Overview of the Male Anatomy: Structure, Function, and Health
Explore the structural complexity of the male anatomy and its essential roles in health, wellness, and reproduction.
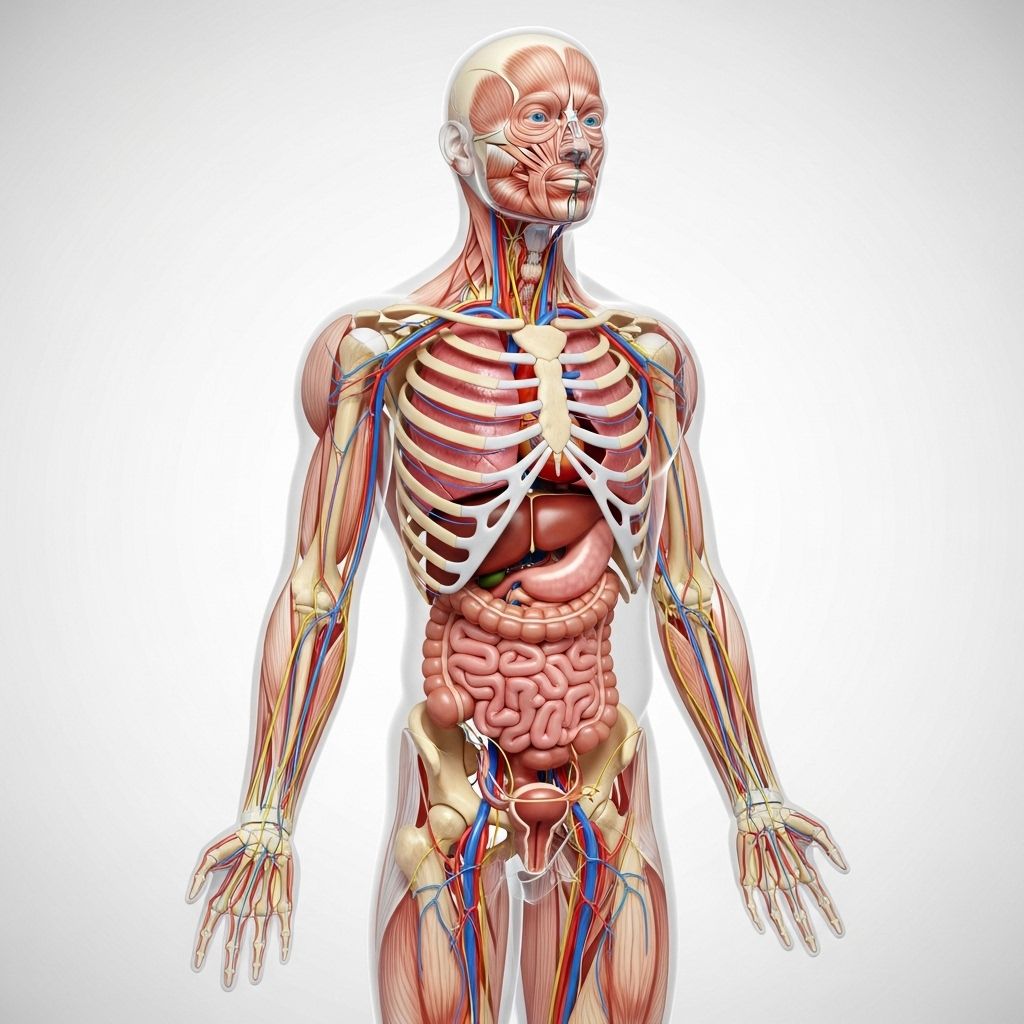
Overview of the Male Anatomy
The male anatomy is a complex network of organs and structures that support numerous functions essential for life and reproduction. From foundational building blocks like cells and tissues to specialized organs responsible for hormonal regulation, sexual function, and urinary health, understanding male anatomy is crucial to grasping overall male wellness and prevention strategies.
Core Components of the Male Anatomy
- External Genitalia: The penis and scrotum are the most visible parts and play major roles in sexual function and reproductive health.
