Pancoast Tumors and Horner Syndrome: Understanding the Connection
Explore the link between Pancoast tumors and Horner syndrome, examining signs, diagnosis, and current treatment strategies.
Pancoast Tumors and Horner Syndrome: How Are They Connected?
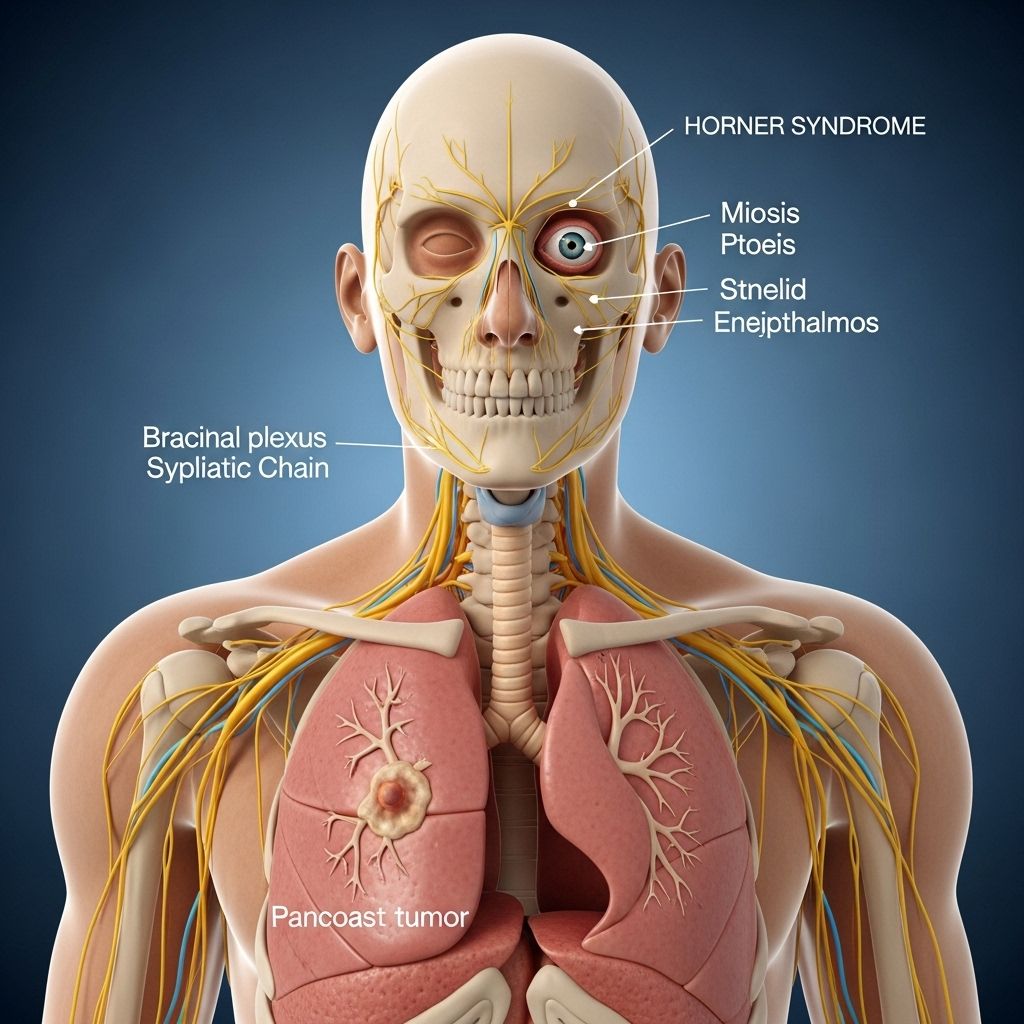
Pancoast tumors represent a unique and rare form of lung cancer that develops at the apex (top segment) of either lung. These tumors are noteworthy not only for their location but for the symptoms they produce, which differ significantly from those seen in more central lung cancers. Among their distinctive clinical features is their link to Horner syndrome—a rare neurological condition reflecting disruption of certain nerve pathways that control the face and eye.
What Are Pancoast Tumors?
Pancoast tumors, sometimes referred to as superior sulcus tumors, arise at the top of a lung near the thoracic inlet. Because of their anatomical position, they are likely to invade adjacent structures before spreading elsewhere in the body.
