Pacemaker Insertion: Procedure, Recovery, and Essential Information
A comprehensive guide to pacemaker insertion, indications, the procedure itself, recovery process, and key safety concerns.
Pacemaker Insertion: What You Need to Know
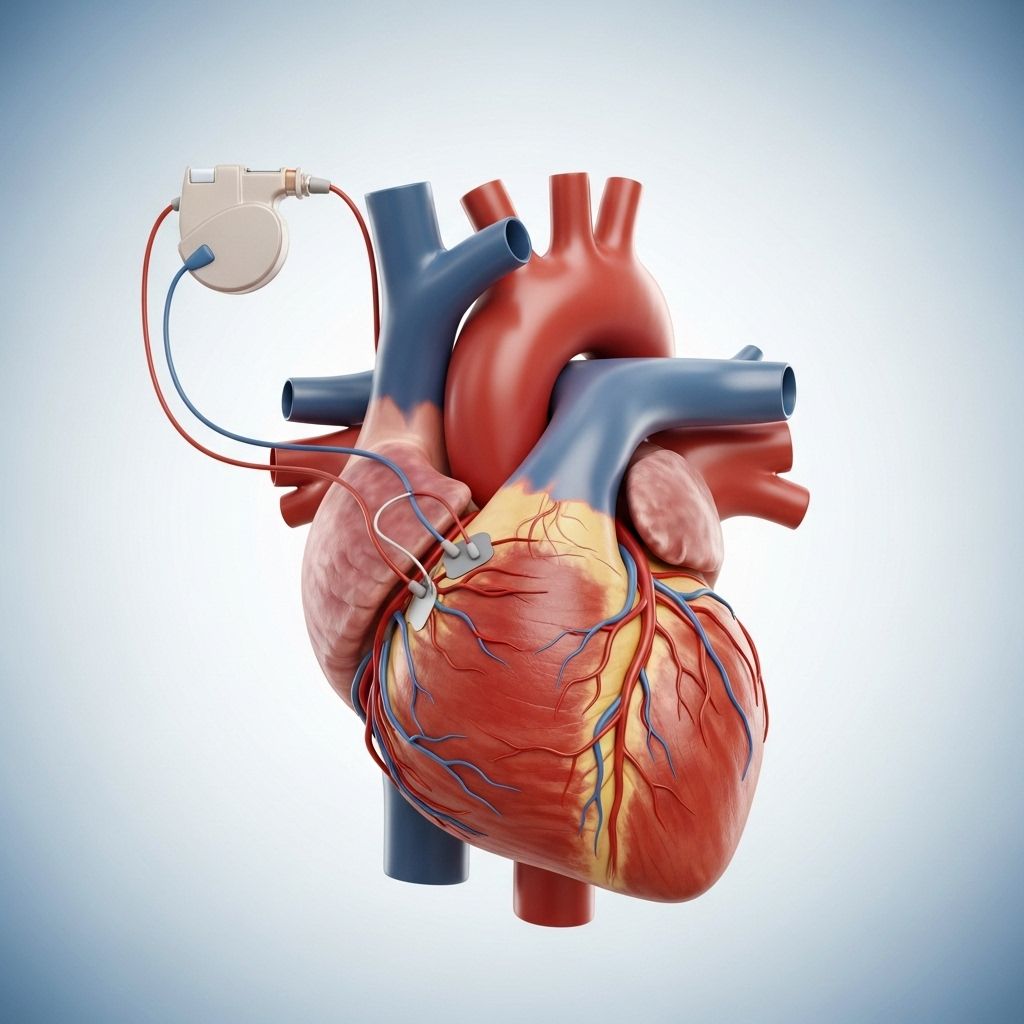
A pacemaker is a small, battery-operated device designed to help regulate heart rhythm by sending electrical impulses to the heart muscle. For many individuals with heart rhythm disorders, pacemaker insertion provides a critical and life-enhancing solution. This guide covers all aspects of pacemaker insertion—from understanding the device and its purpose to procedural details, recovery, risks, and answers to common questions.
What Is a Pacemaker?
A pacemaker is a medical device that helps maintain a steady heartbeat by transmitting electrical pulses to the heart muscle when it detects an irregular or abnormally slow heartbeat. The primary purpose of a pacemaker is to treat arrhythmias, including bradycardia (a heart rate that is too slow), and certain forms of heart block. Modern pacemakers are small, disc-shaped devices implanted under the skin, usually near the collarbone.
