Outlook for IgA Nephropathy: Understanding Prognosis and Management
Discover the progression, prognosis, complications, and treatment options for IgA nephropathy—a common kidney disease affecting people worldwide.
Outlook for IgA Nephropathy
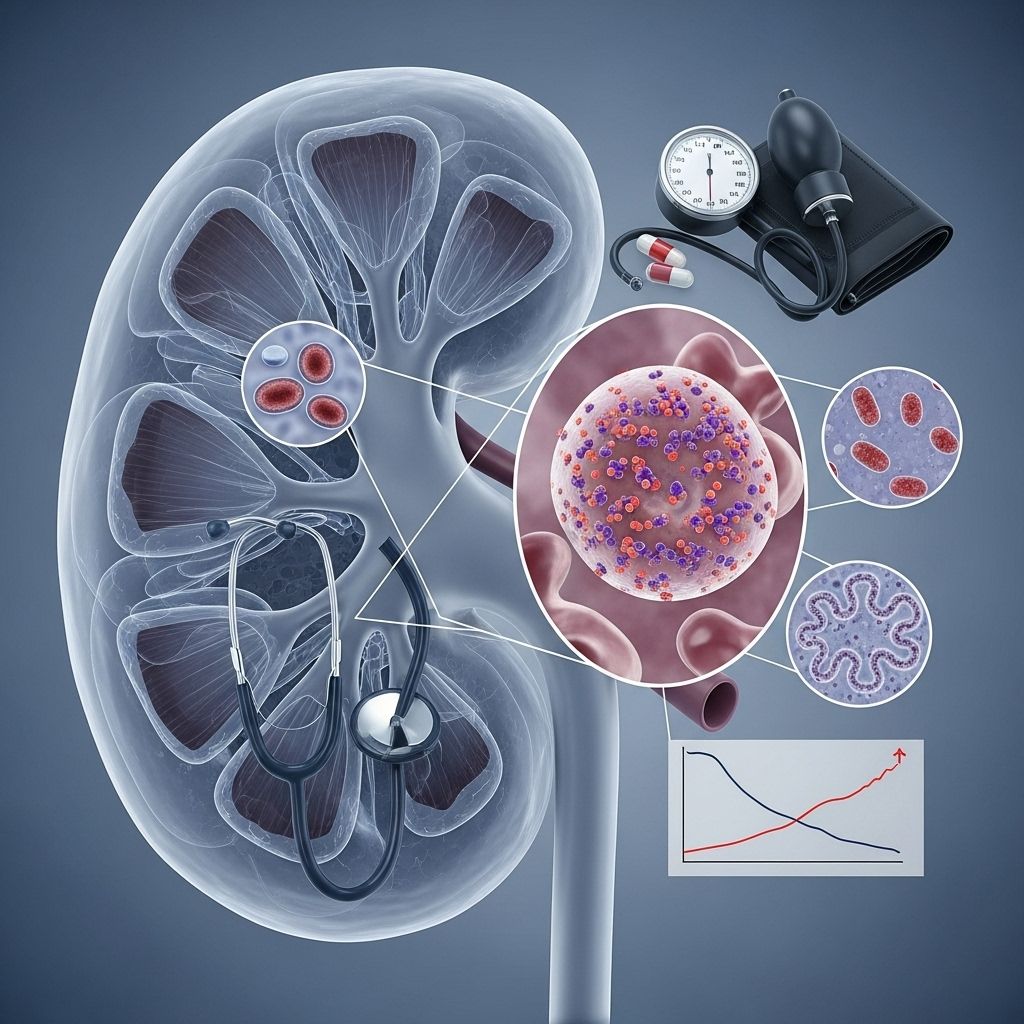
IgA nephropathy—also known as Berger’s disease—is a common autoimmune kidney disorder that can significantly affect long-term health. Understanding its progression, risk factors for severity, potential complications, and strategies for management is crucial for patients and their families.
What is IgA Nephropathy?
IgA nephropathy (IgAN) occurs when immunoglobulin A (IgA) antibodies cluster in the kidneys’ filtering units (glomeruli), triggering inflammation and damage. Over time, this can impair kidney function, leading to chronic kidney disease or even kidney failure. The disease primarily affects young adults, but it can develop at any age. Alternate names include Berger’s disease, after its discoverer, Dr. Jean Berger.
- Autoimmune condition: The body’s immune cells produce abnormal IgA that accumulates in kidneys.
- Glomeruli damage: Leads to leakage of blood and proteins into urine.
- Primary cause: Exact triggers remain unclear; genetic and environmental influences are involved.
How Common Is IgA Nephropathy?
It is among the most frequent causes of glomerular kidney disease worldwide.
- In the US, it’s found in about 1 in 10 kidney biopsies.
- Higher rates are seen in East Asia and parts of Europe.
- The worldwide incidence is at least 2.5 per 100,000 population.
Who Is Most at Risk?
- Ages 10 to 40: Most commonly diagnosed in younger adults.
- Men: Male patients are at higher risk.
- Ethnicity: East Asian and white European ancestry have increased prevalence.
- Family history: Those with relatives affected by IgAN or IgA vasculitis are more likely to develop the disease.
- Associated conditions: Celiac disease, hepatitis, cirrhosis, and HIV increase risk.
Symptoms and Early Detection
Many individuals experience no symptoms initially. IgA nephropathy is often detected by chance during routine urine or blood tests. Common findings and symptoms include:
- Blood in urine (hematuria): May be visible or microscopic. Sometimes occurs during sore throat episodes or after exercise.
