Pacemakers for AFib: When Are They Used and What Should You Know?
Understand how pacemakers are used in atrial fibrillation (AFib), including treatment goals, candidate selection, risks, and alternatives.
Atrial fibrillation (AFib) is a common heart arrhythmia that causes an irregular, often rapid heartbeat. While many treatments are available to manage AFib, pacemakers have a specific role in treating the condition, especially when accompanied by certain heart rate problems. This comprehensive guide explains when pacemakers are used in AFib, their goals, who may benefit, potential risks, and alternative treatment options.
What Is a Pacemaker?
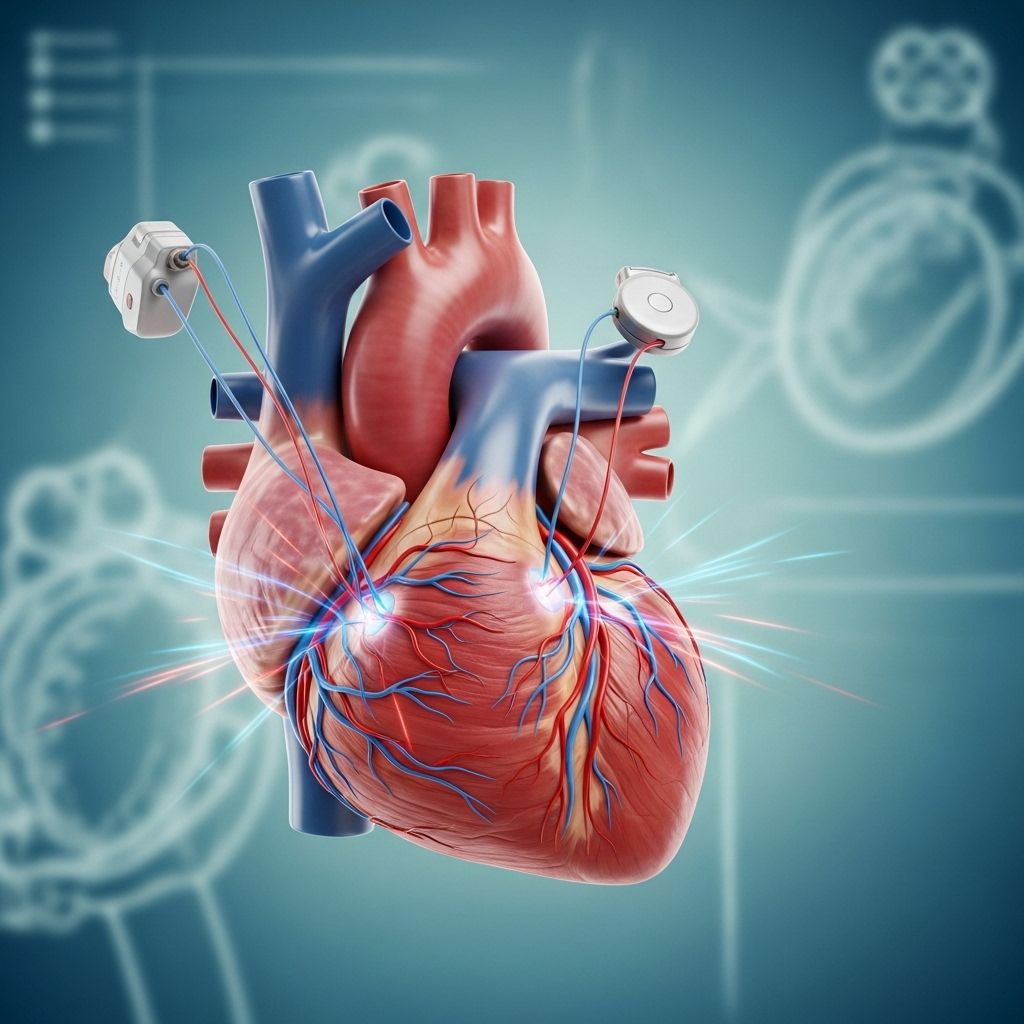
A pacemaker is a small, implantable device designed to help your heart maintain a normal rhythm and rate. Typically placed under the skin near the collarbone, it connects to your heart with thin wires called leads. These leads detect abnormal heart rhythms and send electrical impulses to restore normal heartbeats as needed.
- Size: About the size of a matchbox or slightly bigger.
- Placement: Under the skin, usually on the left side of the chest.
- Function: Monitors and regulates the heartbeat, sending signals if the heart rate drops too low or becomes irregular.
