Paraneoplastic Syndromes and Lung Cancer: Causes, Symptoms, and Treatment
Comprehensive guide to paraneoplastic syndromes in lung cancer, including causes, symptoms, risks, types, and modern treatments.
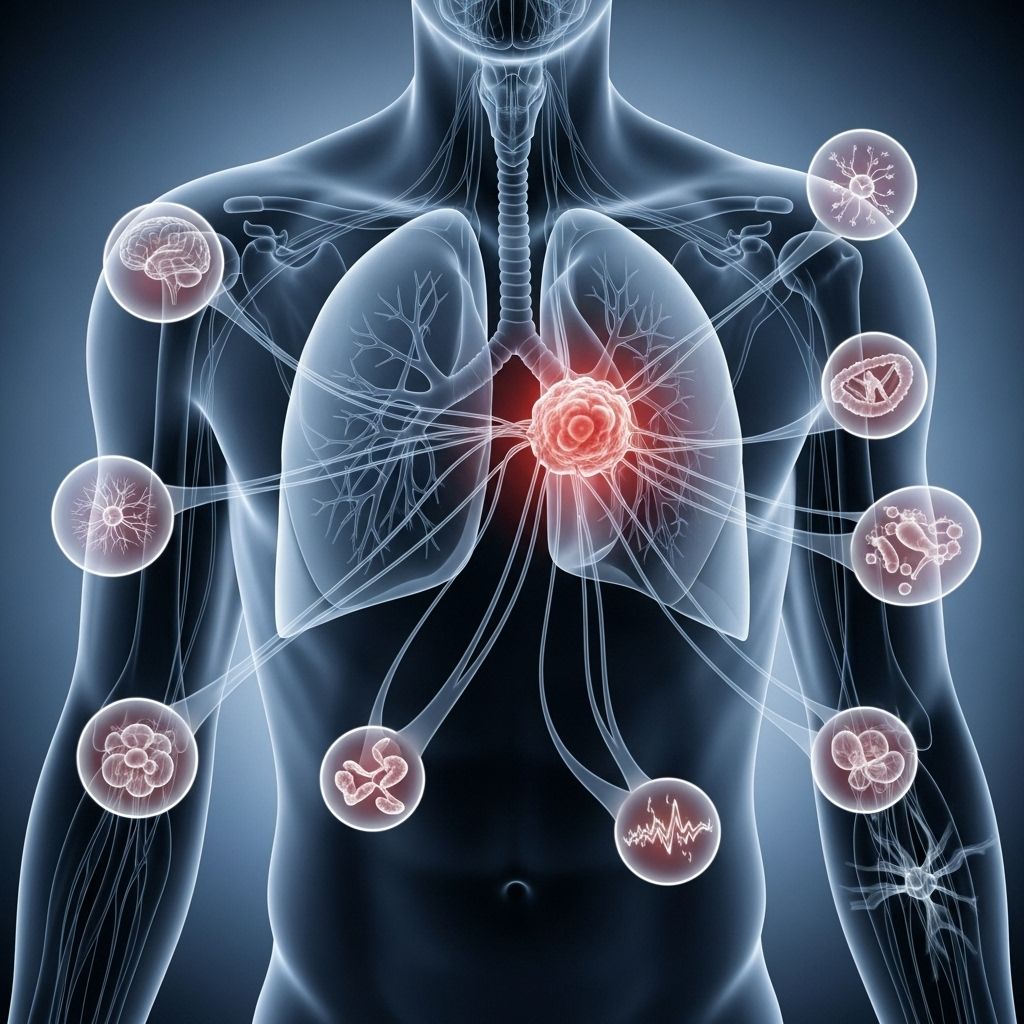
Paraneoplastic syndromes are a complex group of rare disorders that can affect people with cancer, especially lung cancer. Unlike symptoms caused by direct tumor invasion or metastasis, paraneoplastic syndromes result from immune system responses or substances secreted by tumors, impacting areas of the body far from the actual cancer site. Understanding, recognizing, and treating paraneoplastic syndromes is essential for improving outcomes and quality of life in those with lung cancer.
What Are Paraneoplastic Syndromes?
Paraneoplastic syndromes are rare complications linked to cancer where symptoms arise due to the body’s immune response or substances released by the tumor, rather than the local effects of the tumor itself. These responses can cause systemic symptoms affecting organs and tissues throughout the body.
- They occur as a result of the body’s immune system attacking normal tissues due to shared antigens with the tumor.
- The tumor may secrete hormones, cytokines, or autoantibodies, disrupting normal bodily functions.
- Symptoms can affect the endocrine, nervous, skin, blood, or other systems.
How Does Lung Cancer Cause Paraneoplastic Syndromes?
Lung cancer, especially small cell lung cancer (SCLC), is the cancer type most frequently linked to paraneoplastic syndromes. These occur when cancer cells either provoke the immune system to attack normal tissues or produce substances (like hormones or cytokines) that disrupt body functions.