- Pulse generator: Contains the battery and electronic circuitry. It regulates the timing and strength of the electrical impulses.
- Leads (electrodes): Flexible wires that deliver electrical signals from the generator to the heart muscles and transmit heart signals back to the device.
- Placement: Typically inserted under the skin in the upper chest area.
Why Might You Need a Pacemaker?
Pacemaker insertion may be necessary for several heart conditions that disrupt the normal electrical signaling in the heart. Common reasons include:
- Episodes of bradycardia (a slow heartbeat that leads to fainting, weakness, or fatigue)
- Heart rhythm disorders causing the heart to beat too slowly or irregularly
- Advanced heart block or sick sinus syndrome
- Heart failure and certain forms of cardiomyopathy (weakened heart muscle)
- Recovery after heart surgery where natural electrical pathways are damaged or unreliable
Types of Pacemakers
There are several types of pacemakers, each tailored to specific patient needs and underlying heart conditions:
- Single-chamber pacemaker: Sends electrical impulses to either the right atrium or right ventricle of the heart.
- Dual-chamber pacemaker: Coordinates electrical signals between the right atrium and right ventricle to better mimic the heart’s natural rhythm.
- Biventricular pacemaker (Cardiac Resynchronization Therapy): Used for patients with heart failure, this type paces both ventricles for improved heart function.
How Does a Pacemaker Work?
The pacemaker continuously monitors the heart’s rhythm. When it detects abnormality—such as a missed beat or a slow rate—it sends a small, painless electrical pulse to stimulate the heart muscle, prompting a normal heartbeat. The device’s settings can be adjusted externally by healthcare professionals after the insertion to best suit the patient’s needs.
PACEMAKER INSERTION: THE PROCEDURE
Preparing for Pacemaker Insertion
Preparation is crucial to promote safety and ensure optimal outcomes. Your healthcare provider will give you detailed instructions specific to your situation. Preparation steps usually include:
- Reviewing your medical history and medications (including herbs or supplements)
- Blood tests and diagnostic imaging, as needed
- Fasting (no food or drink) often required after midnight prior to the procedure
- Arranging for transportation home after the procedure
- Discussion of anesthesia options and allergies
Inform your care team if you are taking blood thinners or have a bleeding disorder, as some medications may need to be adjusted before surgery.
Overview of the Procedure
Pacemaker insertion is typically performed in a specialized electrophysiology laboratory or an operating room using local anesthesia and mild sedation (so you are awake but relaxed). There are two primary techniques:
- Endocardial (transvenous) approach:
- The most common method, suitable for most adults.
- An incision is made near the collarbone.
- The leads are guided through a vein to the heart using real-time imaging.
- The lead tips are attached to specific heart chambers; the other ends connect to the pulse generator placed in a pocket under the skin.
- Epicardial approach:
- More often used in infants and children, or in adults when a transvenous approach is not possible.
- Surgery involves attaching the pacing leads directly to the outside of the heart muscle.
- Pulse generator may be placed in the abdomen.
Step-by-step outline of the endocardial pacemaker insertion:
- You are positioned on your back and connected to monitoring devices for heart rhythm, blood pressure, and oxygen.
- The skin is cleaned and sterilized; a local anesthetic is injected to numb the area.
- An incision is made below the collarbone, usually on the non-dominant side.
- Leads are inserted through a vein and guided to the appropriate area of the heart (right atrium, right ventricle, or both).
- Lead position is verified and electrical function tested (‘pacing’).
- The leads are connected to the pulse generator, which is then placed into the pocket under the skin.
- Incision is closed with sutures and a sterile dressing is applied.
The entire procedure generally takes about 1-2 hours.
For children or special cases requiring the epicardial approach, general anesthesia is used and hospital stays may be longer.