- Location: Apex (top) of the lung, near major nerves and blood vessels
- Type: Most are classified as non-small cell lung carcinoma (NSCLC)
- Distinguishing features: Early involvement of local nerves, rather than initial lung symptoms
This unique positioning means Pancoast tumors often do not produce classic lung cancer signs, such as chronic cough or shortness of breath. Instead, they may first affect other anatomical structures, chiefly the nerves running close to the lung apex.
What Is Horner Syndrome?
Horner syndrome is a neurological disorder that results when the sympathetic nerve pathway to the face and eyes is damaged. The syndrome manifests through a distinctive group of symptoms:
- Ptosis: Drooping of the upper eyelid on the affected side
- Miosis: Constricted pupil in one eye (making pupils appear unequal in size)
- Anhidrosis: Reduced or absent sweating on one side of the face
- Occasionally, facial flushing due to disrupted nerve signals
The syndrome affects only the side of the face corresponding to the location of the underlying problem, often mirroring the side where a Pancoast tumor is present.
Why Do Pancoast Tumors Cause Horner Syndrome?
The relationship between Pancoast tumors and Horner syndrome revolves around anatomy. The lung’s apex is closely situated to the sympathetic nervous system pathways that extend from the brainstem, down the neck, and into the face. When a tumor develops in this region, it can either compress or directly invade these nerve bundles, leading to Horner syndrome.
- Brachial plexus involvement: This network of nerves controls sensations and movements in the shoulder, arm, and hand. Its close location to the apex makes it vulnerable to tumor impact.
- Sympathetic chain involvement: Disruption here can manifest as Horner syndrome due to the loss of normal sympathetic input to the face and eye.
Symptoms of Horner syndrome can be among the first clues that a Pancoast tumor is present, especially since classic lung symptoms may be absent early on.
Pancoast Tumor: Signs and Symptoms
Unlike conventional lung cancers, Pancoast tumors present with a unique symptom profile driven by their anatomic proximity to nerves and vessels at the lung apex.
- Shoulder pain: Present in up to 96% of people at diagnosis, often radiating to the shoulder blade, upper back, or down the arm
- Arm pain, weakness, numbness, or tingling: From brachial plexus involvement
- Horner syndrome symptoms: Ptosis, miosis, anhidrosis, and facial flushing on one side
- Muscle atrophy or weakness in the hand: With more advanced nerve involvement
- Rarely, respiratory symptoms: Classic symptoms like cough or shortness of breath appear later or may be absent entirely
These atypical presentations can result in delayed diagnosis, as the initial symptoms may be mistaken for orthopedic or neurological conditions, including:
- Rotator cuff injuries
- Brachial plexopathy
- Cervical radiculopathy
Diagnosis: How Are Pancoast Tumors and Horner Syndrome Identified?
Timely identification is critical for both effective treatment and improved outcomes. Diagnosis typically involves a combination of clinical evaluation, imaging, and tissue sampling:
- Clinical examination: Recognizing the classic constellation of symptoms, including shoulder/arm pain and Horner syndrome signs
- Imaging studies: Chest X-ray, computed tomography (CT), and magnetic resonance imaging (MRI) are used to detect tumors located at the lung apex and assess involvement of nearby nerves and structures
- Biopsy: Tissue sampling confirms the cancer type and informs treatment decisions
Importantly, Horner syndrome is not exclusive to cancer; other conditions may produce similar symptoms, so a full diagnostic workup is essential to rule out alternative causes such as trauma, infection, or vascular disorders.
Treatment of Horner Syndrome When Associated with Pancoast Tumors
The treatment for Horner syndrome linked to Pancoast tumors centers on addressing the underlying cancer. The goal is to eradicate or control the tumor, with the hope of relieving nerve stress and restoring normal function.
Standard therapy for Pancoast tumors generally involves a multimodal approach:
- Neoadjuvant chemotherapy and radiation therapy: Administered before surgery to shrink the tumor and improve operability
- Surgical resection: Removal of the tumor if it has not extensively invaded vital structures such as above the T1 nerve root
- Adjuvant therapy: Further treatments after surgery, tailored to the individual’s response and cancer stage
Despite advancements in therapy, the presence of Horner syndrome often indicates more advanced local invasion. As such, early detection is crucial for expanding treatment options and improving the likelihood of successful surgery.
When Surgery May Be Limited
- Invasion into critical nerve roots (above T1) or major vessels reduces surgical feasibility.