How Does a Pacemaker Help in AFib?
In AFib, the top chambers of the heart (the atria) experience chaotic electrical signals, leading to irregular heartbeats. Sometimes, this can cause the lower chambers (the ventricles) to beat too slowly, too quickly, or inconsistently—impacting how the heart pumps blood. Pacemakers are primarily used in AFib when additional rhythm issues, like slow heart rates, occur.
- Restores or maintains a steady heart rate.
- Prevents heart rate from dropping below a medically set threshold.
- Improves circulation and reduces symptoms related to low heart rate.
The pacemaker sends small electrical signals to stimulate the heart, ensuring a regular rhythm even if the heart’s own electrical system is faulty.
Treatment Goals of Using a Pacemaker in AFib
- Prevent bradycardia: Avoid episodes where the heart beats too slowly.
- Support blood circulation: Promote efficient pumping of blood to the organs.
- Enhance quality of life: Reduce symptoms like dizziness, fainting, or extreme fatigue.
- Enable use of medications: Allow patients to take medicines that may otherwise lower heart rate excessively.
When Is a Pacemaker Needed for People With AFib?
Pacemakers are not a standard treatment for all AFib cases. Doctors consider a pacemaker if AFib coexists with certain other heart rhythm problems or if other treatments have not worked. Here are the most frequent scenarios:
AFib With Symptomatic Bradycardia
When AFib is associated with bradycardia (heart rate persistently below 60 beats per minute), and this slow rate causes symptoms, a pacemaker may be needed. Common symptoms include:
- Extreme fatigue
- Dizziness or lightheadedness
- Shortness of breath
- Exercise intolerance
- Confusion or fainting
Pacemakers can prevent the heart rate from dropping too low, thereby relieving these symptoms.
Sinus Node Dysfunction
Some people with AFib experience sinus node dysfunction. This occurs when the heart’s natural pacemaker (the sinoatrial, or SA, node) does not work correctly, causing:
- Tachycardia – heart beats too fast
- Bradycardia – heart beats too slow
- Tachy-brady syndrome – alternation between fast and slow heart rhythms
A pacemaker is often used to protect against pauses or excessively slow heart rates, especially if medications required for AFib management slow the heartbeat too much.
AV Node Ablation With Pacemaker Support
In certain difficult AFib cases, doctors may perform an atrioventricular (AV) node ablation. This procedure destroys the electrical pathway between the heart’s upper and lower chambers to prevent the chaotic signals from reaching the ventricles. This stops the rapid, irregular pulses but also means:
- The heart’s natural electrical connection is interrupted.
- The ventricles rely on an implanted pacemaker to maintain rhythm and rate.
This approach helps those who do not respond to medications or ablation focused on the atria, but they become completely dependent on their pacemaker for heartbeats.
Who Are the Ideal Candidates for a Pacemaker in AFib?
- AFib patients with persistent, symptomatic bradycardia not controllable by medication adjustments.
- Individuals with AFib and sinus node dysfunction causing problematic pauses or slow beats.
- Those who need AV node ablation for uncontrolled AFib and will require permanent pacing afterwards.
- Selected cases where rate control drugs cause dangerously slow heart rates, making it unsafe to continue without pacing support.
Most people with AFib do not automatically require a pacemaker. The decision depends on the specific symptoms, risk factors, and how the heart responds to treatment.
Potential Risks and Complications of Pacemaker Placement
While pacemaker surgery is generally safe, there are some risks and considerations, including:
- Infection at the site of implantation
- Bleeding or bruising
- Lead displacement: Movement of pacemaker wires from their optimal position
- Pneumothorax: Air leaking into the chest cavity causing lung collapse (rare)
- Device malfunction: Although uncommon, the pacemaker may require reprogramming or replacement
- Allergic reaction to device materials or medications used during implantation
Modern techniques have minimized these risks, but your medical team will monitor for potential complications both during and after the procedure.
What to Expect: Pacemaker Placement and Recovery
- Procedure: Usually involves local anesthesia and sedation; often completed in about 1–2 hours.
- Hospital Stay: Many patients can leave the hospital within 24 hours.
- Recovery: Most people resume normal activities within a week, but may need to avoid strenuous shoulder or arm movements on the side of the pacemaker for several weeks.
- Follow-up: Involves regular check-ups to monitor device function and battery life.
Alternatives and Other Treatments for AFib
Pacemakers do not address the underlying AFib itself in most cases—they simply manage slow heart rates or enable use of certain treatments. Other common AFib therapies include:
- Medication: Such as rate control drugs (beta-blockers, calcium channel blockers) and anti-arrhythmic medications.