Immediately After the Procedure
After the pacemaker is implanted, your heart rhythm and vital signs will be monitored. Most patients remain in the hospital for several hours or overnight to ensure proper device function and recovery. Your healthcare team will:
- Monitor the surgical site for bleeding or swelling
- Adjust pacemaker settings as needed using an external programmer
- Provide pain medication if needed
- Review activity and care instructions
Risks and Possible Complications
Pacemaker insertion is generally safe, but as with any procedure, potential risks exist. Complications are uncommon but may include:
- Excessive bleeding or hematoma at the incision site
- Infection (at the incision site or deeper tissue)
- Pneumothorax (air around the lung)
- Movement or dislodgement of leads
- Allergic reaction to anesthesia or contrast dyes
- Damage to blood vessels or the heart muscle (rare)
- Pacemaker malfunction, such as failure to pace or sense properly
Your provider will discuss and manage individual risk factors such as advanced age, chronic illnesses (e.g., diabetes), smoking, and immune suppression.
Recovery and Aftercare
- Most patients can go home the day after pacemaker insertion; some may even go home the same day for uncomplicated procedures.
- You will need to keep the incision clean and dry, following all care instructions.
- Physical activity is restricted—avoid lifting the arm on the side of the incision above your shoulder for several weeks to prevent lead dislodgement.
- Pain, mild bruising, and swelling near the incision are normal for a few days and can be managed with prescribed medication.
- Follow-up appointments will be necessary to check wound healing and pacemaker function.
- Avoid heavy lifting, strenuous activity, or contact sports until cleared by your healthcare provider.
Avoid close or prolonged contact with strong electromagnetic fields and certain medical equipment. Notify all healthcare providers and airport security personnel that you have a pacemaker.
Living with a Pacemaker: Tips and Precautions
- Carry a pacemaker identification card and wear medical alert jewelry.
- Keep routine follow-up visits for device checks and battery monitoring.
- Avoid placing cell phones directly over the pacemaker.
- Report symptoms such as palpitations, dizziness, or syncope to your provider promptly.
- Most household appliances are safe, but stay informed about any devices that might interfere with pacemaker function.
- Remain alert for signs of infection—redness, swelling, fever, or discharge at the incision site.
When to Call Your Doctor
- Signs of infection: fever, chills, redness, swelling, or discharge from the incision
- Excessive bleeding or uncontrollable pain at the procedure site
- Chest pain, difficulty breathing, or cough
- Palpitations, extremely slow, fast, or irregular heartbeats
- A sudden feeling that your heart rate is too slow or too fast
Frequently Asked Questions (FAQs)
Q: Will I feel the pacemaker inside me?
A: You may feel a slight bulge under your skin where the pacemaker is placed, but most people quickly get used to it. Pain or discomfort usually decreases greatly within the first few days.
Q: Can I use cell phones and household appliances?
A: Yes, most common household electrical equipment is safe. Hold cell phones to the ear opposite the pacemaker and avoid placing them directly over the device. Microwave ovens and TVs do not interfere with pacemakers.
Q: How long will the pacemaker battery last?
A: Most pacemaker batteries last 5 to 15 years. Your healthcare team regularly checks the device and will schedule replacement when needed.
Q: Will having a pacemaker limit my activities?
A: After the initial recovery period, most people can return to normal, including moderate exercise, travel, and sexual activity. Some contact sports or activities involving heavy chest impact should be discussed with your doctor.
Q: What should I do before medical imaging or surgery?
A: Inform your healthcare team of your pacemaker before undergoing MRIs, CT scans, radiation therapy, or surgical procedures. Some imaging tests may require special precautions or alternative options.
Key Takeaways
- Pacemaker insertion is a common, generally safe procedure that treats irregular heart rhythms.
- Preparation, careful procedural steps, and vigilant aftercare help minimize risks.
- Most patients recover quickly and can live normal, active lives with a pacemaker.
- Know when to call your doctor or seek emergency care.
- Regular check-ups and good wound care are essential for optimal long-term results.
References
- https://www.webmd.com/heart-disease/pacemaker-implant
- https://www.upstate.edu/cardiacsurgery/surgical-procedures/pacemaker-insertion.php
- https://www.accarenthealth.com/procedure/list?patientType=ADULT&procedureTypeCode=05&procedureCode=33206A&address=21093
- https://www.pted.org/?id=pacemaker1
- https://resources.healthgrades.com/right-care/pacemakers/frequently-asked-questions-about-pacemakers
- https://www.nhlbi.nih.gov/health/pacemakers/what-to-expect
Read full bio of medha deb