- Proteinuria: Protein detected in urine via laboratory testing.
- High blood pressure (hypertension): Often a late sign reflective of kidney impairment.
- Elevated creatinine levels: Indicate decreased kidney efficiency.
- Swelling (edema): Especially in legs or around eyes, due to salt and fluid retention.
- Flank pain: May be present in some cases.
Long-Term Outlook for IgA Nephropathy
The progression of IgA nephropathy varies widely:
- Some people enjoy many years of stable kidney function with little impact on daily life.
- Others experience a gradual decline, progressing to chronic kidney disease (CKD) or end-stage kidney disease (ESKD) requiring dialysis or transplant.
| Possible Outcome | Description | Prevalence |
|---|---|---|
| Stable Kidney Function | No notable disease progression over years; normal life expectancy. | ~50% |
| Mild Decrease in Function | Slow decline; manageable, may need medication; few complications. | ~20% |
| Kidney Failure | Significant decline, often over 10–20 years; requires dialysis or transplant. | ~30% |
What Factors Affect Prognosis?
The risk of progression and severity depends on several factors:
- Amount of protein in urine: Higher levels correlate with worse outcomes.
- Persistent high blood pressure: Uncontrolled hypertension accelerates kidney damage.
- Kidney function at diagnosis: Lower filtration rates (GFR) suggest more advanced disease.
- Age and sex: Younger patients and males have increased risk of progression.
- Genetics and family history: May predispose to more severe forms.
- Other chronic health conditions: Diabetes and heart disease worsen outcomes.
- Lifestyle factors: Smoking and poor diet may contribute to progression.
Complications of IgA Nephropathy
Potential complications include:
- Chronic kidney disease: Gradual loss of function over time, sometimes leading to dialysis.
- Nephrotic syndrome: High urine protein, low blood protein, and abnormal lipid levels create additional cardiovascular risks.
- High blood pressure: Can further damage kidneys, increasing the risk of heart attack and stroke.
- End-stage kidney disease: Complete loss of kidney function, requiring intensive treatment.
How Is IgA Nephropathy Diagnosed?
- Urine tests: Detect blood and protein leaks.
- Blood tests: Monitor kidney filtration and waste products (creatinine).
- Kidney biopsy: The only definitive diagnostic test, visualizing IgA deposits in glomeruli.
Treatment and Management Options
Treatment goals center on slowing disease progression and managing symptoms:
- Blood pressure control: Medications—often ACE inhibitors or angiotensin receptor blockers (ARBs)—are critical to protect kidney function.
- Proteinuria reduction: Lowering how much protein leaks into urine is a key therapeutic endpoint.
- Corticosteroids: Sometimes used to reduce immune system activity.
- New therapies: Sodium-glucose cotransporter 2 (SGLT2) inhibitors and endothelin receptor antagonists are recent additions targeting the root pathogenesis.
- General kidney health:
- Low-sodium diets
- Managing cholesterol
- Maintaining healthy weight and regular exercise
- Advanced disease: Dialysis and transplantation may be necessary if kidneys fail.
Living with IgA Nephropathy: Quality of Life and Monitoring
- Regular medical follow-up: Patients need periodic lab tests and blood-pressure monitoring to detect any changes promptly.
- Self-care: Healthy diet, exercise, controlling blood pressure, and avoiding smoking are key.
- Psychosocial support: Chronic illness can impact mental health—counseling and peer support are recommended.
- Early intervention: Seeking medical advice for new symptoms (swelling, blood in urine, high BP) can prevent complications.
Frequently Asked Questions (FAQs)
Q: Is IgA nephropathy curable?
A: There is no cure at present. Treatment aims to slow progression and reduce complications.
Q: How fast does IgA nephropathy progress?
A: Progression varies widely. Many experience slow progression over years, but some may develop kidney failure within a decade.
Q: Can changes in lifestyle make a difference?
A: Yes. Controlling blood pressure, avoiding excess salt, and exercise help preserve kidney function.
Q: What are the signs that IgA nephropathy is worsening?
A: Increasing urine protein levels, rising blood pressure, swelling, and higher creatinine levels may signal disease advancement.
Q: Is genetic testing available?
A: There is currently no widely available genetic test for IgA nephropathy, though research continues in this area.
Summary Table: Key Facts about IgA Nephropathy
| Feature | Detail |
|---|---|
| Type of Disease | Autoimmune, chronic kidney disorder |
| Main Symptoms | Blood/protein in urine, high blood pressure, swelling |
| Diagnosis | Kidney biopsy (definitive), urine and blood tests |
| Major Complications | Chronic kidney disease, nephrotic syndrome, ESKD |
| Treatment | Blood pressure meds, proteinuria reduction, newer targeted therapies |
| Prognosis | Varies widely; ~30% progress to kidney failure |
Conclusion
IgA nephropathy is a variable, chronic kidney disease that may be stable for years or progress to kidney failure. Individual outlook depends on several risk factors, but advances in treatment are improving patient outcomes. Proactive management, healthy living, and regular monitoring are the foundation of a positive prognosis.
References
- https://www.kidneyresearchuk.org/conditions-symptoms/iga-nephropathy/
- https://my.clevelandclinic.org/health/diseases/5990-iga-nephropathy
- https://www.ccjm.org/content/92/6/373
- https://www.niddk.nih.gov/health-information/kidney-disease/iga-nephropathy
- https://www.kidney.org/kidney-topics/iga-nephropathy
- https://www.ncbi.nlm.nih.gov/books/NBK538214/
Read full bio of Sneha Tete












