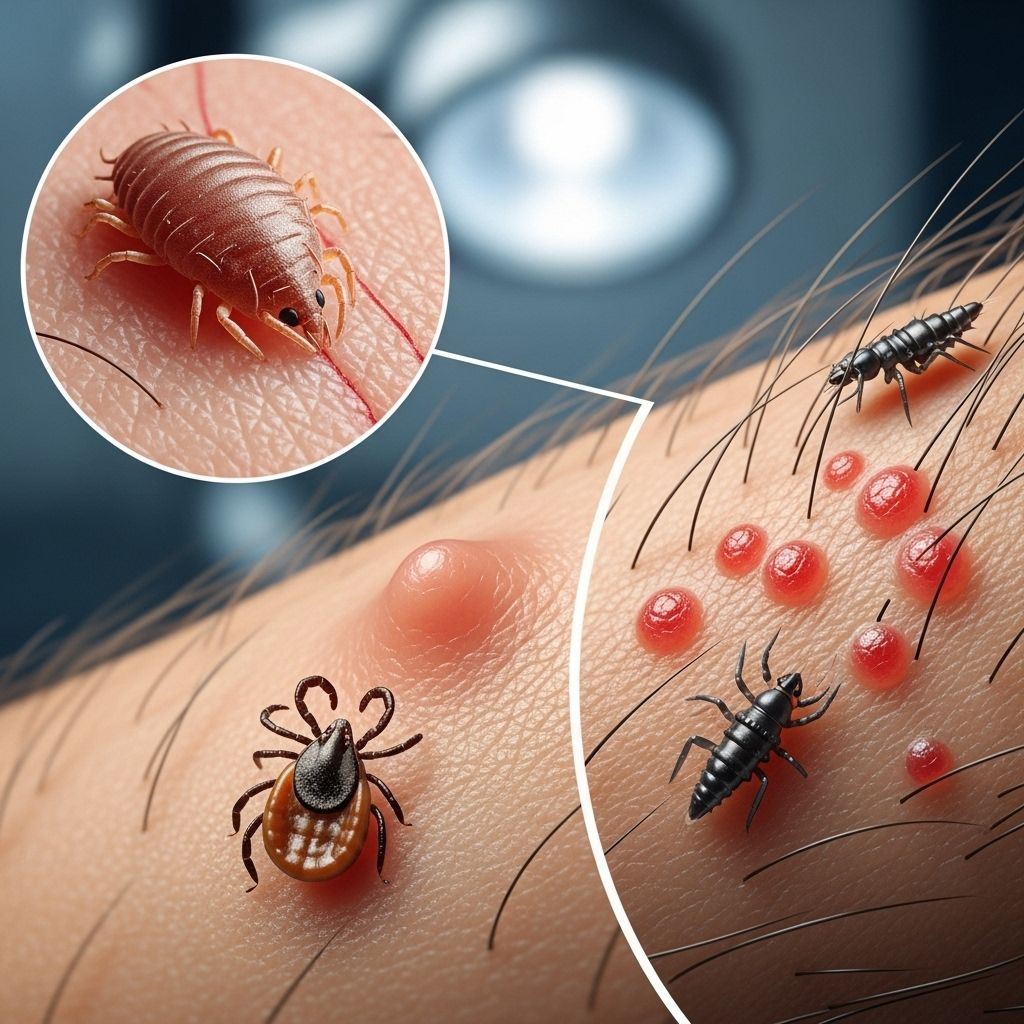
Parasitic skin infections arise when various types of parasites invade or inhabit the skin. These parasites may be protozoa (single-celled organisms), helminths (worms), or arthropods (insects and arachnids). Each has distinct characteristics, modes of transmission, and preferred environmental conditions. The resulting infections display a wide array of symptoms, ranging from mild irritation to severe inflammation and systemic complications.
- Protozoa: Examples include Leishmania species, which cause cutaneous leishmaniasis.