- Internal Reproductive Organs: These include the testes, epididymis, vas deferens, seminal vesicles, and prostate gland.
- Urinary System: The bladder and urethra transport and expel urine.
- Hormonal Systems: The production, regulation, and function of male sex hormones like testosterone occur primarily within the testes.
The External Genitalia
The Penis
The penis serves dual functions: delivering urine out of the body and enabling sexual reproduction. Structurally, it contains three columns of erectile tissue: two corpora cavernosa and one corpus spongiosum. The corpus spongiosum surrounds the urethra and extends to form the glans penis, the sensitive tip. During sexual arousal, increased blood flow fills these tissues, causing an erection.
Key features of the penis include:
- Root: Attaches the penis to the body.
- Shaft: The elongated main portion.
- Glans: The rounded tip, often covered by foreskin unless circumcised.
- Urethral Opening: Located at the tip, provides a passage for urine and semen.
The Scrotum
The scrotum is a sac of skin and muscle that hangs below the penis and houses the testes. Its primary function is to regulate the temperature of the testes, ensuring an environment optimal for sperm production. Muscle fibers in the scrotum contract or relax in response to temperature changes, moving the testes closer to or further from the body.
The Internal Male Reproductive Organs
| Organ | Location | Core Function |
|---|---|---|
| Testes | Within the scrotum | Produce sperm and testosterone. |
| Epididymis | Curved atop the testes | Stores and matures sperm. |
| Vas deferens | Runs from the epididymis into the pelvic cavity | Transports sperm during ejaculation. |
| Seminal vesicles | Behind the bladder | Provide fluid that nourishes and helps sperm move. |
| Prostate gland | Below the bladder, encircling the urethra | Secretes fluid to protect and energize sperm. |
| Urethra | Runs through the penis | Passage for urine and semen out of the body. |
Testes
The testes are oval-shaped organs that make sperm and male hormones (androgens). Each testis is divided into lobules containing hundreds of seminiferous tubules where sperm develop. Testosterone, produced by specialized cells within the testes, shapes male physical traits and drives reproductive function.
Epididymis
Sperm mature and are stored in the epididymis, a tightly coiled tube attached to each testis. Here, sperm acquire motility and the ability to fertilize an egg. During ejaculation, sperm travel from the epididymis into the vas deferens.
Vas Deferens
Each vas deferens is a muscular tube that propels sperm up to the pelvic cavity, mixing them with fluids from accessory organs to form semen.
Seminal Vesicles and Prostate Gland
- Seminal Vesicles: These glands secrete a thick, alkaline fluid rich in sugar (fructose) to nourish sperm. The fluid also helps form the bulk of semen volume.
- Prostate Gland: The prostate adds a slightly milky, protective fluid as sperm pass through. This secretion supports sperm motility, longevity, and protection against the acidic vaginal environment.
Bulbourethral Glands (Cowper’s Glands)
Twin pea-sized glands below the prostate, the bulbourethral glands emit a small amount of lubricating fluid prior to ejaculation. This helps neutralize traces of urine in the urethra and prepares it for semen passage.
The Male Urinary System
The male urinary tract overlaps anatomically and functionally with the reproductive system. Major structures include:
- Bladder: Collects and stores urine.
- Urethra: Carries urine from the bladder through the penis and out of the body. During ejaculation, the flow of urine is temporarily blocked by muscular contractions to ensure only semen is expelled.
Hormonal Regulation and Function
Male anatomy is governed by complex hormonal controls that determine development and ongoing functions. The hypothalamus and pituitary gland in the brain initiate a cascade of signals that stimulate the testes to create testosterone and sperm.
- Testosterone: The primary male sex hormone, responsible for masculine features, muscle mass, voice deepening, and reproductive capacity.
- Luteinizing Hormone (LH): Promotes testosterone synthesis.
- Follicle-Stimulating Hormone (FSH): Stimulates sperm development.