- Immune-Mediated Mechanisms: The immune system forms antibodies or T cells that react not just against the tumor but also against healthy tissues.
- Secretion of Substances: Tumor cells can release hormones, peptides, or cytokines, causing metabolic or hormonal imbalances.
- Remote Effects: Symptoms appear in parts of the body distant from the primary tumor or its metastases.
Early recognition is crucial, as paraneoplastic syndromes may actually be the first sign of lung cancer in some people, appearing before the tumor is discovered.
Who Is at Risk for Paraneoplastic Syndromes?
Paraneoplastic syndromes can develop in a significant minority of people with cancer, but specific factors increase the risk:
- Having lung cancer (especially small cell type)
- Age: More common in middle-aged or older adults
- Other cancers: Risk exists in cancers of the breast, ovary, lymphatic system, and others, but lung cancer is the leading cause
- Both men and women are affected equally
- Estimated frequency in cancer patients: 8% to 20%
Types of Paraneoplastic Syndromes in Lung Cancer
Paraneoplastic syndromes can be grouped based on the body systems they affect. The most common syndromes associated with lung cancer include:
- Endocrine (hormonal) syndromes
- Neurologic (nervous system) syndromes
- Hematologic (blood) syndromes
- Dermatologic (skin) syndromes
- Rheumatologic (joints and connective tissue) syndromes
- Ophthalmologic (eye) syndromes
- Glomerulopathy and Coagulopathy (kidney and clotting disorders)
Common Paraneoplastic Syndromes by Lung Cancer Type
| Lung Cancer Type | Associated Paraneoplastic Syndromes |
|---|---|
| Small cell lung cancer (SCLC) |
|
| Squamous cell carcinoma |
Paraneoplastic syndromes not only influence cancer patients but also highlight the tumor's broader impact on the body. For a closer examination of how lung cancer can affect various bodily functions, it’s valuable to learn about the comprehensive effects of lung cancer on the body. |
| Other types (adenocarcinoma, etc.) |
|
Symptoms of Paraneoplastic Syndromes
The specific symptoms depend on the type of paraneoplastic syndrome and the body system involved. These symptoms often develop suddenly and may precede the diagnosis of lung cancer. Common symptoms include:
- Endocrine Symptoms: Hyponatremia (low sodium), high calcium levels, weakness, fatigue, muscle cramps, confusion
- Neurologic Symptoms: Seizures, confusion, difficulty walking, muscle weakness, numbness, tingling, memory problems
- Hematologic Symptoms: Anemia, unusual clotting, bleeding disorders
- Dermatologic Symptoms: Skin rashes, itching, darkened skin patches
- General Symptoms: Fever, night sweats, unexplained weight loss, appetite loss, sleep disturbances, high blood pressure, dizziness, speech difficulties
Even mild symptoms should be evaluated, as early detection is crucial for effective management.
Specific Paraneoplastic Syndromes in Lung Cancer
Endocrine Paraneoplastic Syndromes
- Syndrome of Inappropriate Antidiuretic Hormone Secretion (SIADH): Tumor produces antidiuretic hormone, causing water retention, low sodium, confusion, muscle cramps, and sometimes coma.
- Cushing’s Syndrome: Overproduction of ACTH from tumor cells, leading to weight gain, high blood pressure, thin skin, and excessive body hair.
- Hypercalcemia of Malignancy: Tumor secretes parathyroid hormone-related peptide (PTHrP), causing high calcium levels, kidney stones, abdominal pain, and psychiatric changes.
Neurologic Paraneoplastic Syndromes
- Lambert-Eaton Myasthenic Syndrome (LEMS): Autoimmune attack on nerve-muscle junctions leads to muscle weakness, especially in the legs, and sometimes affects swallowing or speech.
- Paraneoplastic Cerebellar Degeneration: Autoimmune attack on cerebellar tissue causes poor coordination, unsteadiness, tremor, vertigo, and speech difficulties.
- Other Neurologic Syndromes: Sensory neuropathies, encephalitis, stiff person syndrome.
Other Paraneoplastic Syndromes
- Hematologic: Anemia, thrombocytosis (too many platelets), or increased risk of blood clots (Trousseau’s syndrome).
- Dermatologic: Acanthosis nigricans (dark, velvety skin), dermatomyositis (muscle weakness and skin rash), other rare skin changes.
- Rheumatologic: Joint pain, muscle inflammation.
- Ophthalmologic: Double vision, visual changes due to nerve involvement.
- Renal/Coagulopathy: Glomerulopathies (kidney disease), coagulopathies (clotting abnormalities).
What Causes Paraneoplastic Syndromes?
Paraneoplastic syndromes are triggered by either immunologic or nonimmunologic mechanisms prompted by the presence of a cancerous tumor.
- Immunologic: The immune system forms antibodies or immune T-cells to tumor antigens that cross-react with normal tissue antigens, leading to tissue damage.
- Nonimmunologic: Substances (hormones, cytokines, peptides) are secreted by the tumor or by surrounding tissues in response to the tumor.