- Helminths: Worm-like parasites such as hookworms and filarial worms (e.g., Loa loa causing loiasis).
- Arthropods: Insects or mites such as scabies mites (Sarcoptes scabiei), head lice, and body lice.
These infections are widespread and can be found in all continents, although their prevalence is higher in certain geographic and socioeconomic contexts.
Types of Parasitic Skin Infections
The principal parasitic skin diseases include:
- Scabies
- Pediculosis capitis (head lice)
- Cutaneous larva migrans (from hookworm larvae)
- Cutaneous leishmaniasis
- Loiasis
| Infection Type | Primary Cause | Key Symptoms | Geographical Distribution |
|---|---|---|---|
| Scabies | Sarcoptes scabiei mite | Intense itching, rash, skin burrows | Worldwide, more common in crowded settings |
| Head Lice | Pediculus humanus capitis | Itching scalp, visible lice/nits | Global, especially in children |
| Cutaneous Larva Migrans | Hookworm larvae | Creeping eruption, serpiginous rash, intense itching | Tropical, subtropical regions |
| Cutaneous Leishmaniasis | Leishmania protozoa | Chronic skin ulcers, papules or nodules | Middle East, Africa, Central & South America |
| Loiasis | Loa loa filarial worm | Calabar swelling, migrating worm under skin | Central & West Africa |
Symptoms of Parasitic Skin Infections
Symptoms can range from mild to severe and often depend on the type of parasite and the host’s immune status. Common symptoms include:
- Itching (pruritus), often severe and persistent
- Redness (erythema)
- Rash and localized swelling
- Formation of papules, nodules, or ulcers
- Visible burrows or tracks in the skin (scabies, cutaneous larva migrans)
- Hair loss (pediculosis capitis)
- Secondary bacterial infection from scratching
Some infections, such as loiasis, may cause systemic symptoms depending on the stage and extent of disease. In children, multiple infestations can occur simultaneously, and polyparasitism may signal neglect or living in unhygienic conditions.
Causes and Transmission
Parasitic skin infections are generally caused by direct skin contact with the parasite or its eggs, exposure to contaminated surfaces or soil, or transmission through insect vectors. Routes of transmission include:
- Direct contact: Sharing bedding, towels, or clothing with an infested person (e.g., scabies or lice).
- Environmental exposure: Walking barefoot on contaminated soil (e.g., cutaneous larva migrans), or exposure to infested water.
- Vector-borne: Bites from infected sandflies (leishmaniasis) or blackflies (onchocerciasis).
Risk Factors
Certain populations and behaviors are at higher risk for acquiring parasitic skin infections. Common risk factors include:
- Living in or traveling to endemic regions
- Poor personal hygiene or lack of access to clean water
- Crowded living conditions (e.g., shelters, schools, prisons)
- Poverty and insufficient healthcare infrastructure
- Direct contact with infested individuals or animals
- Children (more susceptible due to close contact and play behaviors)
- Outdoor activities that involve skin contact with contaminated soil or sand
Diagnosis
Diagnosis is based on a combination of clinical examination, patient history, and, in some cases, laboratory testing. Important steps include:
- History of recent travel, exposure, or outbreaks in close settings
- Visual identification of signs (e.g., live lice, burrows, characteristic rashes)
- Dermatological examination for pathognomonic features
- Microscopic identification of parasites from skin scrapings or tissue samples
- Serological tests or PCR (for some protozoal and helminthic infections)
In many settings, diagnosis remains clinical, especially in resource-limited areas without advanced laboratory facilities.
Treatment of Parasitic Skin Infections
The primary goals of treatment are eradication of the parasite, relief of symptoms, prevention of complications and transmission, as well as improving the patient’s quality of life. Treatment often involves a combination of pharmacological and non-pharmacological measures:
Pharmacological Measures
- Scabicides and pediculicides: Permethrin, Ivermectin, Lindane – for scabies and lice
- Antiprotozoal agents: Sodium stibogluconate, Amphotericin B, Miltefosine – for cutaneous leishmaniasis
- Antiparasitic medications: Diethylcarbamazine (DEC), Albendazole – for helminthic infections
Choice of medication depends on the specific parasite and host factors, including age, pregnancy status, and severity of symptoms.