- Electrical Cardioversion: Uses an electric shock under sedation to reset the heart to normal rhythm.
- Catheter Ablation: Destroys small heart tissue areas responsible for abnormal rhythms, with success rates of 70–80% especially in paroxysmal (occasional) AFib.
- AV Node Ablation: As described, often in conjunction with a pacemaker for complex cases.
- Blood Thinners: To reduce risk of stroke, which is higher with AFib due to pooling of blood in the atria.
Which treatment, or combination of treatments, is best depends on your symptoms, how well your heart is pumping, your lifestyle, and medical history.
Living With a Pacemaker
Most people with pacemakers lead full, active lives. However, carrying an implantable device does require certain precautions and regular follow-up care:
- Avoid magnetic fields and certain electrical devices that may interfere with the pacemaker (ask your doctor about specifics)
- Carry a pacemaker ID card at all times
- Inform all healthcare providers that you have a pacemaker
- Attend all scheduled follow-up appointments for device monitoring
With proper care and lifestyle modifications, most people adapt well to living with a pacemaker.
Frequently Asked Questions About Pacemakers in AFib
Is a pacemaker a cure for AFib?
No, a pacemaker does not cure atrial fibrillation. It helps manage certain heart rate-related complications that can occur with AFib, especially slow heart rates. The underlying AFib may persist, and you may still need other treatments for rhythm or stroke prevention.
What symptoms may indicate a need for a pacemaker in AFib?
Symptoms like persistent fatigue, dizziness, fainting, shortness of breath, or confusion—especially if related to slow heart rates—could suggest you may benefit from a pacemaker. Talk to your doctor for evaluation.
Can I use a microwave or cell phone if I have a pacemaker?
Modern pacemakers are shielded from most common household devices, including microwaves and cell phones. However, keep your phone at least six inches away from the device and consult your care provider about any specific electronic or magnetic risks.
Does having a pacemaker change physical activity?
Most routine activities, including exercise, are possible after recovery. However, avoid full-contact sports that could dislodge the device or leads, and follow your doctor’s instructions.
How long does a pacemaker last?
Pacemaker batteries typically last 5–15 years, depending on use and type. When the battery runs low, a minor surgical procedure replaces the device.
Summary Table: Comparing AFib Treatment Approaches
| Treatment | Main Purpose | AFib Cured? | Involves Surgery? | Note |
|---|---|---|---|---|
| Medications | Control heart rate and rhythm | No | No | Foundation therapy for most cases |
| Electrical Cardioversion | Restore normal rhythm | Sometimes | No (external procedure) | May require sedation |
| Catheter Ablation | Destroy tissue causing arrhythmia | Sometimes | Minimally invasive | Success rate up to 80% in select patients |
| AV Node Ablation + Pacemaker | Control ventricular rate | No (AFib persists) | Yes | Leads to pacemaker dependency |
| Pacemaker Alone | Prevent slow heart rates | No | Yes | Mainly for symptom relief, not AFib correction |
Key Takeaways
- Pacemakers are not a primary treatment for AFib itself, but may be necessary if you have additional rhythm issues—especially slow or irregular heart rates.
- AV node ablation makes a pacemaker necessary, as the heart relies on the device for beats after the procedure.
- Most people with AFib will try medications or ablation before considering a pacemaker.
- There are risks associated with pacemakers, but most people experience improvement in symptoms and quality of life.
- Open communication with your medical team is key to determining the best approach for managing your heart rhythm.
References
- https://www.healthline.com/health/heart/pacemaker-for-afib
- https://pubmed.ncbi.nlm.nih.gov/18061003/
- https://medmovie.com/topic/cvml_0413a/
- https://www.uchicagomedicine.org/conditions-services/heart-vascular/atrial-fibrillation/treatments
- https://www.melbourneheartrhythm.com.au/learn/procedures/14-av-node-ablation-and-pacing?showall=1
- https://www.webmd.com/heart-disease/atrial-fibrillation/pacemaker-afib
- https://iuhealth.org/thrive/living-with-afib-how-pacemakers-improve-quality-life
- https://www.heart.org/en/health-topics/atrial-fibrillation/treatment-and-prevention-of-atrial-fibrillation/surgical-procedures-for-afib
- https://afibinstitute.com.au/atrial-fibrillation-treatment-services/pacemakers/
- https://www.mayoclinic.org/tests-procedures/pacemaker/about/pac-20384689
Read full bio of Sneha Tete