Development of the Male Reproductive System
Male reproductive structures originate early in fetal life. Initially, embryos possess both male and female precursor organs. Around seven weeks gestation, genetic and hormonal signals (such as the presence of the SRY gene and androgen hormones) cause differentiation to the male phenotype. Testes produce hormones that shape external genitalia and drive internal organ formation.
Key developmental stages:
- Formation of testes and masculinization of the fetus driven by androgens.
- Descent of the testes from the abdominal cavity into the scrotum before birth.
- Rapid changes during puberty, including increased testosterone levels and initiation of sperm production (gonadarche).
Common Conditions Affecting the Male Anatomy
- Testicular Disorders: Includes torsion, cancer, and varicocele.
- Prostate Issues: Enlarged prostate (benign prostatic hyperplasia), prostate cancer, and prostatitis.
- Erectile Dysfunction: Difficulty achieving or maintaining an erection.
- Infertility: Problems with sperm production or motility.
- Urinary Tract Issues: Blockages or infections impacting urine flow.
Preventative Health and Wellness Strategies
- Regular physical exams and self-examination of the testes.
- Screens for prostate health in older men.
- Safe sexual practices to reduce risk of sexually transmitted infections.
- Healthy lifestyle choices: balanced diet, regular exercise, stress reduction.
- Prompt medical attention for pain, swelling, or dysfunction.
Frequently Asked Questions (FAQs)
Q: What is the function of the testes?
A: The testes produce sperm (for reproduction) and testosterone (for development of male traits and sexual function).
Q: How does puberty affect male anatomy?
A: Puberty triggers a surge in testosterone that leads to physical growth, deepened voice, increased muscle mass, development of body hair, and the start of sperm production.
Q: What is the prostate and why is it important?
A: The prostate is a gland below the bladder that adds vital protective and energizing fluids to semen, helping sperm survive the reproductive journey.
Q: How is male fertility affected by anatomy?
A: Healthy sperm production, proper duct function, and normal hormonal regulation are all necessary for fertility. Disorders or injuries in these areas can impact a man’s ability to father children.
Q: What self-care steps can men take for reproductive health?
A: Men should perform regular self-exams for lumps or changes in the testes, avoid risky behaviors, maintain a healthy lifestyle, and consult healthcare professionals for symptoms or concerns.
Glossary of Key Terms
- Androgen: A group of hormones including testosterone responsible for male traits and sexual development.
- Epididymis: Coiled tube where sperm mature and are stored.
- Gonadarche: Onset of reproductive maturation during puberty.
- Seminal Vesicles: Glands that supply nutrient-rich fluid for sperm.
- Spermatogenesis: The process of sperm cell production in the testes.
Summary Table: Male Anatomy Structure and Function
| Structure | Main Role | Location |
|---|---|---|
| Penis | Urination and sexual reproduction | External (above scrotum) |
| Scrotum | Protects and cools testes | External (below penis) |
| Testes | Sperm and testosterone production | Inside scrotum |
| Epididymis | Maturation/storage of sperm | Attached to testes |
| Vas deferens | Transports sperm | Pelvic cavity |
| Seminal vesicles | Nourishes sperm | Behind bladder |
| Prostate gland | Protective fluid for sperm | Beneath bladder |
| Urethra | Urine and semen passage | Runs through penis |
| Bladder | Stores urine | Pelvic cavity |
References
- Adapted and synthesized from Johns Hopkins Medicine, clinical urologic endocrinology, and functional anatomy sources.
References
- https://pure.johnshopkins.edu/en/publications/development-of-the-male-reproductive-system-3
- https://www.press.jhu.edu/books/title/2679/johns-hopkins-atlas-human-functional-anatomy
- https://www.youtube.com/playlist?list=PLn_zZfPdMwpJU99g3CCAkDXOmH1aIDe_g
- https://profiles.nlm.nih.gov/spotlight/gf/feature/father-of-modern-medicine-the-johns-hopkins-school-of-medicine-1889-1905
Read full bio of Sneha Tete