Non-Pharmacological Measures
- Mechanical or manual removal of parasites (e.g., lice or larvae)
- Topical treatments: lotions, shampoos, corticosteroids to manage itching and inflammation
- Wound care to address secondary bacterial infections or ulcers
- Isolation measures in institutional outbreaks to prevent spreading
- Personal hygiene improvements (regular bathing, laundering bedding/clothes)
Prevention
Preventing parasitic skin infections involves public health strategies, personal hygiene practices, and behavioral modifications:
- Maintaining good personal and household hygiene
- Regular laundering and cleaning of clothing, bedding, and living areas
- Avoiding direct contact with infested individuals, bedding, or clothing
- Using insect repellents and protective clothing in areas with vector-borne risks
- Educating communities on symptoms and prevention practices
- Prompt identification and treatment of cases to prevent outbreaks
- Wearing shoes in areas where hookworm or other soil parasites are common
Complications
- Chronic skin ulceration or disfiguring scars (especially in cutaneous leishmaniasis)
- Secondary bacterial infections from scratching or open lesions
- Spread to other household or community members
- Impaired quality of life due to itching, discomfort, and sleep disturbances
- Stigma and social isolation, particularly for visible or persistent infections
Outlook and Prognosis
With timely and effective diagnosis and treatment, most parasitic skin infections resolve without permanent complications. However, in areas with limited healthcare infrastructure or ongoing outbreaks, repeat and chronic infections can negatively impact social, academic, and occupational functioning.
Frequently Asked Questions (FAQs)
What is the most common parasitic skin infection?
Scabies and head lice are some of the most widespread parasitic skin infections globally, affecting millions of people in both developed and developing countries.
Are parasitic skin infections contagious?
Many such infections are highly contagious, particularly scabies and lice, which spread through direct human contact or shared personal items.
Can parasitic skin infections resolve without treatment?
Some mild infestations (like a few lice) may resolve, but most require medical treatment, especially to prevent spreading and complications.
Is it possible to prevent all parasitic skin infections?
Complete prevention can be challenging, but strict hygiene, personal awareness, and prompt treatment minimize risks significantly.
When should someone see a doctor?
If there is persistent itching, a rash, unexplained skin changes, or signs of infestation, consult a healthcare provider for proper diagnosis and management.
Key Takeaways
- Parasitic skin infections are caused by a wide range of organisms and are prevalent across different regions and settings.
- Common types include scabies, pediculosis capitis, cutaneous larva migrans, cutaneous leishmaniasis, and loiasis.
- Symptoms range from itching and rash to skin ulcers, with a risk of complications like secondary infections if untreated.
- Diagnosis relies on clinical examination, history, and laboratory testing when available.
- Treatment is multi-faceted, involving medication, hygiene, and wound care. Resistance and toxicity of some drugs are growing concerns.
- Prevention hinges on hygiene, prompt treatment, and public health measures.
References
- https://www.chi.gov.sa/Style%20Library/IDF_Branding/Indication/191%20-%20Parasitic%20Skin%20Infection-Indication%20Update.pdf
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4204056/
- https://www.healthline.com/health/skin-infection
- https://my.clevelandclinic.org/health/diseases/24885-parasitic-infection
- https://my.clevelandclinic.org/health/diseases/24911-parasites
- https://www.ppsd.com/dermatology/conditions-treated/parasitic-infections/
- https://libguides.mskcc.org/infectiousdiseases/ParasiticInfections
- https://www.news-medical.net/health/Parasitic-Skin-Infestations.aspx
Read full bio of medha deb