- The tumor’s proximity to the spine and brachial plexus complicates complete removal without significant functional loss.
In these cases, chemotherapy and radiation may be the primary treatment modalities.
Prognosis: What to Expect
The prognosis for individuals with Pancoast tumors depends on:
- Stage at Diagnosis: Early detection increases the chances of cure or long-term control. Presence of Horner syndrome suggests more advanced, local invasion.
- Extent of Invasion: The degree to which the tumor has invaded nerves, blood vessels, or the spine significantly influences treatment success and functional outcomes.
- Response to Multimodal Therapy: Advances in combined chemotherapy, radiation, and improved surgical techniques have enhanced survival rates in recent years.
Despite these advances, the delayed diagnosis resulting from atypical symptoms remains a challenge. This underlines the importance of inclusion of Pancoast tumor in the differential diagnosis for persistent, unexplained shoulder or arm pain, especially in patients at risk for lung cancer.
Prevention & Importance of Early Recognition
As with many cancers, there are no guaranteed strategies for prevention. However, early detection of Pancoast tumors offers the best chance for successful treatment and mitigation of complications like Horner syndrome.
- Awareness: Patients and healthcare providers should be alert to non-respiratory upper chest, shoulder, or arm symptoms, particularly neurological changes.
- Risk factors: A history of smoking or occupational exposure to carcinogens increases lung cancer risk and should prompt thorough evaluation of any unexplained symptoms.
- Prompt medical attention: Early engagement with healthcare providers can expedite diagnosis and initiation of treatment before significant nerve invasion occurs.
Frequently Asked Questions (FAQs)
Q: What makes a Pancoast tumor different from other lung cancers?
A: The primary difference is their location at the top (apex) of the lung, which leads to early invasion of local nerves and vessels rather than initial lung-related symptoms.
Q: Are there any early warning signs of Pancoast tumors?
A: Common early symptoms are persistent shoulder pain, arm pain, or weakness. Respiratory symptoms like cough tend to develop later, if at all.
Q: Can Horner syndrome be reversed if the Pancoast tumor is treated?
A: It may be possible to restore some or all nerve function after successful treatment of the tumor, but outcomes vary depending on the degree and duration of nerve involvement.
Q: Is Horner syndrome always caused by a Pancoast tumor?
A: No. Horner syndrome can result from any process that disrupts the sympathetic nerve pathways to the eye, including trauma, infections, stroke, or other tumors in the neck or upper chest.
Q: How do doctors distinguish Pancoast tumors from musculoskeletal or spine problems?
A: The key is careful evaluation of symptoms, physical examination, and dedicated imaging studies to visualize the lung apex and identify any masses or nerve invasion.
Summary Table: Pancoast Tumor vs. Typical Lung Cancer Presentation
| Feature | Pancoast Tumor | Typical Lung Cancer |
|---|---|---|
| Primary Location | Apex (top) of lung | Central or peripheral lung regions |
| Initial Symptoms | Shoulder/arm pain, neurological deficits, Horner syndrome | Cough, chest pain, shortness of breath |
| Common Nerve Involvement | Brachial plexus, sympathetic chain | Less common early on |
| Detection | Often delayed due to atypical symptoms | Usually earlier, due to respiratory complaints |
References and Further Reading
- Gundepalli SG, et al. (2023). “Lung Pancoast tumor.” NCBI Bookshelf.
- Villgran VD, et al. (2023). “Pancoast syndrome.” NCBI Bookshelf.
- Moffitt Cancer Center. “Pancoast Tumor Signs & Symptoms.”
- Medical News Today. “Pancoast tumors and Horner syndrome.”
References
- https://www.healthline.com/health/lung-cancer/pancoast-tumor-horner-syndrome
- https://www.medicalnewstoday.com/articles/pancoast-tumor-horner-syndrome
- https://www.moffitt.org/cancers/pancoast-tumor/signs-symptoms/
- https://orthopedicreviews.openmedicalpublishing.org/article/143289
- https://www.ncbi.nlm.nih.gov/books/NBK482155/
- https://www.cancerresearchuk.org/about-cancer/lung-cancer/stages-types-grades/types/pancoast-tumours
- https://www.mdanderson.org/cancerwise/3-facts-about-pancoast-tumors.h00-159543690.html
- https://www.cancertherapyadvisor.com/ddi/pancoast-tumor/
Read full bio of Sneha Tete