Not all people with lung cancer will develop a paraneoplastic syndrome, and there is no clear way to predict who will be affected.
How Are Paraneoplastic Syndromes Diagnosed?
Diagnosing a paraneoplastic syndrome in someone with or without a known cancer history can be challenging. Physicians may suspect a syndrome due to the presence of unexplained symptoms, often preceding a cancer diagnosis.
- Medical History and Physical Examination: Comprehensive review of neurological, endocrine, and other systemic symptoms.
- Blood Tests: Measurement of sodium, calcium, hormone levels, tumor markers, and detection of autoantibodies.
- Imaging Studies: CT, MRI, or PET scans to search for underlying tumors in lungs or elsewhere in the body.
- Specialized Tests: Lumbar puncture (spinal tap) for neurological symptoms, urine tests, or skin and tissue biopsies as needed.
It is vital to distinguish symptoms of paraneoplastic syndromes from other medical conditions with similar appearances.
Treatment for Paraneoplastic Syndromes
The cornerstone of managing paraneoplastic syndromes lies in treating the underlying cancer. Being able to control or remove the tumor often leads to improvement or resolution of the syndrome. Common treatment strategies include:
- Direct Cancer Treatment: Surgery, chemotherapy, radiation, or targeted therapies aimed at shrinking or removing the tumor.
- Immunosuppressive Therapy: Corticosteroids (like prednisone), intravenous immunoglobulin, or plasmapheresis to calm abnormal immune responses in neurologic or autoimmune syndromes.
- Supportive Care: Medications to control hormone imbalances, electrolyte corrections (for sodium or calcium), anticonvulsants for seizures, or physical therapy for muscular or neurological symptoms.
- Symptom-Specific Intervention: Drugs to counteract hormone overproduction, anti-clotting medications if necessary, pain management, and nutritional support.
Early diagnosis and prompt treatment of both the underlying cancer and the paraneoplastic syndrome can significantly improve symptoms and outcomes.
What Is the Outlook for People with Paraneoplastic Syndromes?
Prognosis largely depends on the type and stage of lung cancer as well as the specific paraneoplastic syndrome involved. Other factors influencing outlook include:
- Type of syndrome: Some, like SIADH or hypercalcemia, can be life-threatening if untreated.
- Timeliness of diagnosis: Early recognition allows prompt management of both the syndrome and cancer, improving outcomes.
- Response to treatment: Paraneoplastic syndromes often improve when the underlying cancer is controlled, but some neurological syndromes can have lasting effects even after the tumor is removed.
Supportive care, symptom management, and a multidisciplinary team approach are essential for optimizing quality of life and survival.
Living With Paraneoplastic Syndromes
Living with a paraneoplastic syndrome can be challenging, especially when facing the broader context of lung cancer treatment. Resources and strategies that may help include:
- Open communication with your medical team
- Joining cancer support groups for shared experiences
- Utilizing mental health support for emotional well-being
- Maintaining good nutrition and a balanced lifestyle
- Following all prescribed medications and therapies strictly
- Monitoring and reporting new or worsening symptoms promptly
Frequently Asked Questions (FAQs)
What is the main cause of paraneoplastic syndromes in lung cancer?
Paraneoplastic syndromes in lung cancer are mainly caused by either the immune system responding abnormally to the tumor or by hormones, cytokines, or other substances released by the tumor that disrupt normal body functions.
Which type of lung cancer is most often linked to paraneoplastic syndromes?
Small cell lung cancer is most frequently associated with paraneoplastic syndromes, but some syndromes (like hypercalcemia) are more common with certain non-small cell types, such as squamous cell carcinoma.
Can paraneoplastic syndromes be cured if lung cancer is treated?
Many paraneoplastic syndromes improve or resolve when the underlying tumor is effectively treated. However, in some cases, neurological damage may not fully reverse even after cancer control.
Are paraneoplastic syndromes reversible?
Some are reversible if treated early and cancer is controlled, particularly hormonal and some immune syndromes. Persistent neurological damage can be irreversible in some patients despite treatment.
What should I do if I have new or unexplained symptoms and a lung cancer diagnosis?
Report all new, unexplained, or worsening symptoms to your healthcare provider as soon as possible, as they could signal a paraneoplastic syndrome or other complication needing prompt attention.
References
- https://www.mylungcancerteam.com/resources/paraneoplastic-syndromes-and-lung-cancer
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4127595/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7656388/
- https://www.pulmonologyadvisor.com/ddi/paraneoplastic-syndromes/
- https://www.webmd.com/lung-cancer/paraneoplastic-syndromes-small-cell-lung-cancer
- https://my.clevelandclinic.org/health/diseases/17938-paraneoplastic-syndromes
- https://atm.amegroups.org/article/view/26458/html
- https://www.mayoclinic.org/diseases-conditions/paraneoplastic-syndromes/symptoms-causes/syc-20355687
- https://www.merckmanuals.com/home/cancer/overview-of-cancer/paraneoplastic-syndromes
Read full bio of Sneha Tete












